Abstract
BACKGROUND AND AIMS—Barrett's oesophagus is associated with an increased risk of cancer. As dysplasia is not visible during routine endoscopy, random biopsies in the four quadrants every 1-2 cm are recommended. Endoscopic fluorescence detection (EFD) after sensitisation with 5-aminolaevulinic acid (5-ALA) with different modes and concentrations was assessed to optimise the technique for detection of dysplasia or early cancers. 5-ALA is converted intracellularly to protoporphyrin IX which accumulates in malignant tissue and can be detected by typical red fluorescence after illumination with blue light. METHODS—In 47 patients with Barrett's oesophagus, 10 with known dysplasia, 58 fluorescence endoscopies were performed after sensitisation with different concentrations of 5-ALA given orally (5, 10, 20, 30 mg/kg) or locally (500-1000 mg) by spraying the mucosa via a catheter. EFD was performed 4-6 hours after systemic and 1-2 hours after local sensitisation using a special light source delivering white or blue light. A total of 243 biopsies of red fluorescent (n=113) and non-fluorescent areas (n=130) were taken. RESULTS—In three patients, two early cancers and dysplasia, not visible during routine endoscopy, were detected by EFD. Thirty three biopsies revealed either low or high grade dysplasia. Sensitivity for detection of dysplastic lesions ranged from 60% after local sensitisation with 500 mg to 80%, 100%, and 100% after systemic application of 5-ALA 10, 20, and 30 mg/kg, respectively. However, specificity was best for local sensitisation (70%) while systemic administration revealed values between 27% and 56%. Using 5 mg/kg, no red fluorescence in dysplastic lesions was found. No severe side effects were noted. CONCLUSION—EFD is a promising tool to detect non-visible dysplastic lesions in Barrett's oesophagus using 5-ALA sensitisation. A randomised controlled study is now indicated to compare the efficacy of EFD with the standard technique of four quadrant random biopsies. Keywords: Barrett's oesophagus; dysplasia; fluorescence endoscopy; 5-aminolaevulinic acid
Full Text
The Full Text of this article is available as a PDF (180.1 KB).
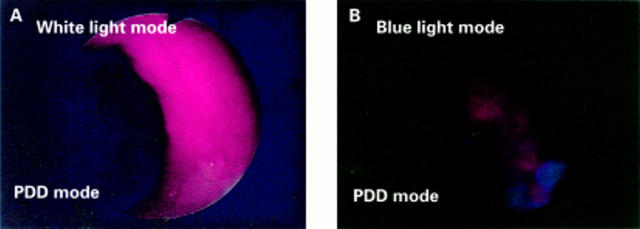
Figure 1 .
Endoscopic fluorescence pictures. Comparative presentation of regular endoscopy with white light (A) and fluorescence endoscopy (B), four hours after sensitisation with 20 mg/kg 5-aminolaevulinic acid. Selective red fluorescence area within the Barrett's segment presented high grade dysplasia.
Figure 2 .
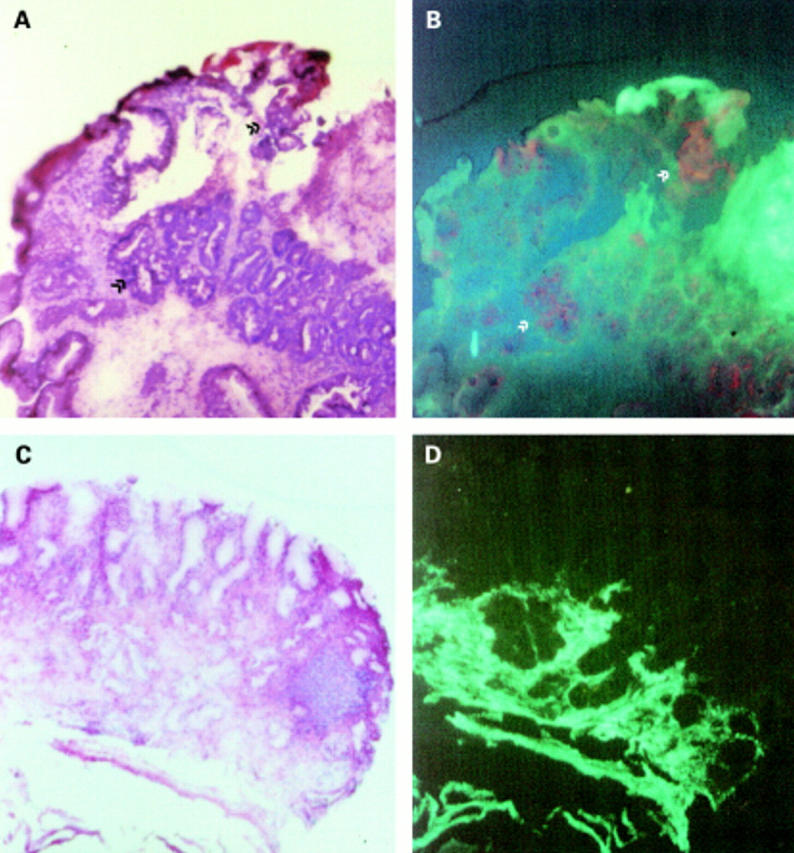
