Abstract
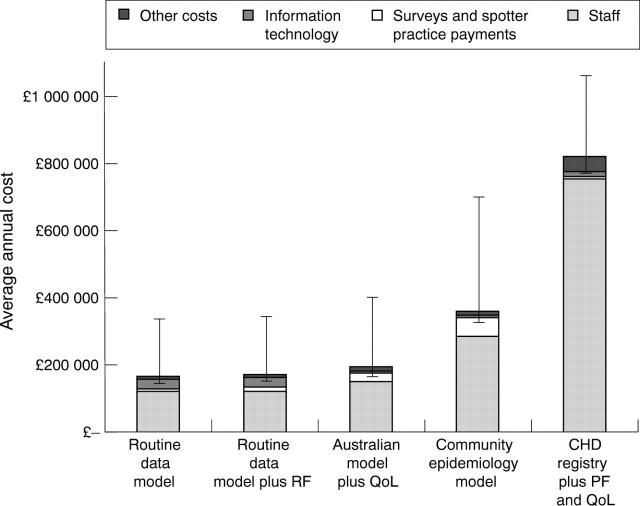
OBJECTIVE—To evaluate the costs and benefits of alternative systems of coronary heart disease monitoring in Scotland. DESIGN—An option appraisal was conducted to evaluate the costs and benefits of implementing a coronary heart disease monitoring system. This involved a review of existing Scottish datasets and relevant reports, specification of options, definition and weighting of benefit criteria by key stakeholders, assessment of options by experts, and costing of options. The options were assessed by 33 stakeholders (grouped as cardiologists, patient representatives, general practitioners, public health physicians, and policy makers), plus 13 topic experts. SETTING—Scotland (population 5.1 million). RESULTS—Between group mean benefit weights were: mortality rates and case fatality (10.6), quality of life (9.8), patient function (8.8), hospital activity (7.8), primary care activity (9.25), prescribing (5.72), socioeconomic impact (4.0), risk factors (7.4), prevalence (5.0), incidence (6.0), case registration (6.82), international comparability (4.2), breadth of coverage (8.8), and frequency (5.8). Differences between group weights were significant for prevalence (p = 0.048) and international comparability (p = 0.032). Four monitoring options were identified: a community epidemiology model, based on MONICA (monitoring trends and determinants in cardiovascular disease) study methodology applied to a series of eight representative communities, had the highest benefits, at an average annual discounted cost of approximately £360 000; models based on the Australian cardiovascular disease monitoring scheme and on enhanced routine data offered fewer benefits at discounted average annual costs ranging from £165 000 to £195 000; finally, a coronary heart disease registry modelled on the Scottish Cancer Registry scheme would have had fewer benefits and substantially higher costs than the other options. CONCLUSIONS—The most beneficial coronary heart disease monitoring system is the community epidemiology model, based on MONICA methodology. Option appraisal potentially offers an explicit and transparent methodology for evidence based policy development. Keywords: monitoring; surveillance; heart disease; option appraisal
Full Text
The Full Text of this article is available as a PDF (107.8 KB).
Figure 1 .
Four highest scoring monitoring options: estimated average annual costs (based on 10 year forecast and 6% annual discount rate). CHD, coronary heart disease; QoL, quality of life; PF, patient function surveys; RF, risk factor surveys.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Breen D. Setting priorities: a framework for the assessment of health care priorities in Scottish Health Boards. Health Bull (Edinb) 1991 Jan;49(1):34–39. [PubMed] [Google Scholar]
- Briggs A., Sculpher M., Buxton M. Uncertainty in the economic evaluation of health care technologies: the role of sensitivity analysis. Health Econ. 1994 Mar-Apr;3(2):95–104. doi: 10.1002/hec.4730030206. [DOI] [PubMed] [Google Scholar]
- Carleton R. A., Lasater T. M., Assaf A., Lefebvre R. C., McKinlay S. M. The Pawtucket Heart Health Program: I. An experiment in population-based disease prevention. R I Med J. 1987 Dec;70(12):533–538. [PubMed] [Google Scholar]
- DAWBER T. R., KANNEL W. B., LYELL L. P. An approach to longitudinal studies in a community: the Framingham Study. Ann N Y Acad Sci. 1963 May 22;107:539–556. doi: 10.1111/j.1749-6632.1963.tb13299.x. [DOI] [PubMed] [Google Scholar]
- Donaldson L. Registering a need. BMJ. 1992 Sep 12;305(6854):597–598. doi: 10.1136/bmj.305.6854.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farquhar J. W., Fortmann S. P., Maccoby N., Haskell W. L., Williams P. T., Flora J. A., Taylor C. B., Brown B. W., Jr, Solomon D. S., Hulley S. B. The Stanford Five-City Project: design and methods. Am J Epidemiol. 1985 Aug;122(2):323–334. doi: 10.1093/oxfordjournals.aje.a114104. [DOI] [PubMed] [Google Scholar]
- Lock C. What value do computers provide to NHS hospitals? BMJ. 1996 Jun 1;312(7043):1407–1410. [PMC free article] [PubMed] [Google Scholar]
- Murray D. M. Design and analysis of community trials: lessons from the Minnesota Heart Health Program. Am J Epidemiol. 1995 Sep 15;142(6):569–575. doi: 10.1093/oxfordjournals.aje.a117677. [DOI] [PubMed] [Google Scholar]