Abstract
Current drug therapy for asthma is highly effective and has evolved from naturally occurring substances through logical pharmaceutical developments. Pharmacology has played a critical role in asthma drug development and several key experimental observations have been published in this journal. Understanding the pharmacology of effective drug therapies has also taught us much about the underlying mechanisms of asthma. β2-Adrenoceptor agonists are the most effective bronchodilators and evolved from catecholamines from the adrenal medulla, whereas corticosteroids, from the adrenal cortex, are by far the most effective controllers of the underlying inflammatory process in the airways. The current ‘gold standard' of asthma therapy is a combination inhaler containing a long-acting β2-agonist with a corticosteroid – an improved form of adrenal gland extract. Cromoglycate, derived from a plant product and theophylline, a dietary methyl xanthine, have also been extensively used in the therapy of asthma, but we still do not understand their molecular mechanisms. Pharmacology has played an important role in improving natural products to make effective long lasting and safe asthma therapies, but has so far been challenged to produce new classes of antiasthma therapy. The only novel class of antiasthma therapy introduced in the last 30 years are leukotriene antagonists, which are less effective than existing treatments. New, more specific, therapies targeted at specific cytokines are less effective than corticosteroids, whereas more effective therapies carry a risk of side effects that may not be acceptable. It seems likely that pharmacology, rather than molecular genetics, will remain the main approach to the further improvement of treatment for asthma.
Keywords: Asthma, bronchodilator, β-adrenoceptor agonist, muscarinic antagonist; theophylline, cromoglycate, corticosteroids
Introduction
We have now evolved highly effective drugs for the management of asthma that have led to a marked reduction in hospital admissions and mortality for this increasingly common disease. Most patients with asthma are now able to lead a normal life through the use of medications that are virtually free of side effects. Indeed, current therapies are so effective that it has so far been proved impossible to develop any new classes of drug that are more effective than existing agents. The advances in asthma therapy have been largely through improving the selectivity and duration of action of existing effective classes of drugs. With respect to this, pharmacology has played an important role in validating drug targets and drug design. Pharmacology, particularly through the use of selective agonists and antagonists, has also played an important role in increasing our understanding of the underlying inflammatory mechanisms of asthma, providing a rational basis for the use of current drug therapy. The history of asthma treatment goes back to thousands of years, but most of the important advances have been made during the last 75 years. As indicated in this review several key studies have been published in the British Journal of Pharmacology. Autonomic pharmacology, which evolved and has always been very strong in the U.K., has played a particularly important role in the development of bronchodilators and British pharmaceutical companies have played (and continue to play) a leading role in the development of asthma medications, supported by strong interactions with basic and clinical pharmacologists.
It is of interest that many of our effective therapies for asthma were originally derived from natural substances. Many were isolated from plants through the discovery of herbal remedies, including atropine, dietary xanthines such as theophylline and chromones from a Mediterranean medicinal herb. The most effective treatments for asthma are derived from hormones, β-adrenoceptor agonists from adrenaline and corticosteroids from cortisone, both secreted by the adrenal gland. Indeed, the most effective therapies available for asthma so far are combination inhalers containing a long-acting β-agonist and a corticosteroid.
Muscarinic receptor antagonists
The leaves of Datura, commonly known as Jimson weed or thorn apple, which were smoked in India for several centuries as a treatment for respiratory disorders (including asthma), contain a muscarinic receptor antagonist, atropine. The ancient Egyptians also inhaled the vapour of heated henbane (Hyoscyamus muticus), which contains another antimuscarinic alkaloid, scopolamine, for the treatment of asthma-like conditions. These therapies were available until well into the last century but fell into disuse with the introduction of more effective bronchodilators derived from adrenaline. An important advance in the use of muscarinic receptor antagonists for asthma was the development of quaternary ammonium derivatives, which did not pass the blood–brain barrier and thus were devoid of the central side effects, such as hallucinations, of naturally occurring atropine-like compounds. Although these quaternary derivatives are not absorbed from the gastrointestinal tract, they are effective when inhaled and ipratropium bromide, a synthetic quaternary antimuscarinic compound, is still used as a bronchodilator in patients with severe asthma. However, it is less effective than a β-agonist, as cholinergic bronchoconstriction is only a relatively small component of the bronchoconstriction in asthma compared to the direct bronchoconstrictor action of other inflammatory mediators in most patients. However, antimuscarinic agents have turned out to be the bronchodilators of choice in the treatment of chronic obstructive pulmonary disease (COPD), where the only reversible component appears to be cholinergic tone in the airways. The most recent advance has been the introduction of the long-acting antimuscarinic, tiotropium, developed by Boehringer Ingelheim, which induces bronchodilatation lasting for several days (Hansel & Barnes, 2002).