Fluorescence microscopy. (A, B) Frozen section (20 µm) from a biopsy of endoscopically red fluorescent positive mucosa in Barrett's oesophagus. (A) Fluorescence of the section and subsequent haematoxylin-eosin stained identical section (B). Enlargement 25×. Fluorescence was limited to the epithelium, mature foveolar epithelium was negative (left side, surface), and distinct and patchy positive fluorescence was related to intestinal metaplasia (specialised epithelium with goblet cells) and to dysplasia (arrows). (C, D) Frozen section (20 µm) from a biopsy of endoscopically red fluorescent negative mucosa in Barrett's oesophagus. (C) Fluorescence of section indicating only green autofluorescence, and subsequently haematoxylin-eosin stained identical section (D), showing the histology of the gastric mucosa (simple metaplasia). Enlargement 25×. Comment: diagnosis was verified by adjacent regular 5 µm sections but identical 20 µm sections are shown here to precisely relate fluorescence to morphology.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bjorkman D. J., Samowitz W. S., Brigham E. J., Peterson B. J., Straight R. C. Fluorescence localization of early colonic cancer in the rat by hematoporphyrin derivative. Lasers Surg Med. 1991;11(3):263–270. doi: 10.1002/lsm.1900110310. [DOI] [PubMed] [Google Scholar]
- Drewitz D. J., Sampliner R. E., Garewal H. S. The incidence of adenocarcinoma in Barrett's esophagus: a prospective study of 170 patients followed 4.8 years. Am J Gastroenterol. 1997 Feb;92(2):212–215. [PubMed] [Google Scholar]
- Eker C., Montán S., Jaramillo E., Koizumi K., Rubio C., Andersson-Engels S., Svanberg K., Svanberg S., Slezak P. Clinical spectral characterisation of colonic mucosal lesions using autofluorescence and delta aminolevulinic acid sensitisation. Gut. 1999 Apr;44(4):511–518. doi: 10.1136/gut.44.4.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk G. W., Rice T. W., Goldblum J. R., Richter J. E. Jumbo biopsy forceps protocol still misses unsuspected cancer in Barrett's esophagus with high-grade dysplasia. Gastrointest Endosc. 1999 Feb;49(2):170–176. doi: 10.1016/s0016-5107(99)70482-7. [DOI] [PubMed] [Google Scholar]
- Hameeteman W., Tytgat G. N., Houthoff H. J., van den Tweel J. G. Barrett's esophagus: development of dysplasia and adenocarcinoma. Gastroenterology. 1989 May;96(5 Pt 1):1249–1256. doi: 10.1016/s0016-5085(89)80011-3. [DOI] [PubMed] [Google Scholar]
- Levine D. S., Haggitt R. C., Blount P. L., Rabinovitch P. S., Rusch V. W., Reid B. J. An endoscopic biopsy protocol can differentiate high-grade dysplasia from early adenocarcinoma in Barrett's esophagus. Gastroenterology. 1993 Jul;105(1):40–50. doi: 10.1016/0016-5085(93)90008-z. [DOI] [PubMed] [Google Scholar]
- McArdle J. E., Lewin K. J., Randall G., Weinstein W. Distribution of dysplasias and early invasive carcinoma in Barrett's esophagus. Hum Pathol. 1992 May;23(5):479–482. doi: 10.1016/0046-8177(92)90123-k. [DOI] [PubMed] [Google Scholar]
- Messmann H., Knüchel R., Bäumler W., Holstege A., Schölmerich J. Endoscopic fluorescence detection of dysplasia in patients with Barrett's esophagus, ulcerative colitis, or adenomatous polyps after 5-aminolevulinic acid-induced protoporphyrin IX sensitization. Gastrointest Endosc. 1999 Jan;49(1):97–101. doi: 10.1016/s0016-5107(99)70453-0. [DOI] [PubMed] [Google Scholar]
