Abstract
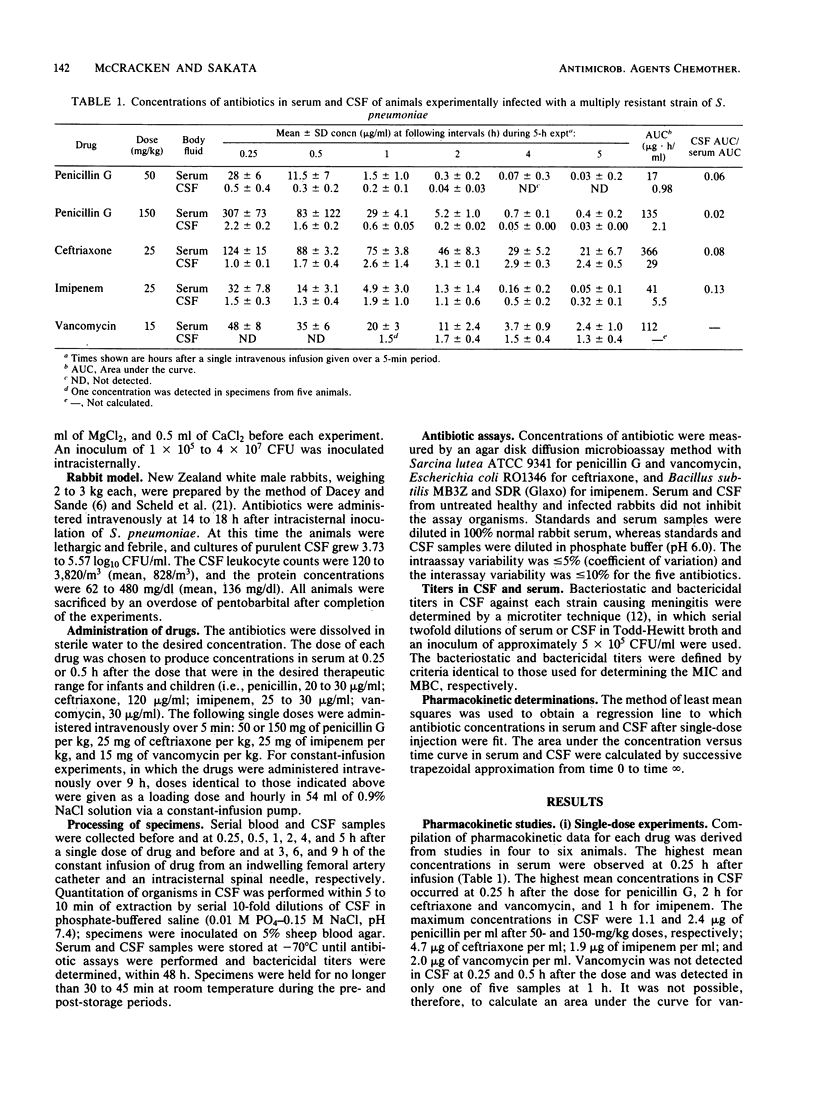
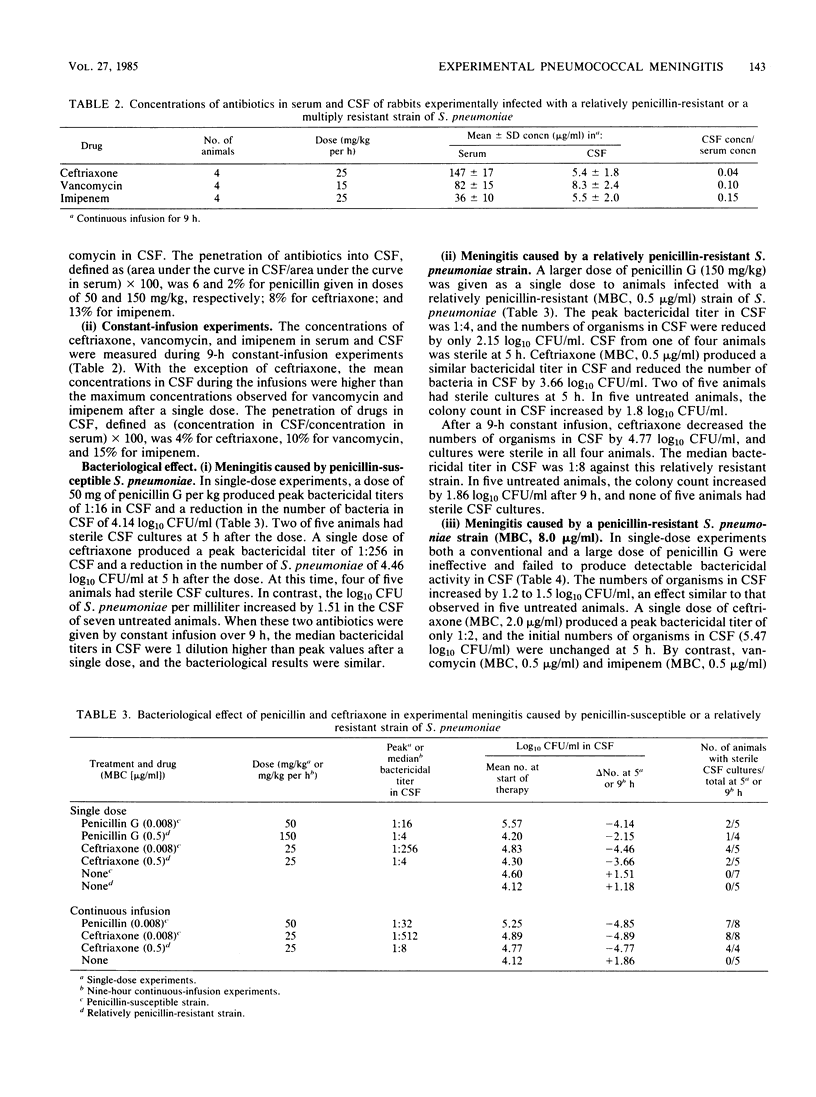
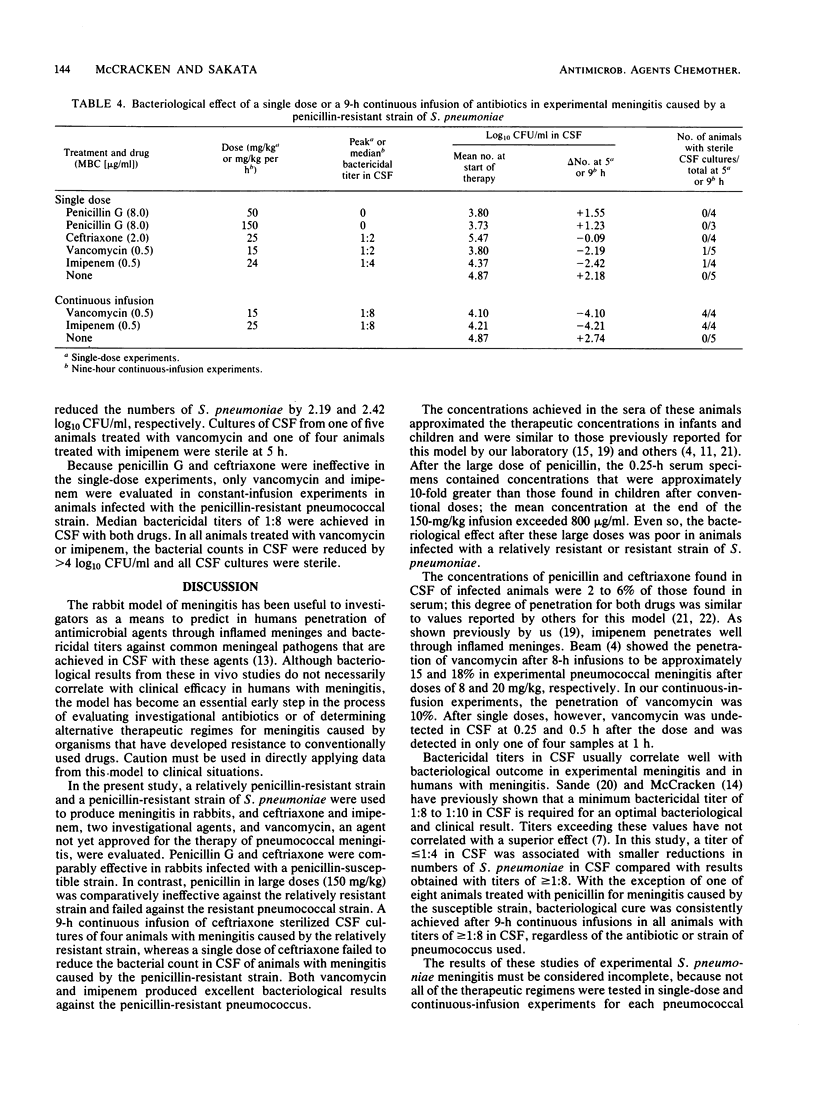
The pharmacokinetics and bacteriological efficacies of penicillin G, ceftriaxone, vancomycin, and imipenem were determined in rabbits with experimental meningitis caused by Streptococcus pneumoniae strains with different penicillin susceptibilities. Drug dosages were adjusted to attain peak concentrations in serum that were similar to those observed in infants and children. In animals infected with a penicillin-susceptible (MBC, 0.008 micrograms/ml) pneumococcus, penicillin G and ceftriaxone reduced the number of organisms in cerebrospinal fluid (CSF) by greater than or equal to 4.14 log10 CFU/ml after single doses and after 9-h continuous infusions. A single large dose (50 mg/kg) of penicillin G was comparatively ineffective (-2.15 log10 CFU/ml) against a relatively penicillin-resistant (MBC, 0.5 micrograms/ml) strain, whereas ceftriaxone therapy resulted in a 3.66- and 4.77-log10 CFU/ml reduction after single doses and 9-h continuous infusions, respectively. In animals in which meningitis was caused by a penicillin-resistant (MBC, 8.0 micrograms/ml) pneumococcus, a single dose of penicillin (50 or 150 mg/kg) or of ceftriaxone failed to lower the number of organisms in CSF. Vancomycin and imipenem reduced the counts in CSF by at least 2.19 and 4.10 log10 CFU/ml after single doses and 9-h infusions, respectively. In all experiments, a bactericidal titer of greater than or equal to 1:8 in CSF was necessary to achieve a maximal bacteriological effect.
