Abstract
Aims: To compare the clinical efficacy of twice daily oral co-trimoxazole with twice daily oral amoxicillin for treatment of childhood pneumonia.
Methods: Randomised controlled, double blind, multicentre study in outpatient departments of seven hospitals and in one community health service. A total of 1471 children (aged 2–59 months) with non-severe pneumonia were randomly assigned to 25 mg/kg amoxicillin (n = 730) or 4 mg/kg trimethoprim plus 20 mg/kg sulphamethoxazole (co-trimoxazole) (n = 741). Both medicines were given orally twice daily for five days.
Results: Data from 1459 children were analysed: 725 were randomised to amoxicillin and 734 to co-trimoxazole. Treatment failure in the amoxicillin group was 16.1% compared to 18.9% in the co-trimoxazole group. Multivariate analysis showed that treatment failure was more likely in infants who had history of difficult breathing or those who had been ill for more than three days before presentation.
Conclusions: Both amoxicillin and co-trimoxazole were equally effective in non-severe pneumonia. Good follow up of patients is essential to prevent worsening of illness.
Full Text
The Full Text of this article is available as a PDF (135.3 KB).
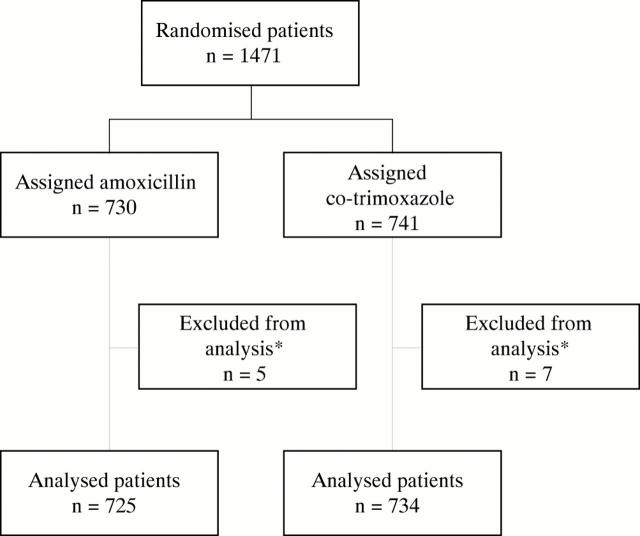
Figure 1 .
Trial profile. *These patients did not fulfil enrolment criteria.
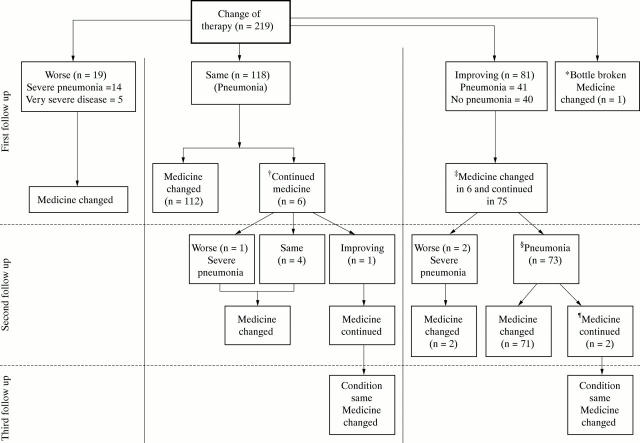
Figure 2 .