A key development in muscarinic pharmacology has been the recognition of distinct muscarinic receptor subtypes, which have different functions and distribution. An important development in lung pharmacology made by Fryer & Maclagan (1984) was the recognition that M3 receptors mediate the bronchoconstrictor effect of cholinergic tone, whereas M2 receptors functioned as feedback inhibitory receptors (autoreceptors) in parasympathetic nerves of animals. This was subsequently confirmed in human airways (Minette & Barnes, 1988). The clinical consequence is that the nonselective muscarinic antagonists, such as atropine and ipratropium, will also increase acetylcholine production from cholinergic nerves by blocking the M2 autoreceptors and may thus overcome the blockade of the M3 receptors on airway smooth muscle cells. This led to the idea that M3-selective antagonists may be more effective as bronchodilators. Indeed, tiotropium has a kinetic selectivity for M3 receptors as it dissociates much more slowly from M3 receptors than from M2 receptors. However, it has not been convincingly shown that M3 receptor selectivity has any important clinical advantage and the long duration of action is a much more important advantage. New developments include more long-acting muscarinic antagonists which will be used alone and in combination with long-acting β2-agonists, mainly for COPD patients, but also for patients with asthma. Interestingly, an old antimuscarinic drug, glycopyrrolate, used for many years by anaesthetists to dry upper airway secretions, has recently been found to have a similar pharmacology to tiotropium with kinetic selectivity for M3 receptors and a long duration of action when given by inhalation.
β-Adrenoceptor agonists
Ephedrine, derived from the plant Ephedra and known in Chinese medicine as Ma Huang, has been used in the treatment of respiratory diseases for over 5000 years. Ephedrine is thus the earliest antiasthma agent known. It acts indirectly, by releasing endogenous catecholamines, resulting in bronchodilatation. It was shown to be effective by inhalation by Dale as early as 1910 (Barger & Dale, 1910). Oliver and Sharpey-Shafer were the first to describe the effect of adrenal gland extract on blood pressure but they did not study any airway effects. It was Solis-Cohen (1900), a physician from Philadelphia, who first showed that orally administered adrenal extract (adrenal substance pills) was beneficial in asthma and the direct bronchodilator effect of adrenaline was first demonstrated by Kahn in 1907 using precontracted tracheal strips in vitro (Brewis, 1990). Adrenaline given by subcutaneous injection became a widely used treatment, particularly for acute exacerbations of asthma. Of course, adrenergic agonists are now given preferably by inhalation and the first known description of inhaled adrenaline in asthma was by Percy Camps, a general practitioner from Teddington, who described the efficacy of nebulising an adrenaline solution with oxygen in patients with acute exacerbations of asthma (Brewis, 1990).
Isoprenaline was synthesised by German chemists in the 1940s and was shown to have less cardiovascular side effects than adrenaline and became the most widely used inhaled treatment for asthma for about 20 years. It was the synthesis of isoprenaline that allowed Ahlquist in 1948 to distinguish between α- and β-adrenergic receptors, based on the difference in bronchial response to isoprenaline and noradrenaline (Ahlquist, 1948). In 1967 Lands et al. (1967) demonstrated, using the rank order of potency of natural and synthetic sympathomimetic amines, that β-receptors could be further subdivided into β1-receptors in the heart and β2-receptors in the airways. Isoetharine had been found by Lands to be a highly selective agonist at β2-adrenoceptors and this was confirmed in humans by Collier & Dornhorst (1969). However, isoetharine was short-lived in its effects, like isoprenaline, due to rapid metabolism of the catechol ring. A major breakthrough was the discovery of the first β2-selective agonist with a longer duration of action than isoprenaline by the team at Glaxo led by David Jack and Roy Brittain (Figure 1; Brittain et al., 1968), and its pharmacology was elegantly described in the British Journal of Pharmacology by Cullum et al. (1969) (later Alabaster). This compound, salbutamol, remains the most widely used antiasthma drug in the world today.
Figure 1.
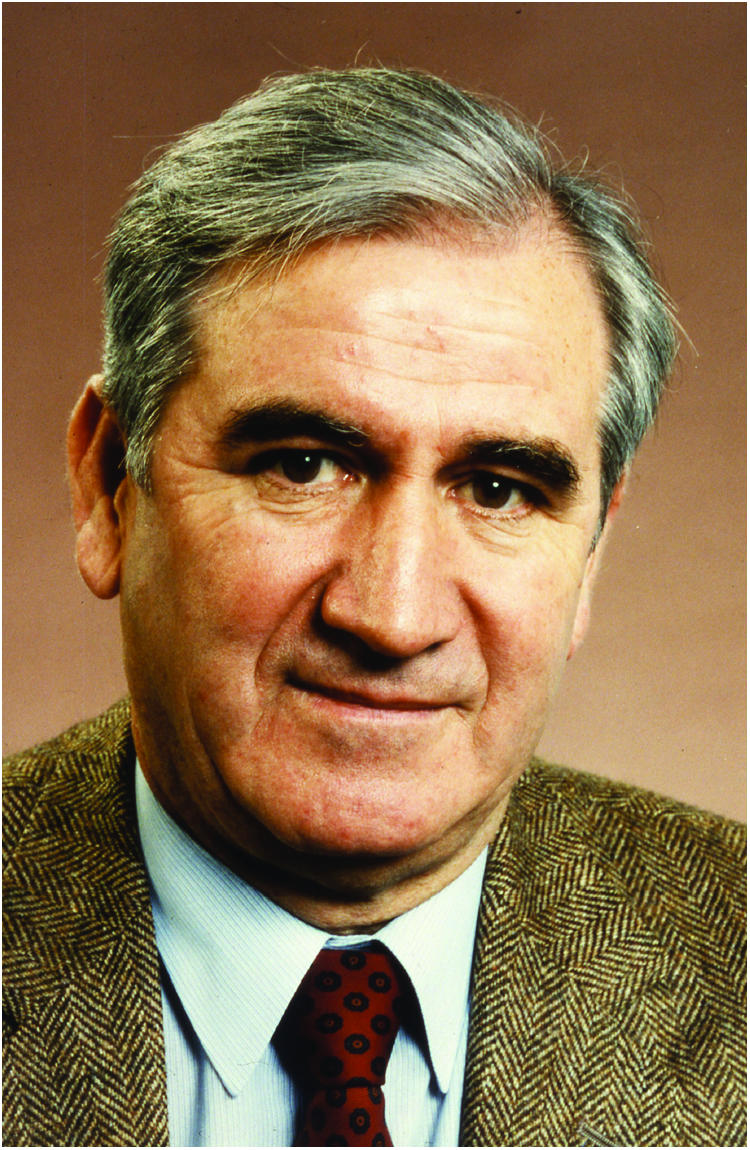
Sir David Jack, FRS.
