Abstract
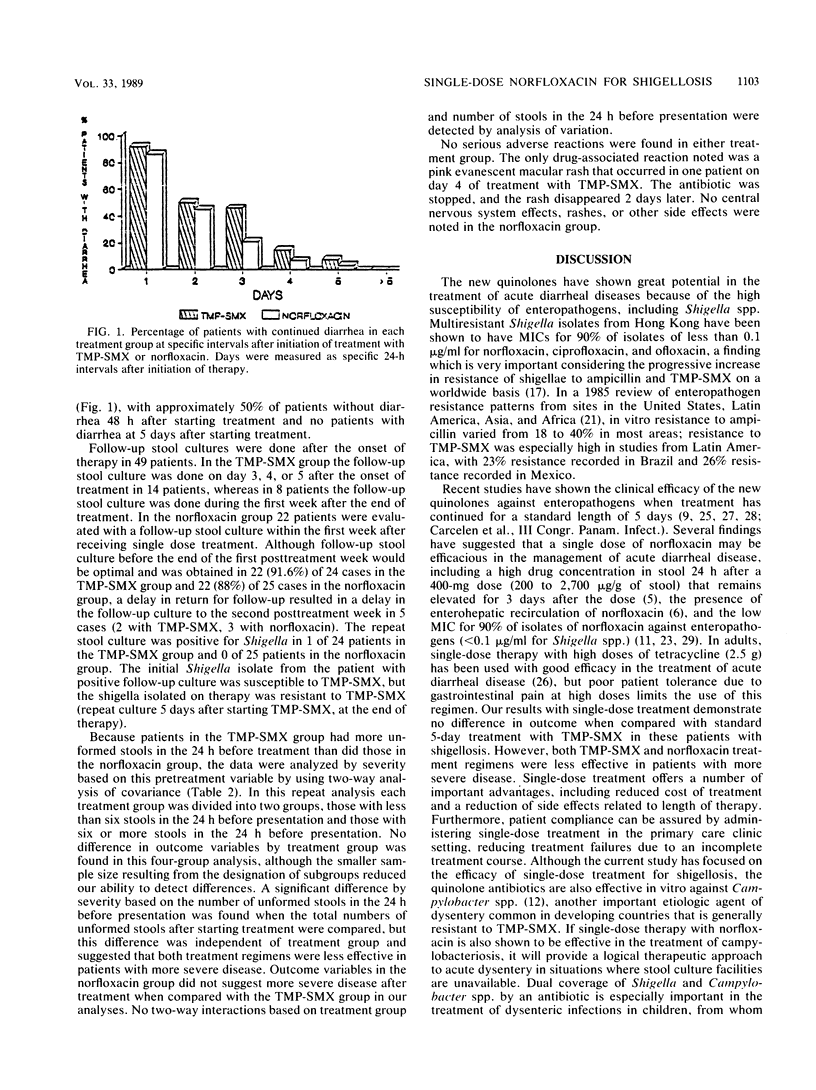
Shigellae have been shown to be highly susceptible to new quinolone agents, with average MICs for 90% of isolates of less than 0.1 microgram/ml. Because these agents also reach high concentrations in the stool after a single dose, the effectiveness of a single 800-mg dose of norfloxacin and of 5-day treatment with trimethoprim-sulfamethoxazole (TMP-SMX) were compared in a randomized trial. Patients with clinical dysentery received one of these treatment regimens, and clinical data and follow-up culture results were analyzed for patients whose stool culture on presentation grew shigellae. When 55 patients with shigellosis (26 treated with TMP-SMX, 29 treated with norfloxacin) whose bacterial isolates were susceptible to the antibiotic given were compared by treatment group, no significant differences were seen in days of illness (mean, 2.5 +/- 0.65 days with TMP-SMX and 2.0 +/- 0.47 days with norfloxacin; P = 0.200) or number of unformed stools after starting treatment (mean, 9.7 +/- 2.37 stools with TMP-SMX and 7.6 +/- 3.19 stools with norfloxacin; P = 0.312). Resistance in vitro to TMP-SMX was seen in 15% of Shigella isolates, whereas none was resistant to norfloxacin. Bacteriologic failure was found in 1 patient among 24 receiving TMP-SMX and in none of 25 patients receiving norfloxacin. One single dose of norfloxacin was as effective as 5 days of treatment with TMP-SMX in these adults with shigellosis.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alfaham M., Holt M. E., Goodchild M. C. Arthropathy in a patient with cystic fibrosis taking ciprofloxacin. Br Med J (Clin Res Ed) 1987 Sep 19;295(6600):699–699. doi: 10.1136/bmj.295.6600.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHEEVER F. S. The treatment of shigellosis with antibiotics. Ann N Y Acad Sci. 1952 Dec 30;55(6):1063–1069. doi: 10.1111/j.1749-6632.1952.tb22666.x. [DOI] [PubMed] [Google Scholar]
- Carlson J. R., Thornton S. A., DuPont H. L., West A. H., Mathewson J. J. Comparative in vitro activities of ten antimicrobial agents against bacterial enteropathogens. Antimicrob Agents Chemother. 1983 Oct;24(4):509–513. doi: 10.1128/aac.24.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cofsky R. D., duBouchet L., Landesman S. H. Recovery of norfloxacin in feces after administration of a single oral dose to human volunteers. Antimicrob Agents Chemother. 1984 Jul;26(1):110–111. doi: 10.1128/aac.26.1.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohue-Rolfe A., Keusch G. T., Edson C., Thorley-Lawson D., Jacewicz M. Pathogenesis of Shigella diarrhea. IX. Simplified high yield purification of Shigella toxin and characterization of subunit composition and function by the use of subunit-specific monoclonal and polyclonal antibodies. J Exp Med. 1984 Dec 1;160(6):1767–1781. doi: 10.1084/jem.160.6.1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupont H. L., Corrado M. L., Sabbaj J. Use of norfloxacin in the treatment of acute diarrheal disease. Am J Med. 1987 Jun 26;82(6B):79–83. doi: 10.1016/0002-9343(87)90624-3. [DOI] [PubMed] [Google Scholar]
- GARFINKEL B. T., MARTIN G. M., WATT J., PAYNE F. J., MASON R. P., HARDY A. V. Antibiotics in acute bacillary dysentery; observations in 1,408 cases with positive cultures. J Am Med Assoc. 1953 Apr 4;151(14):1157–1160. doi: 10.1001/jama.1953.02940140001001. [DOI] [PubMed] [Google Scholar]
