Abstract
Converging evidence suggests that high levels of education and intellectual activity increase the cognitive reserve and reduce the risk of dementia. However, little is known about the impact that different neuroprotective strategies may have on the incidence of Alzheimer's disease. Using a simple mathematical regression model, it is shown here that age-specific counts of basic cognitive units (surrogate of neurons or synapses) in the normal population can be estimated from Alzheimer's incidence rates. Hence, the model can be used to test the effect of neuroprotection on Alzheimer's incidence. It was found that the number of basic cognitive units decreases with age, but levels off in older people. There were no gender differences after correcting for survival. The model shows that even modest neuroprotective effects on basic cognitive units can lead to dramatic reductions in the number of Alzheimer's cases. Most remarkably, a 5% increase in the cognitive reserve would prevent one third of Alzheimer's cases. These results suggest that public health policies aimed at increasing the cognitive reserve in the general population (e.g., implementing higher levels of education) are likely the most effective strategy for preventing Alzheimer's disease.
Introduction
There is concern that the progressive loss of neurons and synapses with age may lead to dramatic increases in incidence rates of late-onset Alzheimer's disease in future generations with greater longevity [1]. However, while there is substantial evidence that normal aging is associated with some cognitive impairment, the relationship between Alzheimer's disease, normal aging, and brain function is still far from clear [2]–[5]. It has been shown that most people accumulate Alzheimer-related lesions with age [6], but there is still controversy as to whether neuron death (or synapse density loss) is an inevitable result of normal aging [7]. Conversely, advanced Alzheimer's pathology is sometimes associated with normal cognition [8]. These observations highlight a considerable disjunction between pathology and function in the aging brain, and support the notion that the cognitive reserve plays a crucial role in modifying the relationship between pathology and cognitive function [9], [10]. Indeed, there is converging evidence that education and cognitive activity have protective effects on cognition, reducing the risk of dementia [11]–[14].
The main objective of this study was to evaluate the effect of neuroprotection on Alzheimer's disease incidence. From a functional viewpoint, normal cognition depends on the contribution of a number of basic cognitive units (BCU), which may represent neurons, synapses or cerebral circuits (biological units). The cognitive reserve refers to the number of BCU an individual has to lose before developing dementia symptoms [10]. Age-specific incidence rates of Alzheimer's disease reflect the instantaneous probability of BCU counts dropping below a certain threshold, which separates normal cognition from dementia. Consequently, reported incidence rates of Alzheimer's disease can be used to model and ‘visualize’ the effect of aging on BCU counts in the normal (living) population. Most importantly, this simple mathematical model offers a unique method to estimate the effect of neuroprotection on Alzheimer's disease incidence. Several observations support the model: 1) Virtually the entire population has Alzheimer-related pathology (amyloid plaques and neurofibrillary tangles) by age 90 years [6]; 2) The hippocampus is targeted by both normal aging and Alzheimer's disease [7]; and 3) Synapse density loss seems to be the major correlate of cognitive impairment in both normal aging and Alzheimer's disease [11].
Methods
Data: Epidemiological studies
A Medline/PubMed search of the English literature between 1966 and the end of 2005 identified 26 studies on the incidence of Alzheimer's disease that met the inclusion criteria. Studies were selected according to the following inclusion criteria: 1) Case finding was based on a field survey with population-based samples; 2) Males and females were included in the study; 3) Age-specific incidence rates of Alzheimer's disease were reported for dementia from mild to severe; 4) Standard errors of incidence rates were reported or could be calculated from the reported data. There were 11 studies from Europe [15]–[25], 8 studies from North America [26]–[33], 4 studies from Asia [34]–[37], 1 study from Africa [38], 1 study from Australia [39], and 1 study from South America [40]. Sixteen studies included specific data for women and men. Some of these 26 studies were included in previous meta-analyses and review articles [41]–[45].
Mathematical model
The model assumes that 1) BCU counts are approximately normally distributed at any given age, and 2) Alzheimer's disease occurs when BCU counts drop below a certain threshold value (symptom threshold). Therefore, as incidence rates of Alzheimer's disease represent the probability (p) of failure in cognition at any given age, age-specific z-scores can be directly obtained from these p values. Re-arranging the formula of the z-score, the following equation is obtained: E(y|x) = c−z-score×SD(y|x), where c represents the symptom threshold, E(y|x) is the expected BCU count (y) at any given age (x), and SD(y|x) is the corresponding standard deviation.
It should be noted that post-mortem studies support the model assumption that BCU counts are approximately normally distributed at any given age, and suggest that Alzheimer's symptoms appear when the BCU count drops to about 50% the normal value at an early age (say, age 20 years) [11], [46]–[51]. Hence, the BCU count can be expressed as a proportion, using c = 0.5 as the most likely threshold value. Regression analyses of previous post-mortem studies also suggest that SD(y|x) = 0.1 is the most likely value for the standard deviation. Consequently, the final equation is E(y|x) = BCU|age = 0.5−0.1×z-score. Sensitivity analyses were carried out to evaluate the effect of changing these parameter values.