The next logical development was to extend the duration of action of salbutamol by substitution in the side chain and this resulted in the discovery by Brittain and Jack of salmeterol, the first long-acting β2-agonist with a bronchodilator action of over 12 h (Ball et al., 1991). Inhaled salmeterol was shown to have a prolonged duration of action in patients with asthma (Ullman & Svedmyr, 1988) and was introduced into clinical practice in 1990. Another long-acting β2-agonist, formoterol, was initially used in tablet form in Japan, with no indication of a long duration of action. This was only discovered when formoterol was given by inhalation to asthmatic patients and shown to have a similar duration of action to salmeterol. These long-acting β2-agonists have found an important place in the management of asthma in combination with a corticosteroid. These combination inhalers are the most effective asthma therapies currently available, as the long-acting β2-agonist and corticosteroids exert complementary actions and, in some situations, can show synergism (Barnes, 2002). Combination inhalers are now the most rapidly grown segment of the antiasthma market, with the most recent development being the synthesis of even longer acting β2-agonists, such as indacaterol (QAB149), which has a duration of over 24 h making it suitable for once-daily dosing (Beeh et al., 2005).
Corticosteroids
Corticosteroids are the most effective controllers of asthma and it has been proved to be extremely difficult to find any new treatment that comes close to providing an equal therapeutic benefit. It is likely that the benefits of orally administered adrenal extract described by Solis-Cohen in 1900 was, in fact, due to the steroid content rather than any adrenaline present, as the adrenaline would be extensively metabolised on its absorption from the gastrointestinal tract. The gut wall and liver contain high levels of monoamine oxidase, the major enzyme inactivating endogenous monoamines including catecholamines (see also Youdim & Bakhle, this issue). This was not recognised at the time and it was almost 50 years later, when cortisol had been isolated from the adrenal cortex, that the idea of corticosteroids as therapy for asthma became clear. The Nobel Prize for Medicine and Physiology was awarded in 1950 to Kendall and Reichstein who had independently isolated and synthesised cortisol and then adrenocorticotropic hormone (ACTH) and Philip Hench, a rheumatologist working at the Mayo Clinic, who had demonstrated its dramatic efficacy when given by intravenous injection in patients with rheumatoid arthritis. Only 6 months after Hench's demonstration of the clinical efficacy of ACTH in rheumatoid patients, Boardley et al. (1949) at Johns Hopkins University had shown that it had equally good effects in patients with asthma. They described five patients with asthma, interestingly all of whom had eosinophilic sputum, who improved rapidly with intramuscular injections of ACTH over a 3-week period with disappearance of the sputum. They later confirmed these observations in a larger group of patients. Subsequently, oral cortisone, widely used at that time to treat several inflammatory diseases, was shown to be an effective replacement for the injections, in patients with difficult-to-control asthma. However, there was scepticism in the U.K. leading to a Medical Research Council multicentre trial of cortisone in asthma patients, which was the first placebo-controlled trial performed in asthma (Medical Research Council, 1956). Surprisingly the results were disappointing with few clinical improvements that were not sustained during the 2 months of therapy. This may have reflected the low dose of cortisone used, the lack of objective measurements of lung function and the inclusion of many patients who had COPD. Despite this poor result, oral steroids were used more and more in patients with severe asthma, but it was clear that side effects were a major problem, resulting in stunting of growth in children, osteoporosis and metabolic disturbances.