Details of patients needing a change in antibiotic therapy (n = 219). *One study bottle was broken and medicine was changed to chloramphenicol; †4 were non-compliant and 2 looked clinically well; ‡3 looked sick clinically, 1 developed rash, and the mothers of 2 were very apprehensive and wanted therapy changed; §6 had improved clinically but respiratory rate was still above age specific cut off value. 5 children also had wheezing; ¶in both the respiratory rate was on borderline age specific cut off value, so treatment was continued.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bettenay F. A., de Campo J. F., McCrossin D. B. Differentiating bacterial from viral pneumonias in children. Pediatr Radiol. 1988;18(6):453–454. doi: 10.1007/BF00974077. [DOI] [PubMed] [Google Scholar]
- Calver A. D., Walsh N. S., Quinn P. F., Baran C., Lonergan V., Singh K. P., Orzolek W. S. Dosing of amoxicillin/clavulanate given every 12 hours is as effective as dosing every 8 hours for treatment of lower respiratory tract infection. Lower Respiratory Tract Infection Collaborative Study Group. Clin Infect Dis. 1997 Apr;24(4):570–574. doi: 10.1093/clind/24.4.570. [DOI] [PubMed] [Google Scholar]
- Cook R. C., Zachariah J., Cree F., Harrison H. E. Efficacy of twice-daily amoxycillin/clavulanate ('Augmentin-Duo' 400/57) in mild to moderate lower respiratory tract infection in children. Br J Clin Pract. 1996 Apr-May;50(3):125–128. [PubMed] [Google Scholar]
- Courtoy I., Lande A. E., Turner R. B. Accuracy of radiographic differentiation of bacterial from nonbacterial pneumonia. Clin Pediatr (Phila) 1989 Jun;28(6):261–264. doi: 10.1177/000992288902800604. [DOI] [PubMed] [Google Scholar]
- Daschner F. D., Behre U., Dalhoff A. Prospective clinical trial on the efficacy of amoxycillin administered twice or four times daily in children with respiratory tract infections. J Int Med Res. 1981;9(4):274–276. doi: 10.1177/030006058100900407. [DOI] [PubMed] [Google Scholar]
- Deeks S. L., Palacio R., Ruvinsky R., Kertesz D. A., Hortal M., Rossi A., Spika J. S., Di Fabio J. L. Risk factors and course of illness among children with invasive penicillin-resistant Streptococcus pneumoniae. The Streptococcus pneumoniae Working Group. Pediatrics. 1999 Feb;103(2):409–413. doi: 10.1542/peds.103.2.409. [DOI] [PubMed] [Google Scholar]
- Drusano G. L. Role of pharmacokinetics in the outcome of infections. Antimicrob Agents Chemother. 1988 Mar;32(3):289–297. doi: 10.1128/aac.32.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fassl A., Muhr R., Pirker S., Nahler G. Amoxycillin in bronchitis. Comparison of two versus three daily doses. J Int Med Res. 1987 Mar-Apr;15(2):76–82. doi: 10.1177/030006058701500203. [DOI] [PubMed] [Google Scholar]
- Feder H. M., Jr, Gerber M. A., Randolph M. F., Stelmach P. S., Kaplan E. L. Once-daily therapy for streptococcal pharyngitis with amoxicillin. Pediatrics. 1999 Jan;103(1):47–51. doi: 10.1542/peds.103.1.47. [DOI] [PubMed] [Google Scholar]
- Forgie I. M., O'Neill K. P., Lloyd-Evans N., Leinonen M., Campbell H., Whittle H. C., Greenwood B. M. Etiology of acute lower respiratory tract infections in Gambian children: I. Acute lower respiratory tract infections in infants presenting at the hospital. Pediatr Infect Dis J. 1991 Jan;10(1):33–41. doi: 10.1097/00006454-199101000-00008. [DOI] [PubMed] [Google Scholar]
- Gauderer M. W., Crane M. M., Green J. A., DeCou J. M., Abrams R. S. Acute appendicitis in children: the importance of family history. J Pediatr Surg. 2001 Aug;36(8):1214–1217. doi: 10.1053/jpsu.2001.25765. [DOI] [PubMed] [Google Scholar]