Full text
PDF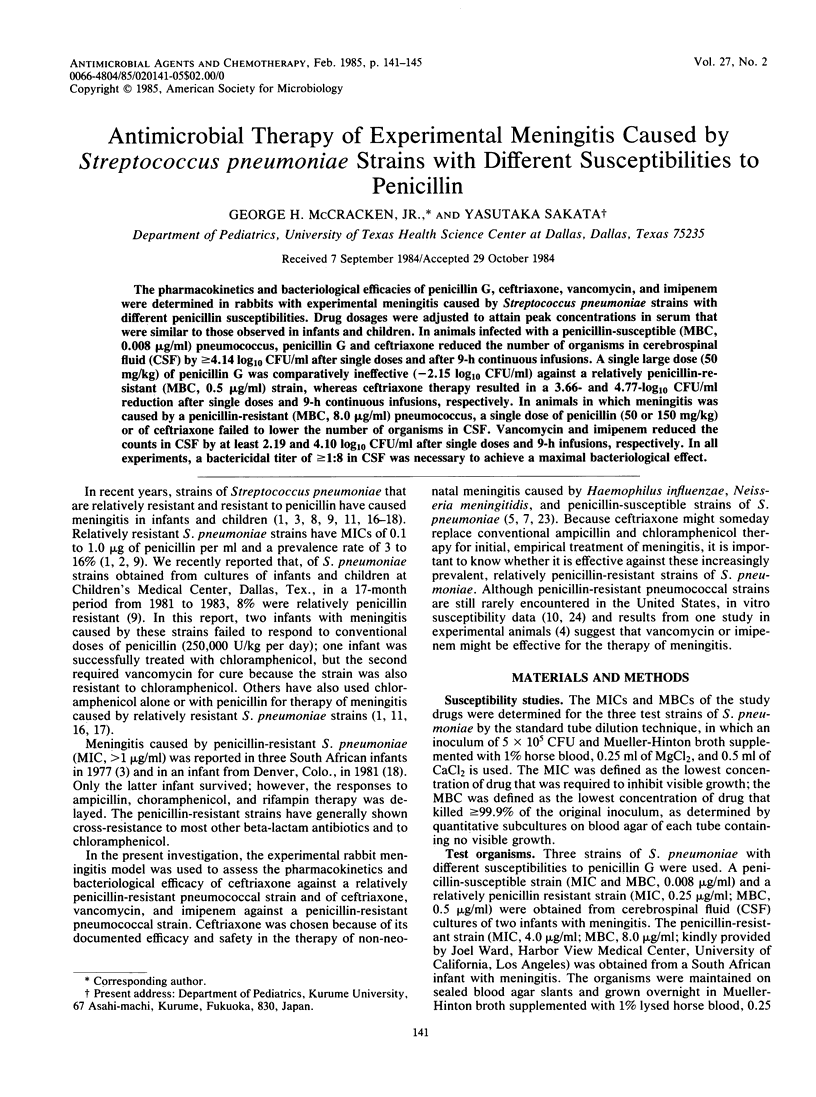

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahronheim G. A., Reich B., Marks M. I. Penicillin-insensitive pneumococci. Case report and review. Am J Dis Child. 1979 Feb;133(2):187–191. doi: 10.1001/archpedi.1979.02130020079017. [DOI] [PubMed] [Google Scholar]
- Anderson K. C., Maurer M. J., Dajani A. S. Pneumococci relatively resistant to penicillin: a prevalence survey in children. J Pediatr. 1980 Dec;97(6):939–941. doi: 10.1016/s0022-3476(80)80426-4. [DOI] [PubMed] [Google Scholar]
- Appelbaum P. C., Bhamjee A., Scragg J. N., Hallett A. F., Bowen A. J., Cooper R. C. Streptococcus pneumoniae resistant to penicillin and chloramphenicol. Lancet. 1977 Nov 12;2(8046):995–997. doi: 10.1016/s0140-6736(77)92892-6. [DOI] [PubMed] [Google Scholar]
- Beam T. R. Vancomycin therapy of experimental pneumococcal meningitis caused by penicillin-sensitive and resistant strains. J Antimicrob Chemother. 1981 Jan;7(1):89–99. doi: 10.1093/jac/7.1.89. [DOI] [PubMed] [Google Scholar]
- Congeni B. L. Comparison of ceftriaxone and traditional therapy of bacterial meningitis. Antimicrob Agents Chemother. 1984 Jan;25(1):40–44. doi: 10.1128/aac.25.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dacey R. G., Sande M. A. Effect of probenecid on cerebrospinal fluid concentrations of penicillin and cephalosporin derivatives. Antimicrob Agents Chemother. 1974 Oct;6(4):437–441. doi: 10.1128/aac.6.4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devitt L., Riley I., Hansman D. Human infection caused by penicillin-insensitive pneumococci. Med J Aust. 1977 Apr 16;1(16):586–588. doi: 10.5694/j.1326-5377.1977.tb130925.x. [DOI] [PubMed] [Google Scholar]