This immediately suggested the need to give corticosteroids by inhalation as a way of reducing systemic side effects, yet cortisone and dexamethasone given by inhalation proved to be of little benefit. This was because of their lack of topical efficacy and led to a search for topically active steroids. McKenzie & Stoughton (1962) discovered that this topical efficacy was correlated with skin blanching, although the cellular basis for this test is still uncertain. Hydrocortisone turned out to be weak in the McKenzie test, but two synthetic steroids, beclomethasone dipropionate (BDP) and betamethasone-17-valerate gave good skin blanching responses. Both of these steroids were effective as topical treatments for eczema, predicting that they would also be effective by inhalation. Both of these new steroids were developed for inhalation and an important paper by Harry Morrow Brown and co-workers in 1972 established that inhaled BDP was very effective in reducing the need for oral corticosteroids and in many patients achieved better control (Brown et al., 1972). Interestingly, Brown reported that the patients who did best had high numbers of eosinophils in their sputum, an observation that has been confirmed in many subsequent studies. The widespread use of inhaled corticosteroids in asthma has been the major reason why asthma morbidity and recently mortality have fallen. There is now a search for inhaled corticosteroids with improved therapeutic ratios and less systemic side effects, with the introduction of budesonide and fluticasone propionate which have reduced oral bioavailability and recently ciclesonide, which is a prodrug, activated by esterases in the lower airways.
There has recently been a much better understanding of the molecular mechanisms involved in the anti-inflammatory effects of corticosteroids in asthma, with particular emphasis on the effects of corticosteroids on chromatin remodelling through increased recruitment of histone deacetylase-2 to activated inflammatory genes (Barnes & Adcock, 2003). In the future, there is a prospect for selective glucocorticoid receptor agonists or dissociated steroids, which have improved anti-inflammatory effects through repression of activated inflammatory genes and reduced binding of glucocorticoid receptors to DNA, which is thought to mediate side effects (see also Buckingham, this issue). Interestingly, the topically active corticosteroids now used in inhalers for asthma already show a degree of dissociation.
Chromones
Khellin is a naturally occurring chromone, extracted from the medicinal plant Amni visnaga and long used in Egypt and the Eastern Mediterranean countries for the treatment of respiratory disorders. Khellin has bronchodilator properties but also caused nausea and a research group at Fisons Pharmaceuticals decided to test related chromone derivatives as potential antiasthma drugs. As there was no satisfactory animal model these compounds were tested on allergen challenge in asthmatic volunteers, including the leader of the team, Roger Altounyan (Figure 2). Altounyan identified the most active compounds, leading eventually to the synthesis of a bis-chromone, disodium cromoglycate (DSCG). This remarkable drug inhibited not only antigen challenge but also challenges due to exercise and irritant gases. DSCG was orally inactive and had to be given by a dry powder inhaler device (Spinhaler) that was devised by Altounyan. DSCG proved to be effective in clinical trials in asthmatic patients and was without side effects (Howell & Altounyan, 1967). However, DSCG had a short duration of action, prompting the search for compounds of longer duration or that were orally active. Nedocromil sodium was introduced as a slightly longer-acting inhaled cromone but had little advantage over DSCG. Chromones have now largely been replaced by inhaled corticosteroids, but they remain a fascinating novel therapy with an unknown mode of action. Although it was believed that chromones worked as mast cell stabilisers (Cox, 1967), it later became clear that they also worked on other cell types, including sensory nerves. Their lack of side effects implied that their effect was specific for the abnormality of asthma, but their molecular target has not yet been identified, although there is some evidence that they act on certain chloride channels (Norris & Alton, 1996). Identification of the molecular mechanism of action of chromones may be an important approach to finding new antiasthma medications and the development of longer acting and perhaps orally active drugs that target the same mechanism.
Figure 2.
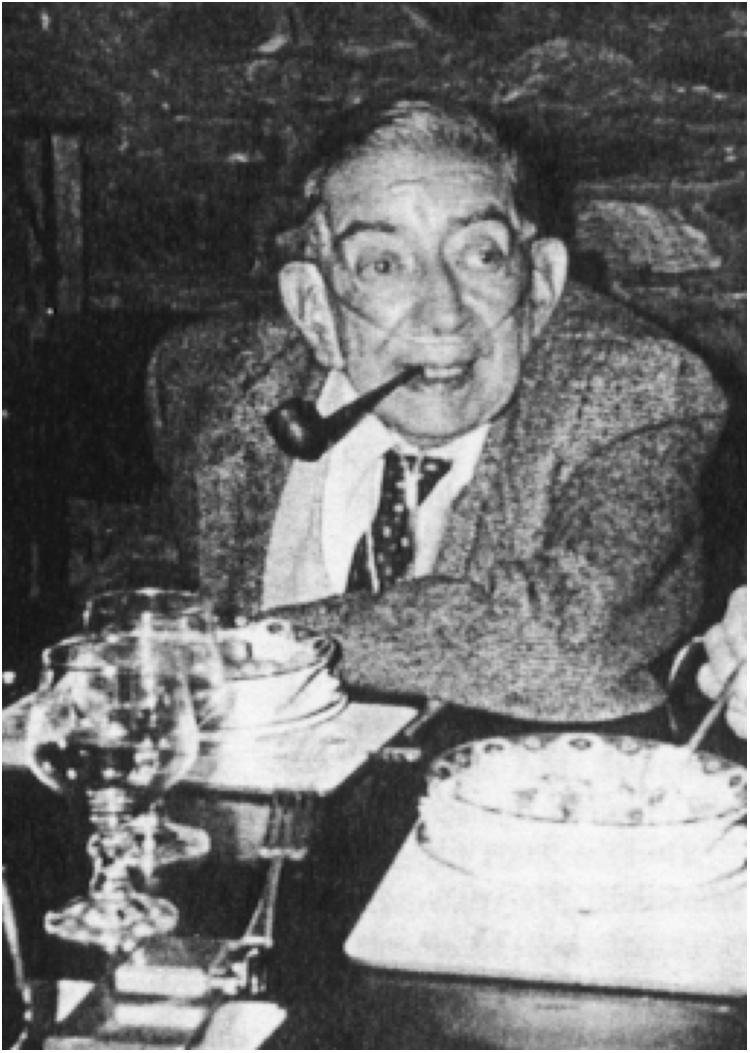
Dr Roger Altounyan (1922–1987).
