Abstract
Transient abnormalities in ECGs, echocardiograms, and cardiac enzymes have been described in the acute setting of subarachnoid haemorrhage. In addition, left ventricular dysfunction has been reported at the time of brain death. A patient with an acute subarachnoid haemorrhage who presented with raised troponin I (TnI) concentrations and diffuse left ventricular dysfunction is described. After declaration of brain death 32 hours later, the heart was felt initially not suitable for transplantation. A normal cardiac catheterisation, however, lead to successful transplantation of the donor heart. Raised catecholamine concentrations and metabolic perturbations have been proposed as the mechanisms leading to the cardiac dysfunction seen with brain death. This may be a biphasic process, allowing time for myocardial recovery and reversal of the left ventricular dysfunction. Awareness of this phenomenon in the acutely ill neurologic population needs to be raised in order to prevent the unnecessary rejection of donor hearts. Keywords: heart transplantation; troponin I; left ventricular dysfunction
Full Text
The Full Text of this article is available as a PDF (121.6 KB).
Figure 1 .
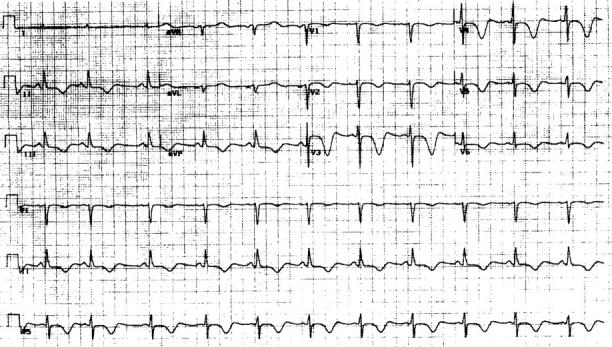
EGG recorded within 24 hours of onset of subarachnoid haemorrhage. Note the inverted T waves in leads II, III, AVF, V2, V3, V4, V5, and V6. In addition, there is ST segment elevation in V3, V4, and V5. These findings are common ECG abnormalities following subarachnoid haemorrhage.
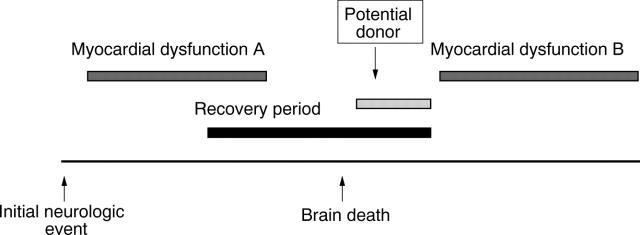
Figure 2 .
As proposed by Novitzky, myocardial dysfunction at the time of brain death may consist of two physiologic processes.9 An initial injury is caused by a high catecholamine state (myocardial dysfunction A), and a second injury is induced by metabolic perturbations (myocardial dysfunction B). We propose that these two processes do not necessarily occur contiguously, but instead occur as a biphasic phenomenon allowing for a period of myocardial recovery. If appropriate haemodynamic support is given, the second metabolic induced injury could be delayed, allowing a window of opportunity for successful organ procurement.