- Jackson M. A., Shelton S., Nelson J. D., McCracken G. H., Jr Relatively penicillin-resistant pneumococcal infections in pediatric patients. Pediatr Infect Dis. 1984 Mar-Apr;3(2):129–132. doi: 10.1097/00006454-198403000-00010. [DOI] [PubMed] [Google Scholar]
- Landesman S. H., Cummings M., Gruarin A., Bernheimer H. Susceptibility of multiply antibiotic-resistant pneumococci to the new beta-lactam drugs and rosaramicin. Antimicrob Agents Chemother. 1981 Apr;19(4):675–677. doi: 10.1128/aac.19.4.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mace J. W., Janik D. S., Sauer R. L., Quilligan J. J., Jr Penicillin-resistant pneumococcal meningitis in an immunocompromised infant. J Pediatr. 1977 Sep;91(3):506–507. doi: 10.1016/s0022-3476(77)81339-5. [DOI] [PubMed] [Google Scholar]
- Marymont J. H., Jr, Wentz R. M. Serial dilution antibiotic sensitivity testing with the microtitrator system. Am J Clin Pathol. 1966 May;45(5):548–551. doi: 10.1093/ajcp/45.5.548. [DOI] [PubMed] [Google Scholar]
- McCracken G. H., Jr Management of bacterial meningitis in infants and children. Current status and future prospects. Am J Med. 1984 May 15;76(5A):215–223. doi: 10.1016/0002-9343(84)90267-5. [DOI] [PubMed] [Google Scholar]