- Ghafoor A., Nomani N. K., Ishaq Z., Zaidi S. Z., Anwar F., Burney M. I., Qureshi A. W., Ahmad S. A. Diagnoses of acute lower respiratory tract infections in children in Rawalpindi and Islamabad, Pakistan. Rev Infect Dis. 1990 Nov-Dec;12 (Suppl 8):S907–S914. doi: 10.1093/clinids/12.supplement_8.s907. [DOI] [PubMed] [Google Scholar]
- Khan M. A., Qazi S. A., Rehman G. N., Bari A. A community study of the application of WHO ARI management guidelines in Pakistan. Ann Trop Paediatr. 1993;13(1):73–78. doi: 10.1080/02724936.1993.11747627. [DOI] [PubMed] [Google Scholar]
- Mastro T. D., Ghafoor A., Nomani N. K., Ishaq Z., Anwar F., Granoff D. M., Spika J. S., Thornsberry C., Facklam R. R. Antimicrobial resistance of pneumococci in children with acute lower respiratory tract infection in Pakistan. Lancet. 1991 Jan 19;337(8734):156–159. doi: 10.1016/0140-6736(91)90813-5. [DOI] [PubMed] [Google Scholar]
- Mastro T. D., Nomani N. K., Ishaq Z., Ghafoor A., Shaukat N. F., Esko E., Leinonen M., Henrichsen J., Breiman R. F., Schwartz B. Use of nasopharyngeal isolates of Streptococcus pneumoniae and Haemophilus influenzae from children in Pakistan for surveillance for antimicrobial resistance. Pediatr Infect Dis J. 1993 Oct;12(10):824–830. doi: 10.1097/00006454-199310000-00006. [DOI] [PubMed] [Google Scholar]
- Mulholland E. K., Simoes E. A., Costales M. O., McGrath E. J., Manalac E. M., Gove S. Standardized diagnosis of pneumonia in developing countries. Pediatr Infect Dis J. 1992 Feb;11(2):77–81. doi: 10.1097/00006454-199202000-00004. [DOI] [PubMed] [Google Scholar]
- Pallares R., Liñares J., Vadillo M., Cabellos C., Manresa F., Viladrich P. F., Martin R., Gudiol F. Resistance to penicillin and cephalosporin and mortality from severe pneumococcal pneumonia in Barcelona, Spain. N Engl J Med. 1995 Aug 24;333(8):474–480. doi: 10.1056/NEJM199508243330802. [DOI] [PubMed] [Google Scholar]
- Qazi S. A. Antibiotic strategies for developing countries: experience with acute respiratory tract infections in Pakistan. Clin Infect Dis. 1999 Feb;28(2):214–218. doi: 10.1086/515124. [DOI] [PubMed] [Google Scholar]
- Ríos A. M., de la Hoz F., Leal A. L., Castillo O., Castañeda E. Impacto de la resistencia a antimicrobianos y de serotipos de Streptococcus pneumoniae en la mortalidad de niños menores de 5 años con enfermedad invasora. Rev Panam Salud Publica. 1999 Feb;5(2):69–76. doi: 10.1590/s1020-49891999000200001. [DOI] [PubMed] [Google Scholar]
- Sazawal S., Black R. E. Meta-analysis of intervention trials on case-management of pneumonia in community settings. Lancet. 1992 Aug 29;340(8818):528–533. doi: 10.1016/0140-6736(92)91720-s. [DOI] [PubMed] [Google Scholar]
- Shvartzman P., Tabenkin H., Rosentzwaig A., Dolginov F. Treatment of streptococcal pharyngitis with amoxycillin once a day. BMJ. 1993 May 1;306(6886):1170–1172. doi: 10.1136/bmj.306.6886.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus W. L., Qazi S. A., Kundi Z., Nomani N. K., Schwartz B. Antimicrobial resistance and clinical effectiveness of co-trimoxazole versus amoxycillin for pneumonia among children in Pakistan: randomised controlled trial. Pakistan Co-trimoxazole Study Group. Lancet. 1998 Jul 25;352(9124):270–274. doi: 10.1016/s0140-6736(97)10294-x. [DOI] [PubMed] [Google Scholar]
- Tupasi T. E., Lucero M. G., Magdangal D. M., Mangubat N. V., Sunico M. E., Torres C. U., de Leon L. E., Paladin J. F., Baes L., Javato M. C. Etiology of acute lower respiratory tract infection in children from Alabang, Metro Manila. Rev Infect Dis. 1990 Nov-Dec;12 (Suppl 8):S929–S939. doi: 10.1093/clinids/12.supplement_8.s929. [DOI] [PubMed] [Google Scholar]
- Valtonen M., Piippo T., Pitkäjärvi T., Pyykönen M. L. Comparison of amoxycillin given two and three times a day in acute respiratory tract infections in children. Scand J Prim Health Care. 1986 Nov;4(4):201–204. doi: 10.3109/02813438609014831. [DOI] [PubMed] [Google Scholar]