Abstract
BACKGROUND/AIMS—Cryptogenetic multifocal ulcerous stenosing enteritis (CMUSE) is a rare disease whose origin is unknown. The aim of this study was to describe the clinical spectrum of CMUSE, to determine the origin and pathophysiology of the disease, and to propose a treatment strategy. METHODS—A total of 220 French gastroenterology departments were contacted to review patients with unexplained small bowel strictures. Of 17 responses, 12 corresponded to a diagnosis of CMUSE. These patients were hospitalised between 1965 and 1993 and their medical records were reviewed. RESULTS—All patients (mean age 42.1 (4.4) years) had intestinal and five had extraintestinal symptoms (peripheral neuropathy, buccal aphthae, sicca syndrome, polyarthralgia, Raynaud's phenomenon, arterial hypertension). One patient had heterozygous type I C2 deficiency (28 base pair gene deletion). Two to 25 (mean 8.3 (1.9)) small intestine strictures were found. Stenoses of the large jejunoileal arteries were observed on two and aneurysms on three of five mesenteric angiograms. Despite surgery, symptoms recurred in seven of 10 patients and strictures in four. Steroid therapy was effective but caused dependence. One untreated patient died. Small bowel pathology showed superficial ulceration of the mucosae and submucosae, and an inflammatory infiltrate made of neutrophils and eosinophils. CONCLUSIONS—CMUSE is an independent entity characterised by steroid sensitive inflammation of the small bowel which often recurs after surgery. CMUSE may be related to a particular form of polyarteritis nodosa with mainly intestinal expression or with an as yet unclassified vasculitis. Keywords: cryptogenetic multifocal ulcerous stenosing enteritis; vasculitis; small intestine
Full Text
The Full Text of this article is available as a PDF (145.1 KB).
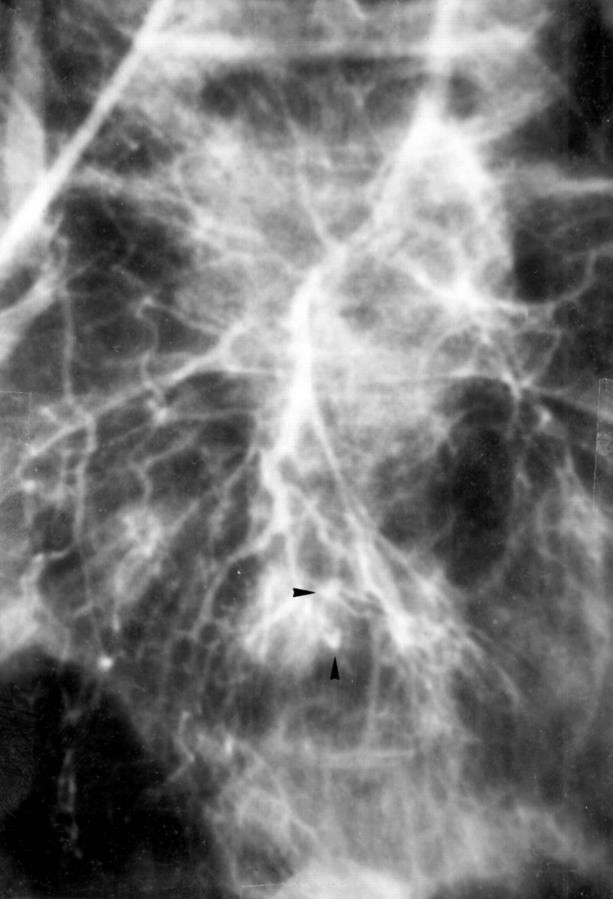
Figure 1 .
Superior mesenteric artery. Selective conventional angiography; arterial phase showing aneurysms of the distal jejunal arteries (arrowheads).
Figure 2 .