- McCracken G. H., Jr, Nelson J. D., Grimm L. Pharmacokinetics and bacteriological efficacy of cefoperazone, ceftriaxone, and moxalactam in experimental Streptococcus pneumoniae and Haemophilus influenzae meningitis. Antimicrob Agents Chemother. 1982 Feb;21(2):262–267. doi: 10.1128/aac.21.2.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken G. H., Jr Pharmacokinetic and bacteriological correlations between antimicrobial therapy of experimental meningitis in rabbits and meningitis in humans: a review. J Antimicrob Chemother. 1983 Dec;12 (Suppl 500):97–108. doi: 10.1093/jac/12.suppl_d.97. [DOI] [PubMed] [Google Scholar]
- Naraqi S., Kirkpatrick G. P., Kabins S. Relapsing pneumococcal meningitis: isolation of an organism with decreased susceptibility to penicillin G. J Pediatr. 1974 Nov;85(5):671–673. doi: 10.1016/s0022-3476(74)80513-5. [DOI] [PubMed] [Google Scholar]
- Paredes A., Taber L. H., Yow M. D., Clark D., Nathan W. Prolonged pneumococcal meningitis due to an organism with increased resistance to penicillin. Pediatrics. 1976 Sep;58(3):378–381. [PubMed] [Google Scholar]
- Radetsky M. S., Istre G. R., Johansen T. L., Parmelee S. W., Lauer B. A., Wiesenthal A. M., Glode M. P. Multiply resistant pneumococcus causing meningitis: its epidemiology within a day-care centre. Lancet. 1981 Oct 10;2(8250):771–773. doi: 10.1016/s0140-6736(81)90184-7. [DOI] [PubMed] [Google Scholar]
- Sakata Y., McCracken G. H., Jr, Thomas M. L., Olsen K. D. Pharmacokinetics and therapeutic efficacy of imipenem, ceftazidime, and ceftriaxone in experimental meningitis due to an ampicillin- and chloramphenicol-resistant strain of Haemophilus influenzae type b. Antimicrob Agents Chemother. 1984 Jan;25(1):29–32. doi: 10.1128/aac.25.