Abstract
OBJECTIVE—To assess whether the use of inverted lead aVR (−aVR) would improve the classification of acute inferior or lateral myocardial infarction presenting with ST elevation. DESIGN—Observational study. The presence of ⩾ 1 mm ST elevation in lead −aVR (derived by manual assessment of ST depression in conventional lead aVR) was determined by a single investigator, blinded to patient outcome. PATIENTS—173 consecutive patients with chest pain for ⩽ 12 hours and ST elevation of ⩾ 1 mm in inferior leads (II, III, aVF) or lateral leads (I, aVL, V5, V6), excluding those with anterolateral ST elevation. MAIN OUTCOME MEASURE—Incidence of ST elevation in lead −aVR in patients with inferior or lateral ST elevation, or both. RESULTS—ST elevation in lead −aVR was present in 25 of 136 patients (18%) with inferior but no lateral ST elevation (indicating greater superior involvement) and in three of 11 patients (27%) with lateral but no inferior ST elevation (indicating greater inferior involvement). ST elevation in lead −aVR bridged the gap between inferior and lateral ST elevation in 15 of 25 (60%) patients with inferior and lateral chest lead (V5/V6) ST elevation, and in all patients with inferior and lateral limb lead (I/aVL) ST elevation. The presence of ST elevation in lead −aVR was associated with a larger infarct size as defined by median peak creatine kinase on serial sampling: 1780 v 987 mmol/l; p = 0.021. CONCLUSIONS—Use of lead −aVR improves the ECG classification of acute inferior or lateral acute myocardial infarction and thus may be useful as part of the routine 12 lead ECG assessment of such patients. Keywords: electrocardiography; acute myocardial infarction
Full Text
The Full Text of this article is available as a PDF (146.7 KB).
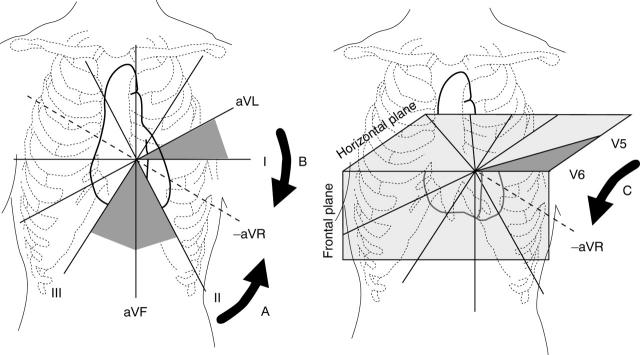
Figure 1 .
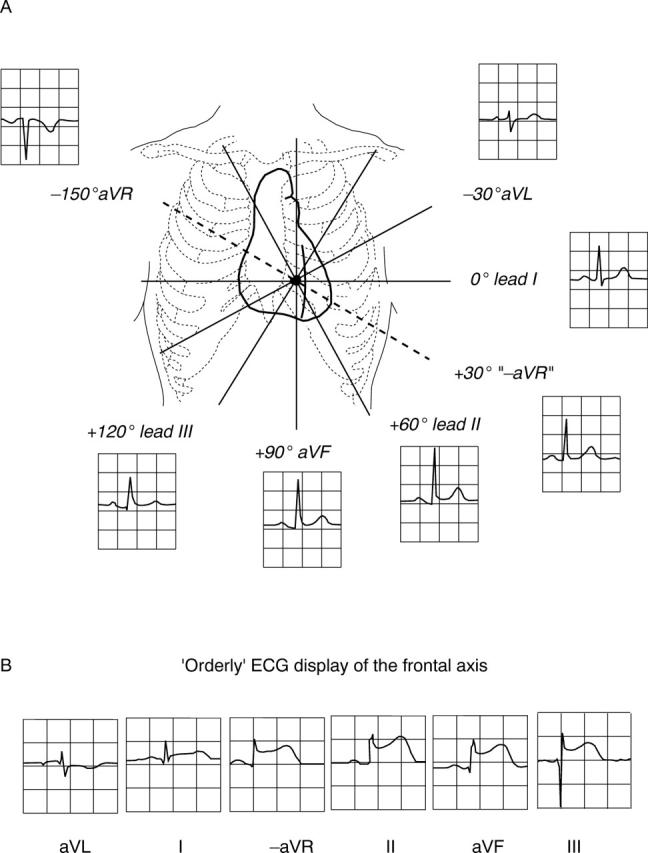
(A) Frontal axis illustrating individual leads including conventional and inverted aVR. (B) An orderly ECG display of the frontal axis in a patient with acute inferolateral myocardial infarction incorporating −aVR, arranged in 30° intervals from aVL to lead III. A sequential rise and fall in ST segment height is seen as the leads circle the apex of the left ventricle.
Figure 2 .
Diagrammatic illustration of ST elevation in lead −aVR indicating a greater superior involvement in patients with acute inferior ST elevation (arrow A), and a greater inferior involvement in patients with acute lateral limb lead ST elevation (arrow B) or lateral chest lead ST elevation (arrow C).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson S. T., Pahlm O., Selvester R. H., Bailey J. J., Berson A. S., Barold S. S., Clemmensen P., Dower G. E., Elko P. P., Galen P. Panoramic display of the orderly sequenced 12-lead ECG. J Electrocardiol. 1994 Oct;27(4):347–352. doi: 10.1016/s0022-0736(05)80275-4. [DOI] [PubMed] [Google Scholar]
- Dower G. E., Nazzal S. B., Pahlm O., Haistey W. K., Jr, Marriott H. L., Bullington R. H., Bullington D. Limb leads of the electrocardiogram: sequencing revisited. Clin Cardiol. 1990 May;13(5):346–348. doi: 10.1002/clc.4960130508. [DOI] [PubMed] [Google Scholar]
- Gambill C. L., Wilkins M. L., Haisty W. K., Jr, Anderson S. T., Maynard C., Wagner N. B., Selvester R. H., Wagner G. S. T wave amplitudes in normal populations. Variation with ECG lead, sex, and age. J Electrocardiol. 1995 Jul;28(3):191–197. doi: 10.1016/s0022-0736(05)80257-2. [DOI] [PubMed] [Google Scholar]
- Pahlm U. S., Pahlm O., Wagner G. S. The standard 11-lead ECG. Neglect of lead aVR in the classical limb lead display. J Electrocardiol. 1996;29 (Suppl):270–274. doi: 10.1016/s0022-0736(96)80074-4. [DOI] [PubMed] [Google Scholar]
- Viik J., Lehtinen R., Turjanmaa V., Niemelä K., Malmivuo J. Correct utilization of exercise electrocardiographic leads in differentiation of men with coronary artery disease from patients with a low likelihood of coronary artery disease using peak exercise ST-segment depression. Am J Cardiol. 1998 Apr 15;81(8):964–969. doi: 10.1016/s0002-9149(98)00073-3. [DOI] [PubMed] [Google Scholar]
- Viik J., Lehtinen R., Turjanmaa V., Niemelä K., Malmivuo J. The effect of lead selection on traditional and heart rate-adjusted ST segment analysis in the detection of coronary artery disease during exercise testing. Am Heart J. 1997 Sep;134(3):488–494. doi: 10.1016/s0002-8703(97)70086-3. [DOI] [PubMed] [Google Scholar]