Theophylline
Theophylline, a methyl xanthine found in tea, was isolated at the end of the 19th century but its use in asthma was not seen until Hirsch (1922) described its bronchodilator effect in three asthmatic patients and its relaxant effect in bovine airways in vitro. This confirmed the in vitro observations made in the previous year by Macht & Ting (1921). The soluble ethylene diamine salt of theophylline, aminophylline, was developed for intravenous administration and shown to be very effective in acute severe asthma, particularly in patients who had not responded well to adrenaline (Hermann et al., 1937). Intravenous aminophylline remained a standard treatment for acute exacerbations of asthma until displaced by nebulised β2-agonists over the last 20 years. It is still used in occasional patients who fail to respond to adrenergic bronchodilators. The main limitations of theophylline are its side effects, such as nausea, headache and diuresis, which occurred within the therapeutic range and occasionally the very serious adverse effects of cardiac arrhythmias and seizures. Indeed, overdosage of aminophylline was to become the commonest cause of death due to asthma in hospital.
This led to several studies relating the efficacy and side effects of theophylline to plasma concentrations. In a classical pharmacokinetic study, Mitenko & Ogilvie (1973) demonstrated that the bronchodilator effect of theophylline was related to plasma concentration between 5 and 20 mg l−1, but above 20 mg l−1, side effects were very common. This led to recommendations for a therapeutic range of 10–20 mg l−1, although even within this range side effects were relatively common. Plasma monitoring became routine, particularly in view of the variable pharmacokinetics of theophylline and the multiplicity of factors that affected plasma concentrations. Oral theophylline was a very popular treatment which was inexpensive, eventually becoming the most widely used therapy worldwide, but it has a short duration of action. This limitation led to the formulation of slow-release theophylline and aminophylline preparations that could be given once or twice daily, which were successful due to their convenience and greater tolerability. Side effects limited the use of theophylline as a bronchodilator and the introduction of inhaled β2-agonists as bronchodilators led to a decline in its use as β-agonists were more effective and better tolerated. Theophylline is still used in the management of severe asthma as an additional therapy added to inhaled corticosteroids and there has recently been a revival of interest in its mechanisms of action (Barnes, 2003).
The bronchodilator effect of theophylline appears to be due to inhibition of phosphodiesterases (principally PDE3 and 4) in airway smooth muscle and this may also account for the nausea, headaches and some of the cardiovascular side effects, explaining why these side effects are commonly seen at bronchodilator doses. Theophylline acts as a functional antagonist in airway smooth muscle and has greater efficacy than β2-agonists when airway smooth muscle is strongly contracted (Karlsson & Persson, 1981). Theophylline is also an adenosine receptor antagonist at relatively high concentrations and this may account for serious side effects such as cardiac arrhythmias and seizures. However, there is increasing evidence that at lower plasma concentrations (5–10 mg l−1) theophylline has nonbronchodilator effects that include anti-inflammatory actions and immunomodulatory effects. These cannot be accounted for by PDE inhibition or adenosine antagonism suggesting that there is some other molecular basis for these effects. Recently, theophylline in low therapeutic concentrations has been shown to activate the nuclear enzyme histone deacetylase and thereby to switch off activated inflammation genes in an action that is synergistic with corticosteroids (Ito et al., 2002). This interaction may open up possibilities for novel anti-inflammatory therapies in the future.
Antagonists of inflammatory mediators
Many mediators have been implicated in the pathophysiology of asthma with the result that even more antagonists and synthesis inhibitors have been developed as potential antiasthma therapies. Inflammatory mediators come and go in popularity, but most have proved to be disappointing as therapeutic targets for asthma. There are over 100 mediators already implicated in asthma, making it unlikely (but not impossible) that blocking a single mediator would have a major clinical effect (Barnes et al., 1998).
Histamine was the first mediator implicated in the pathophysiology of asthma since Dale's demonstration that it mimicked anaphylactic bronchoconstriction in guinea pigs (Dale & Laidlaw, 1910). Schild went on to show that sensitised asthmatic lung tissue and airways caused bronchoconstriction through the release of histamine (Schild et al., 1951). Curry (1946) showed that intravenous and inhaled histamine caused bronchoconstriction in patients with asthma but not in normal subjects. He was thus the first to demonstrate airway hyper-responsiveness in patients with asthma, which is the defining physiological abnormality of this disease and remains an important target of asthma therapy. All this research suggested that antihistamines might be a useful therapy for asthma. In a classic paper published in the British Journal of Pharmacology, Ash and Schild showed that the classical antihistamine mepyramine blocked the contraction of guinea-pig trachea, but not the gastric acid secretion, deducing that there were different types of histamine receptors (Ash & Schild, 1966; see also Parsons & Ganellin, this issue). Mepyramine blocks histamine H1 receptors and antihistamines, such as mepyramine and chlorpheniramine, were tested in asthma but with disappointing results. Even with the development of much more potent nonsedating H1-receptor antagonists, there is no clinical benefit in patients with asthma. The reason for this disappointing finding is that there are other bronchoconstrictor mediators produced in asthma.