- Goodman L. J., Fliegelman R. M., Trenholme G. M., Kaplan R. L. Comparative in vitro activity of ciprofloxacin against Campylobacter spp. and other bacterial enteric pathogens. Antimicrob Agents Chemother. 1984 Apr;25(4):504–506. doi: 10.1128/aac.25.4.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross R. J., Threlfall E. J., Ward L. R., Rowe B. Drug resistance in Shigella dysenteriae, S flexneri and S boydii in England and Wales: increasing incidence of resistance to trimethoprim. Br Med J (Clin Res Ed) 1984 Mar 10;288(6419):784–786. doi: 10.1136/bmj.288.6419.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haltalin K. C., Nelson J. D., Ring R., 3rd, Sladoje M., Hinton L. V. Double-blind treatment study of shigellosis comparing ampicillin, sulfadiazine, and placebo. J Pediatr. 1967 Jun;70(6):970–981. doi: 10.1016/s0022-3476(67)80275-0. [DOI] [PubMed] [Google Scholar]
- Levine M. M. Antimicrobial therapy for infectious diarrhea. Rev Infect Dis. 1986 May-Jun;8 (Suppl 2):S207–S216. doi: 10.1093/clinids/8.supplement_2.s207. [DOI] [PubMed] [Google Scholar]
- Ling J., Kam K. M., Lam A. W., French G. L. Susceptibilities of Hong Kong isolates of multiply resistant Shigella spp. to 25 antimicrobial agents, including ampicillin plus sulbactam and new 4-quinolones. Antimicrob Agents Chemother. 1988 Jan;32(1):20–23. doi: 10.1128/aac.32.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macaden R., Gokul B. N., Pereira P., Bhat P. Bacillary dysentery due to multidrug resistant Sh. dysenteriae type 1. Indian J Med Res. 1980 Feb;71:178–185. [PubMed] [Google Scholar]
- Meyer P. W., Lerman S. J. Rise and fall of shigella antibiotic resistance. Antimicrob Agents Chemother. 1980 Jan;17(1):101–102. doi: 10.1128/aac.17.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray B. E. Resistance of Shigella, Salmonella, and other selected enteric pathogens to antimicrobial agents. Rev Infect Dis. 1986 May-Jun;8 (Suppl 2):S172–S181. doi: 10.1093/clinids/8.supplement_2.s172. [DOI] [PubMed] [Google Scholar]
- Nelson J. D., Kusmiesz H., Jackson L. H., Woodman E. Trimethoprim-sulfamethoxazole therapy for shigellosis. JAMA. 1976 Mar 22;235(12):1239–1243. [PubMed] [Google Scholar]
- O'Hare M. D., Felmingham D., Ridgway G. L., Grüneberg R. N. The comparative in vitro activity of twelve 4-quinolone antimicrobials against enteric pathogens. Drugs Exp Clin Res. 1985;11(4):253–257. [PubMed] [Google Scholar]
- Paniker C. K., Vimala K. N., Bhat P., Stephen S. Drug resistant shigellosis in south India. Indian J Med Res. 1978 Sep;68:413–417. [PubMed] [Google Scholar]
- Pichler H. E., Diridl G., Stickler K., Wolf D. Clinical efficacy of ciprofloxacin compared with placebo in bacterial diarrhea. Am J Med. 1987 Apr 27;82(4A):329–332. [PubMed] [Google Scholar]
- Pickering L. K., DuPont H. L., Olarte J. Single-dose tetracycline therapy for shigellosis in adults. JAMA. 1978 Feb 27;239(9):853–854. [PubMed] [Google Scholar]
- Ramirez-Ronda C. Quinolones in the treatment of gastrointestinal infections. Chemioterapia. 1987 Jun;6(2 Suppl):488–489. [PubMed] [Google Scholar]
- Shungu D. L., Weinberg E., Gadebusch H. H. In vitro antibacterial activity of norfloxacin (MK-0366, AM-715) and other agents against gastrointestinal tract pathogens. Antimicrob Agents Chemother. 1983 Jan;23(1):86–90. doi: 10.1128/aac.23.1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanhoof R., Hubrechts J. M., Roebben E., Nyssen H. J., Nulens E., Leger J., De Schepper N. The comparative activity of pefloxacin, enoxacin, ciprofloxacin and 13 other antimicrobial agents against enteropathogenic microorganisms. Infection. 1986 Nov-Dec;14(6):294–298. doi: 10.1007/BF01643966. [DOI] [PubMed] [Google Scholar]