Longitudinal section of the resected small bowel through the strictures.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Agnello V. Complement deficiency states. Medicine (Baltimore) 1978 Jan;57(1):1–23. doi: 10.1097/00005792-197801000-00001. [DOI] [PubMed] [Google Scholar]
- Baer A. N., Bayless T. M., Yardley J. H. Intestinal ulceration and malabsorption syndromes. Gastroenterology. 1980 Oct;79(4):754–765. [PubMed] [Google Scholar]
- Brahme F., Hildell J. Angiography in Crohn's disease revisited. AJR Am J Roentgenol. 1976 May;126(5):941–951. doi: 10.2214/ajr.126.5.941. [DOI] [PubMed] [Google Scholar]
- Camilleri M., Pusey C. D., Chadwick V. S., Rees A. J. Gastrointestinal manifestations of systemic vasculitis. Q J Med. 1983 Spring;52(206):141–149. [PubMed] [Google Scholar]
- Chagnon J. P., Devars du Mayne J. F., Marche C., Vissuzaine C., Cerf M. L'entérite sténosante multifocale cryptogénétique: une entité autonome? Gastroenterol Clin Biol. 1984 Nov;8(11):808–813. [PubMed] [Google Scholar]
- DEBRAY C., BESANCON F., HARDOUIN J. P., MARTIN E., MARCHE C., KHOURY K. ENT'ERITE ST'ENOSANTE ULC'EREUSE PLURIFOCALE CRYPTOG'EN'ETIQUE. Arch Mal Appar Dig Mal Nutr. 1964 Mar;53:193–206. [PubMed] [Google Scholar]
- Doutre L. P., Paccalin J., Périssat J., Traissac F. J. Entérite ténosante ulcéreuse plurifocale. Une nouvelle observation. Arch Fr Mal App Dig. 1966 Jun;55(6):537–540. [PubMed] [Google Scholar]
- Fauci A. S., Haynes B., Katz P. The spectrum of vasculitis: clinical, pathologic, immunologic and therapeutic considerations. Ann Intern Med. 1978 Nov;89(5 Pt 1):660–676. doi: 10.7326/0003-4819-89-5-660. [DOI] [PubMed] [Google Scholar]
- Gauthier A. P., Rampal M., Lieutaud R., Sarles H. Sténoses multiples "idiopathiques" de l'intestin grêle. A propos de deux observations. Arch Fr Mal App Dig. 1966 Jan-Feb;55(1):31–43. [PubMed] [Google Scholar]
- Hekali P., Kajander H., Pajari R., Stenman S., Somer T. Diagnostic significance of angiographically observed visceral aneurysms with regard to polyarteritis nodosa. Acta Radiol. 1991 Mar;32(2):143–148. [PubMed] [Google Scholar]
- Jeffries G. H., Steinberg H., Sleisenger M. H. Chronic ulcerative (nongranulomatous) jejunitis. Am J Med. 1968 Jan;44(1):47–59. doi: 10.1016/0002-9343(68)90236-2. [DOI] [PubMed] [Google Scholar]
- Jennette J. C., Falk R. J., Andrassy K., Bacon P. A., Churg J., Gross W. L., Hagen E. C., Hoffman G. S., Hunder G. G., Kallenberg C. G. Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum. 1994 Feb;37(2):187–192. doi: 10.1002/art.1780370206. [DOI] [PubMed] [Google Scholar]
- Johnson C. A., Densen P., Hurford R. K., Jr, Colten H. R., Wetsel R. A. Type I human complement C2 deficiency. A 28-base pair gene deletion causes skipping of exon 6 during RNA splicing. J Biol Chem. 1992 May 5;267(13):9347–9353. [PubMed] [Google Scholar]
- Kuehne S. E., Gauvin G. P., Shortsleeve M. J. Small bowel stricture caused by rheumatoid vasculitis. Radiology. 1992 Jul;184(1):215–216. doi: 10.1148/radiology.184.1.1609082. [DOI] [PubMed] [Google Scholar]
- Lang J., Price A. B., Levi A. J., Burke M., Gumpel J. M., Bjarnason I. Diaphragm disease: pathology of disease of the small intestine induced by non-steroidal anti-inflammatory drugs. J Clin Pathol. 1988 May;41(5):516–526. doi: 10.1136/jcp.41.5.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lescut J., Grégoire L., Weisemburger J. P. Stenoses multiples cryptogenetiques de l'intestin grele. Lille Med. 1969;14(5):602–607. [PubMed] [Google Scholar]