There was particular interest in another mediator released from lungs that was clearly different from histamine. Kellaway, Feldberg and co-workers demonstrated that guinea-pig lungs perfused with cobra venom or as shown later, allergen, released a substance that contracted smooth muscle preparations more slowly than histamine, which they designated slow-reacting muscle-stimulant substance (Feldberg & Kellaway, 1938). It was subsequently shown to be released with histamine during anaphylactic shock and termed slow-reacting substance of anaphylaxis (SRS-A) (Brocklehurst, 1960). We made great efforts to identify this substance but it was not until 1979 that the chemical structure of SRS-A was identified as a mixture of lipid mediators called leukotrienes, from the fact that they could be derived from leukocytes and the carbon backbone had three double bonds (Murphy et al., 1979). The biosynthetic pathway for the cysteinyl-leukotrienes (cys-LT) involved the initial oxidation of arachidonic acid by 5′-lipoxygenase and subsequent conjugation with glutathione. The effects of cys-LTs were blocked by the previously discovered SRS-A anatgonist called FPL 55712. Priscilla Piper and her co-workers carried out a series of studies on the pharmacological properties of cys-LTs (Piper & Samhoun, 1982), which were shown to be potent bronchoconstrictors when given by inhalation to asthmatic patients. This then led to a search for more potent and selective cys-LT antagonists or 5′-lipoxygenase inhibitors, culminating in the development of several highly potent cys-LT1-receptor antagonists, such as zafirlukast and montelukast. These were introduced into clinical practice in the 1990s and were the first new class of anti-asthma therapy for over 30 years. Although cys-LT antagonists have some clinical efficacy in asthma patients, they have proved to be relatively weak compared to inhaled corticosteroids. However, they have some value as an add-on therapy to inhaled corticosteroids and have the advantage of oral administration without significant side effects.
Other mediator antagonists, including antagonists of kinins, platelet-activating factor or inhibitors of prostaglandin synthesis provide no clinical benefit in asthma. More recently inhibition of key cytokines, such as interleukin (IL)-4 and IL-5 have also been found to have little or no clinical efficacy in asthma patients (Barnes, 2004). This lack of efficacy of single mediator antagonists presumably reflects the multiplicity of mediators in asthma and the redundancy of their effects. It suggests that effective asthma therapies need to have a broad spectrum of anti-inflammatory activity.
Future directions in pharmacological therapy
There has been great pressure from the pharmaceutical industry to develop new drugs for asthma as this is an enormous and expanding global market. However, it has proved to be a difficult challenge as existing therapies are highly effective and safe. Combination inhalers with a corticosteroid and a long-acting β2-agonist are the most effective treatment so far available and it is likely that several combination inhalers will become available, including once-daily drugs. There is a need to find more effective therapies for patients with more severe asthma, who are not well controlled by current therapies. Although this is a small minority of patients (<5%) they account for more than half of the health care spending on asthma. New treatments in development for asthma include inhibitors of the proinflammatory enzymes, such as PDE4, p38 mitogen-activated kinase and nuclear-factor-κB activating kinase (IKK2) (Barnes, 2004). More specific approaches include inhibiting chemokine receptors on eosinophils and T lymphocytes, inhibiting adhesion molecules that recruit key inflammatory cells and inhibiting mast cells with Syk kinase inhibitors. Antibodies that block IgE have now been introduced in some countries and have clinical efficacy, especially in patients with severe allergic asthma. None of the treatments currently available for asthma change the natural history of the disease or are curative. There is now interest in vaccination approaches that divert the immune system in asthmatic patients back to normal, but the potential dangers of such approaches have not been explored.
Final comments
Pharmacology has played an important role in identifying and validating new targets in asthma therapy over the last 75 years and it will continue to be a vital part of progress in the future. Human pharmacology studies have been of particular value, in view of the disappointing predictability of animal models of asthma. Allergen challenge in asthmatic volunteers has proved to be particularly valuable. All of the treatments that have been effective in asthma have demonstrated an effect on some aspect of the allergen response, whereas drugs that have not shown antiallergic activity have failed in subsequent clinical trials for asthma. Novel genes associated with asthma have been identified by molecular genetic techniques, but this has not yet resulted in any new treatment approaches. In the future, it may be possible to identify subsets of asthmatic patients through genetic analysis so that more specific therapies can be administered, but so far pharmacogenetics has had little clinical impact. A more significant contribution of pharmacogenetics in the future may be in selecting patients that respond best to more specific therapies.