- Messmann H., Kullmann F., Wild T., Knüchel-Clarke R., Rüschoff J., Gross V., Schölmerich J., Holstege A. Detection of dysplastic lesions by fluorescence in a model of colitis in rats after previous photosensitization with 5-aminolaevulinic acid. Endoscopy. 1998 May;30(4):333–338. doi: 10.1055/s-2007-1001278. [DOI] [PubMed] [Google Scholar]
- Messmann H., Szeimies R. M., Bäumler W., Knüchel R., Zirngibl H., Schölmerich J., Holstege A. Enhanced effectiveness of photodynamic therapy with laser light fractionation in patients with esophageal cancer. Endoscopy. 1997 May;29(4):275–280. doi: 10.1055/s-2007-1004189. [DOI] [PubMed] [Google Scholar]
- Panjehpour M., Overholt B. F., Vo-Dinh T., Haggitt R. C., Edwards D. H., Buckley F. P., 3rd Endoscopic fluorescence detection of high-grade dysplasia in Barrett's esophagus. Gastroenterology. 1996 Jul;111(1):93–101. doi: 10.1053/gast.1996.v111.pm8698231. [DOI] [PubMed] [Google Scholar]
- Peng Q., Warloe T., Berg K., Moan J., Kongshaug M., Giercksky K. E., Nesland J. M. 5-Aminolevulinic acid-based photodynamic therapy. Clinical research and future challenges. Cancer. 1997 Jun 15;79(12):2282–2308. doi: 10.1002/(sici)1097-0142(19970615)79:12<2282::aid-cncr2>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Regula J., MacRobert A. J., Gorchein A., Buonaccorsi G. A., Thorpe S. M., Spencer G. M., Hatfield A. R., Bown S. G. Photosensitisation and photodynamic therapy of oesophageal, duodenal, and colorectal tumours using 5 aminolaevulinic acid induced protoporphyrin IX--a pilot study. Gut. 1995 Jan;36(1):67–75. doi: 10.1136/gut.36.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampliner R. E. Practice guidelines on the diagnosis, surveillance, and therapy of Barrett's esophagus. The Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1998 Jul;93(7):1028–1032. doi: 10.1111/j.1572-0241.1998.00362.x. [DOI] [PubMed] [Google Scholar]
- Spechler S. J. Endoscopic surveillance for patients with Barrett esophagus: does the cancer risk justify the practice? Ann Intern Med. 1987 Jun;106(6):902–904. doi: 10.7326/0003-4819-106-6-902. [DOI] [PubMed] [Google Scholar]
- Steinbach P., Weingandt H., Baumgartner R., Kriegmair M., Hofstädter F., Knüchel R. Cellular fluorescence of the endogenous photosensitizer protoporphyrin IX following exposure to 5-aminolevulinic acid. Photochem Photobiol. 1995 Nov;62(5):887–895. doi: 10.1111/j.1751-1097.1995.tb09152.x. [DOI] [PubMed] [Google Scholar]
- von Holstein C. S., Nilsson A. M., Andersson-Engels S., Willén R., Walther B., Svanberg K. Detection of adenocarcinoma in Barrett's oesophagus by means of laser induced fluorescence. Gut. 1996 Nov;39(5):711–716. doi: 10.1136/gut.39.5.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Rueden D. G., McBrearty F. X., Clements B. M., Woratyla S. Photo detection of carcinoma of the colon in a rat model: a pilot study. J Surg Oncol. 1993 May;53(1):43–46. doi: 10.1002/jso.2930530112. [DOI] [PubMed] [Google Scholar]