Abstract
OBJECTIVE—To examine the reliability, validity, and responsiveness of a new health status measure (LVD-36) for patients with left ventricular dysfunction which was designed with emphasis on content validity, clarity, brevity, and ease of use. DESIGN—At baseline, patients completed the LVD-36 and a range of measures reflecting general health and disease severity. The LVD-36 was repeated after one week. After six months, it was repeated again, along with a transition question to measure global changes in health. SETTING—Patients were recruited from the cardiology and general medical clinics at a south west London hospital. PATIENTS—60 patients with chronic left ventricular dysfunction. INTERVENTIONS—None. MAIN OUTCOME MEASURES—Short form 36 questionnaire (SF-36), Minnesota living with heart failure questionnaire (LIhFE), New York Heart Association criteria, and exercise performance and echocardiographic tests. RESULTS—The LVD-36 showed good internal consistency (κ = 0.95) and repeatability (ri = 0.95). Its scores were significantly associated with SF-36 mental and physical component scores (r = −0.48 and −0.75; p < 0.0001), with exercise capacity (r = −0.52; p < 0.0001), and with systolic shortening fraction (r = −0.27; p < 0.05). Change in the LVD-36 over six months was associated with change in overall health (F = 5.7; p < 0.001). In tests of validity and responsiveness, the LVD-36 performed similarly to or marginally better than the LIhFE. CONCLUSIONS—The LVD-36 showed a high level of reliability and validity, and appears to measure changes in health. It provides a short, simple, valid, and reliable measure of health status in patients with left ventricular dysfunction. Keywords: health status; quality of life; heart failure; left ventricular dysfunction
Full Text
The Full Text of this article is available as a PDF (165.8 KB).
Figure 1 .
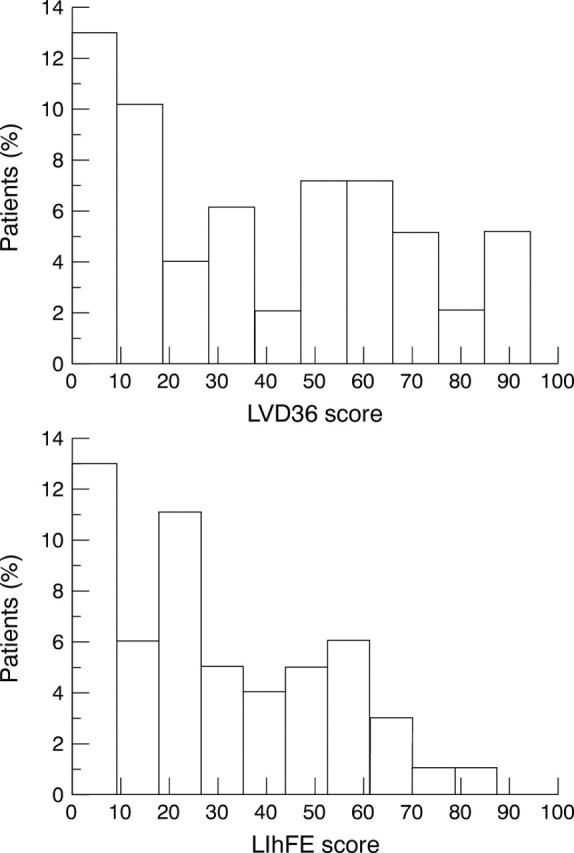
Histogram of LVD-36 and LIhFE scores.
Figure 2 .
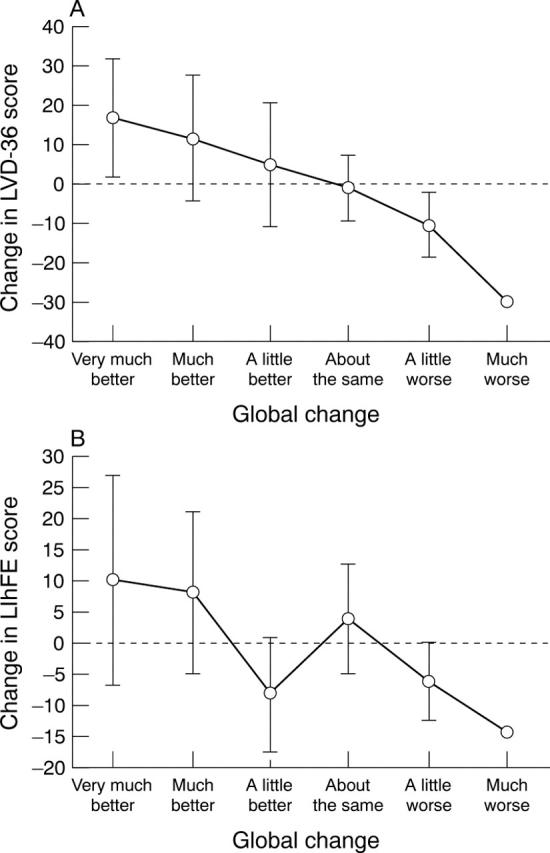
Association between the patients' score for global change and change in scores for (A) LVD-36 and (B) LIhFE over six months. Error bars show 95% confidence intervals.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Gardin J. M., Henry W. L., Savage D. D., Ware J. H., Burn C., Borer J. S. Echocardiographic measurements in normal subjects: evaluation of an adult population without clinically apparent heart disease. J Clin Ultrasound. 1979 Dec;7(6):439–447. doi: 10.1002/jcu.1870070606. [DOI] [PubMed] [Google Scholar]
- Goldman L., Hashimoto B., Cook E. F., Loscalzo A. Comparative reproducibility and validity of systems for assessing cardiovascular functional class: advantages of a new specific activity scale. Circulation. 1981 Dec;64(6):1227–1234. doi: 10.1161/01.cir.64.6.1227. [DOI] [PubMed] [Google Scholar]
- Guyatt G. H., Nogradi S., Halcrow S., Singer J., Sullivan M. J., Fallen E. L. Development and testing of a new measure of health status for clinical trials in heart failure. J Gen Intern Med. 1989 Mar-Apr;4(2):101–107. doi: 10.1007/BF02602348. [DOI] [PubMed] [Google Scholar]
- O'Leary C. J., Jones P. W. The influence of decisions made by developers on health status questionnaire content. Qual Life Res. 1998 Aug;7(6):545–550. doi: 10.1023/a:1008882626075. [DOI] [PubMed] [Google Scholar]
- Wiklund I., Lindvall K., Swedberg K., Zupkis R. V. Self-assessment of quality of life in severe heart failure. An instrument for clinical use. Scand J Psychol. 1987;28(3):220–225. doi: 10.1111/j.1467-9450.1987.tb00758.x. [DOI] [PubMed] [Google Scholar]