Glossary
- ACTH
adrenocorticotrophic hormone
- BDP
beclomethasone dipropionate
- COPD
chronic obstructive pulmonary disease
- Cys-LT
cysteinyl leukotriene
- DSCG
disodium cromoglycate
- PDE
phosphodiesterase
- SRS-A
slow-reacting substance of anaphylaxis
References
- AHLQUIST R.P. A study of adrenotropic receptors. Am. J. Physiol. 1948;153:586. doi: 10.1152/ajplegacy.1948.153.3.586. [DOI] [PubMed] [Google Scholar]
- ASH A.S.P., SCHILD H.O. Receptors mediating some actions of histamine. Br. J. Pharmac. Chemother. 1966;27:427–439. doi: 10.1111/j.1476-5381.1966.tb01674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BALL D.I., BRITTAIN R.T., COLEMAN R.A., DENYER L.H., JACK D., JOHNSON M., LUNTS L.H., NIALS A.T., SHELDRICK K.E., SKIDMORE I.F. Salmeterol, a novel, long-acting β2-adrenoceptor agonist: characterization of pharmacological activity in vitro and in vivo. Br. J. Pharmacol. 1991;104:665–671. doi: 10.1111/j.1476-5381.1991.tb12486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BARGER G., DALE H.H. Chemical structure and sympathomimetic action of amines. J. Physiol. 1910;41:19–59. doi: 10.1113/jphysiol.1910.sp001392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BARNES P.J. Scientific rationale for combination inhalers with a long-acting β2-agonists and corticosteroids. Eur. Respir. J. 2002;19:182–191. doi: 10.1183/09031936.02.00283202. [DOI] [PubMed] [Google Scholar]
- BARNES P.J. Theophylline: new perspectives on an old drug. Am. J. Respir. Crit. Care Med. 2003;167:813–818. doi: 10.1164/rccm.200210-1142PP. [DOI] [PubMed] [Google Scholar]
- BARNES P.J. New drugs for asthma. Nat. Rev. Drug Discov. 2004;3:831–844. doi: 10.1038/nrd1524. [DOI] [PubMed] [Google Scholar]
- BARNES P.J., ADCOCK I.M. How do corticosteroids work in asthma. Ann Intern. Med. 2003;139:359–370. doi: 10.7326/0003-4819-139-5_part_1-200309020-00012. [DOI] [PubMed] [Google Scholar]
- BARNES P.J., CHUNG K.F., PAGE C.P. Inflammatory mediators of asthma: an update. Pharmacol. Rev. 1998;50:515–596. [PubMed] [Google Scholar]
- BEEH K.M., SCHELFOUT V., GRONKE F., KANNIESS F., CAMERON R., VAN AS A. QAB149: the first once-daily β2-agonist with 24-h bronchodilation. Proc. Amer. Thorac. Soc. 2005;2:A356. [Google Scholar]
- BOARDLEY J.E., CAREY R.A., HARVEY A.M. Preliminary observations on the effect of adrenocorticotropic hormone in allergic diseases. Bull. Johns. Hopkins. Hosp. 1949;85:396–410. [PubMed] [Google Scholar]
- BREWIS R.A.L. Classical Papers in Asthma. London: Science Press; 1990. [Google Scholar]
- BRITTAIN R.T., FARMER J.B., JACK D., MARTIN L.E., SIMPSON W.T. Alpha-[(t-Butylamino)methyl]-4-hydroxy-m-xylene-alpha 1,alpha 3-diol (AH.3365): a selective beta-adrenergic stimulant. Nature. 1968;219:862–863. doi: 10.1038/219862a0. [DOI] [PubMed] [Google Scholar]
- BROCKLEHURST W.E. The release of histamine and formation of a slow-reacting substance (SRS-A) during anaphylactic shock. J. Physiol. 1960;151:416–435. doi: 10.1113/jphysiol.1960.sp006449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BROWN H.M., STOREY G., GEORGE W.H. Beclomethasone dipropionate: a new steroid aerosol for the treatment of allergic asthma. BMJ. 1972;1:585–590. doi: 10.1136/bmj.1.5800.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COLLIER J.G., DORNHORST A.C. Evidence for two different types of beta-receptors in man. Nature. 1969;223:1283–1284. doi: 10.1038/2231283a0. [DOI] [PubMed] [Google Scholar]
- COX J.S.G. Disodium cromoglycate (FPL 670) (‘Intal'): a specific inhibitor of reaginic antibody-antigen mechanisms. Nature. 1967;216:1328–1329. doi: 10.1038/2161328a0. [DOI] [PubMed] [Google Scholar]
- CULLUM V.A., FARMER J.B., JACK D., LEVY G.P. Salbutamol: a new, selective beta-adrenoceptive receptor stimulant. Br. J. Pharmacol. 1969;35:141–151. doi: 10.1111/j.1476-5381.1969.tb07975.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CURRY J.J. The action of histamine on the repiratory tract in normal and asthmatic subjects. J. Clin. Invest. 1946;25:785–791. doi: 10.1172/JCI101764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DALE H.H., LAIDLAW P.P. The physiological action of β-iminazoly-ethylamine. J. Physiol. 1910;41:318–341. doi: 10.1113/jphysiol.1910.sp001406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FELDBERG W., KELLAWAY C.H. Liberation of histamine and formation of lysocithin-like substances by cobra venom. J. Physiol. 1938;94:187–226. doi: 10.1113/jphysiol.1938.sp003674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FRYER A.D., MACLAGAN J. Muscarinic inhibitory receptors in pulmonary parasympathetic nerves in the guinea-pig. Br. J. Pharmacol. 1984;83:973–978. doi: 10.1111/j.1476-5381.1984.tb16539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HANSEL T.T., BARNES P.J. Tiotropium bromide: a novel once-daily anticholinergic bronchodilator for the treatment of COPD. Drugs Today. 2002;38:585–600. doi: 10.1358/dot.2002.38.9.696535. [DOI] [PubMed] [Google Scholar]