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sande M. A. Antibiotic therapy of bacterial meningitis: lessons we've learned. Am J Med. 1981 Oct;71(4):507–510. doi: 10.1016/0002-9343(81)90191-1. [DOI] [PubMed] [Google Scholar]
- Scheld W. M., Brodeur J. P., Sande M. A., Alliegro G. M. Comparison of cefoperazone with penicillin, ampicillin, gentamicin, and chloramphenicol in the therapy of experimental meningitis. Antimicrob Agents Chemother. 1982 Oct;22(4):652–656. doi: 10.1128/aac.22.4.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheretz R. J., Dacey R., Sande M. A. Cefamandole in the therapy of experimental pneumococcal meningitis. J Antimicrob Chemother. 1976 Jun;2(2):159–165. doi: 10.1093/jac/2.2.159. [DOI] [PubMed] [Google Scholar]
- Steele R. W., Bradsher R. W. Comparison of ceftriaxone with standard therapy for bacterial meningitis. J Pediatr. 1983 Jul;103(1):138–141. doi: 10.1016/s0022-3476(83)80801-4. [DOI] [PubMed] [Google Scholar]
- Ward J. I., Moellering R. C., Jr Susceptibility of pneumococci to 14 beta-lactam agents: comparison of strains resistant, intermediate-resistant, and susceptible to penicillin. Antimicrob Agents Chemother. 1981 Aug;20(2):204–207. doi: 10.1128/aac.20.2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Rio M. A., Chrane D., Shelton S., McCracken G. H., Jr, Nelson J. D. Ceftriaxone versus ampicillin and chloramphenicol for treatment of bacterial meningitis in children. Lancet. 1983 Jun 4;1(8336):1241–1244. doi: 10.1016/s0140-6736(83)92696-x. [DOI] [PubMed] [Google Scholar]