- Lie J. T. The Canadian Rheumatism Association, 1991 Dunlop-Dottridge Lecture. Vasculitis, 1815 to 1991: classification and diagnostic specificity. J Rheumatol. 1992 Jan;19(1):83–89. [PubMed] [Google Scholar]
- Lightfoot R. W., Jr, Michel B. A., Bloch D. A., Hunder G. G., Zvaifler N. J., McShane D. J., Arend W. P., Calabrese L. H., Leavitt R. Y., Lie J. T. The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum. 1990 Aug;33(8):1088–1093. doi: 10.1002/art.1780330805. [DOI] [PubMed] [Google Scholar]
- Lopez L. R., Schocket A. L., Stanford R. E., Claman H. N., Kohler P. F. Gastrointestinal involvement in leukocytoclastic vasculitis and polyarteritis nodosa. J Rheumatol. 1980 Sep-Oct;7(5):677–684. [PubMed] [Google Scholar]
- Macinot C., Lorenzini C. L., Ravey M., Mauvary G., Rauber G. Entérite segmentaire sténosante multifocale. Sem Hop. 1974 Oct 14;50(41):2518–2520. [PubMed] [Google Scholar]
- McCauley R. L., Johnston M. R., Fauci A. S. Surgical aspects of systemic necrotizing vasculitis. Surgery. 1985 Jan;97(1):104–110. [PubMed] [Google Scholar]
- Mills P. R., Brown I. L., Watkinson G. Idiopathic chronic ulcerative enteritis. Report of five cases and review of the literature. Q J Med. 1980 Spring;49(194):133–149. [PubMed] [Google Scholar]
- Perlemuter G., Chaussade S., Soubrane O., Degoy A., Louvel A., Barbet P., Legman P., Kahan A., Weiss L., Couturier D. Multifocal stenosing ulcerations of the small intestine revealing vasculitis associated with C2 deficiency. Gastroenterology. 1996 May;110(5):1628–1632. doi: 10.1053/gast.1996.v110.pm8613071. [DOI] [PubMed] [Google Scholar]
- ROCHA A., ARTIGAS V. [Stenosing ulcerous disease of the jejuno-ileum]. Arch Mal Appar Dig Mal Nutr. 1959 Oct;48:1230–1236. [PubMed] [Google Scholar]
- Ruan E. A., Komorowski R. A., Hogan W. J., Soergel K. H. Nongranulomatous chronic idiopathic enterocolitis: clinicopathologic profile and response to corticosteroids. Gastroenterology. 1996 Sep;111(3):629–637. doi: 10.1053/gast.1996.v111.pm8780567. [DOI] [PubMed] [Google Scholar]
- SHOESMITH J. H., TATE G. T., WRIGHT C. J. MULTIPLE STRICTURES OF THE JEJUNUM. Gut. 1964 Apr;5:132–135. doi: 10.1136/gut.5.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schölmerich J., Schmidt E., Schümichen C., Billmann P., Schmidt H., Gerok W. Scintigraphic assessment of bowel involvement and disease activity in Crohn's disease using technetium 99m-hexamethyl propylene amine oxine as leukocyte label. Gastroenterology. 1988 Nov;95(5):1287–1293. doi: 10.1016/0016-5085(88)90363-0. [DOI] [PubMed] [Google Scholar]
- Tandon H. D., Prakash A. Pathology of intestinal tuberculosis and its distinction from Crohn's disease. Gut. 1972 Apr;13(4):260–269. doi: 10.1136/gut.13.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield A. J., Sawyerr A. M., Dhillon A. P., Pittilo R. M., Rowles P. M., Lewis A. A., Pounder R. E. Pathogenesis of Crohn's disease: multifocal gastrointestinal infarction. Lancet. 1989 Nov 4;2(8671):1057–1062. doi: 10.1016/s0140-6736(89)91078-7. [DOI] [PubMed] [Google Scholar]
- Williams D. H., Kratka C. D., Bonafede J. P., Katon R. M. Polyarteritis nodosa of the gastrointestinal tract with endoscopically documented duodenal and jejunal ulceration. Gastrointest Endosc. 1992 Jul-Aug;38(4):501–503. doi: 10.1016/s0016-5107(92)70487-8. [DOI] [PubMed] [Google Scholar]
- Williams D. H., Kratka C. D., Bonafede J. P., Katon R. M. Polyarteritis nodosa of the gastrointestinal tract with endoscopically documented duodenal and jejunal ulceration. Gastrointest Endosc. 1992 Jul-Aug;38(4):501–503. doi: 10.1016/s0016-5107(92)70487-8. [DOI] [PubMed] [Google Scholar]