- HERMANN G.R., AYNESWORTH M.B., MARTIN J. Succesful treatment of persistent extreme dyspnea ‘Status asthmaticus' – use of theophylline ethylene diamine. J. Lab. Clin. Med. 1937;23:135–148. [PubMed] [Google Scholar]
- HIRSCH S. Klinischer und experimenteller Beitrag zur krampfloseneden Wirkung der Purin Derivativ. Klin. Wochenschr. 1922;1:615–618. [Google Scholar]
- HOWELL J.B., ALTOUNYAN R.E. A double-blind trial of disodium cromoglycate in the treatment of allergic bronchial asthma. Lancet. 1967;2:539–542. doi: 10.1016/s0140-6736(67)90499-0. [DOI] [PubMed] [Google Scholar]
- ITO K., LIM S., CARAMORI G., COSIO B., CHUNG K.F., ADCOCK I.M., BARNES P.J. A molecular mechanism of action of theophylline: Induction of histone deacetylase activity to decrease inflammatory gene expression. Proc. Natl. Acad. Sci. U.S.A. 2002;99:8921–8926. doi: 10.1073/pnas.132556899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KARLSSON J.A., PERSSON C.G. Influence of tracheal contraction on relaxant effects in vitro of theophylline and isoprenaline. Br. J. Pharmacol. 1981;74:73–79. doi: 10.1111/j.1476-5381.1981.tb09956.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LANDS A.M., ARNOLD A., MCAULIFF J.P., LUDUENA F.P., BROWN T.G., JR Differentiation of receptor systems activated by sympathomimetic amines. Nature. 1967;214:597–598. doi: 10.1038/214597a0. [DOI] [PubMed] [Google Scholar]
- MACHT D., TING G.C. A study of antispasmodic drugs on the bronchus. J. Pharmacol. Exp. Ther. 1921;18:373–398. [Google Scholar]
- MCKENZIE A.W., STOUGHTON R.B. Method for comparing percutaneous absorption of steroids. Arch. Dermatol. 1962;86:608–610. [Google Scholar]
- MEDICAL RESEARCH COUNCIL. Controlled trial of effects of cortisone acetate in status asthmaticus; report to the Medical Research Council by the subcommittee on clinical trials in asthma. Lancet. 1956;271:803–806. [PubMed] [Google Scholar]
- MINETTE P.A., BARNES P.J. Prejunctional inhibitory muscarinic receptors on cholinergic nerves in human and guinea-pig airways. J. Appl. Physiol. 1988;64:2532–2537. doi: 10.1152/jappl.1988.64.6.2532. [DOI] [PubMed] [Google Scholar]
- MITENKO P.A., OGILVIE R.I. Rational intravenous doses of theophylline. New Engl. J. Med. 1973;289:600–603. doi: 10.1056/NEJM197309202891202. [DOI] [PubMed] [Google Scholar]
- MURPHY R.C., HAMMARSTROM S., SAMUELSSON B. Leukotriene C: a slow-reacting substance from murine mastocytoma cells. Proc. Natl. Acad. Sci. U.S.A. 1979;76:4275–4279. doi: 10.1073/pnas.76.9.4275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NORRIS A.A., ALTON E.W. Chloride transport and the action of sodium cromoglycate and nedocromil sodium in asthma. Clin. Exp. Allergy. 1996;26:250–253. [PubMed] [Google Scholar]
- PIPER P.J., SAMHOUN M.N. Stimulation of arachidonic acid metabolism and generation of thromboxane A2 by leukotrienes B4, C4 and D4 in guinea-pig lung in vitro. Br. J. Pharmacol. 1982;77:267–275. doi: 10.1111/j.1476-5381.1982.tb09295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SCHILD H.O., HAWKINS D.F., MONGAR J.L., HERXHEIMER H. Reaction of isolated human and asthmatic lung and bronchial tissue to a specifci antigen. Histamine release and muscular contraction. Lancet. 1951;2:376–382. doi: 10.1016/s0140-6736(51)91554-1. [DOI] [PubMed] [Google Scholar]
- SOLIS-COHEN S. The use of adrenal substances in the treatment of asthma. JAMA. 1900;34:1164–1169. [Google Scholar]
- ULLMAN A., SVEDMYR N. Salmeterol, a new long acting inhaled β2-adrenoceptor agonist: comparison with salbuterol in adult asthmatic patients. Thorax. 1988;43:674–678. doi: 10.1136/thx.43.9.674. [DOI] [PMC free article] [PubMed] [Google Scholar]