Statistical analysis
Average annual age-specific incidence rates of Alzheimer's disease (per 1,000 person-years) were estimated from the reported incidence rates using two different non-parametric regression methods, loess and sm [52]–[54]. As rates are always restricted (i.e., they can only take positive values), a log transformation was used in the regression analysis, where log is the natural logarithm. The estimated age-specific average values were then converted back to the original scale, which gives the average p at any given age, from which the corresponding z-scores were directly obtained. These z-scores were then incorporated into the final equation BCU|age = 0.5−0.1×z-score, obtaining thus the BCU curve. The smoothing parameter was selected according to the cross-validation criterion in each regression analysis [52]–[54]. The inverse variances of log incidence rates of Alzheimer's disease were used as weights, which are proportional to the number of incident Alzheimer's cases [55]. The same non-parametric weighted regression methods were also applied to the different E(y|x) values obtained directly from the reported incidence rates for each study. Gender comparisons were performed using weighted non-parametric methods (sm ancova and generalized additive models using loess) [53].
Results
Estimates of basic cognitive units (BCU)
Non-parametric fits of log incidence rates of Alzheimer's disease on age (Fig. 1), and the corresponding BCU curves (Fig. 2), were found to depart significantly from linearity (sm regression, P<0.0001). Thus, BCU counts decrease with age in the normal population up to around age 85 years and then tend to level off. Sensitivity analysis demonstrated consistency in the overall pattern of the BCU curve i) after changing the values for c and SD, ii) using age-dependent SD values (either age-related increase or age-related decrease of SD), and iii) using non-constant sm smoothing parameters.
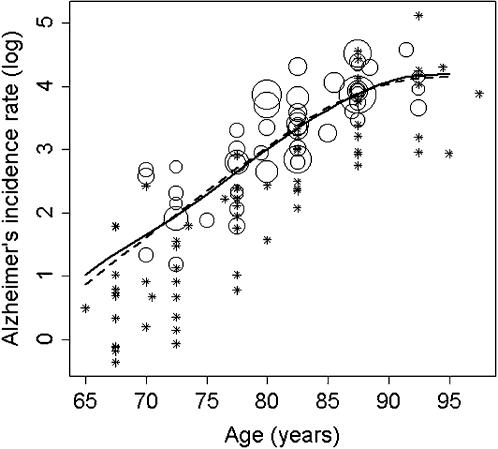
Figure 1. Non-parametric regression of the natural logarithm (log) of Alzheimer's incidence rates on age.
Rates were estimated per 1,000 person-years.
The diameter of the circles for each data point is proportional to the square root of the number of Alzheimer's cases.
For visibility, very small circles have been replaced by asterisks.
The solid and dashed curves were obtained by weighted non-parametric regression methods using sm and loess, respectively (see Methods); the smoothing parameter corresponded to span = 1 in both cases [52]–[54].
The two curves closely agree and depart significantly from a linear model (sm regression, P<0.0001).
There was no evidence for non-constant variance (score test, P = 0.88).
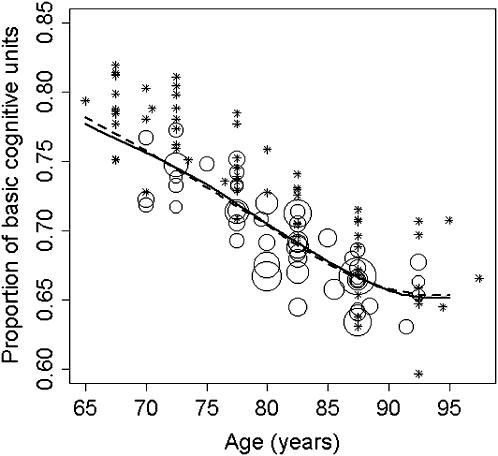
Figure 2. Non-parametric regression of the number of basic cognitive units (BCU) on age.
The BCU count is expressed as a proportion with respect to the average normal BCU count at an early age (say, age 20 years).
Again, circle sizes are proportional to the square root of the number of Alzheimer's cases, asterisks represent very small circles, the solid curve was obtained using sm, and the dashed curve was obtained using loess (span = 1).
Data points were directly derived from the z-scores associated with the corresponding Alzheimer's incidence rates, using the equation: BCU|age = 0.5−0.1× z-score, where the threshold (c) is 0.5, and the standard deviation (SD) is 0.1 (see Methods).
The plotted curves were derived from the average annual incidence rates of Alzheimer's disease (see Fig. 1), but virtually identical curves were obtained by direct weighted non-parametric regression of BCU points on age.
Again, both BCU curves closely agree and depart significantly from linearity (sm regression, P<0.0001).
Thus, BCU counts decrease with age up to approximately age 85 years, and then level off.
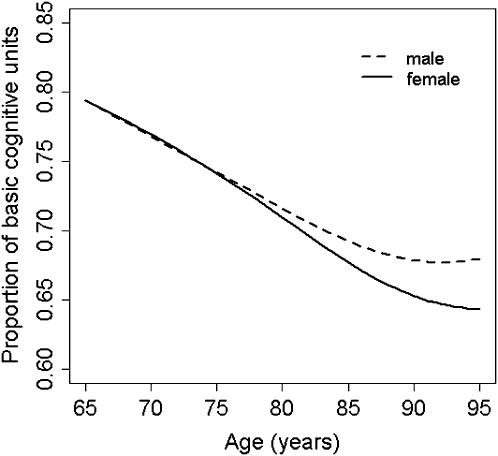
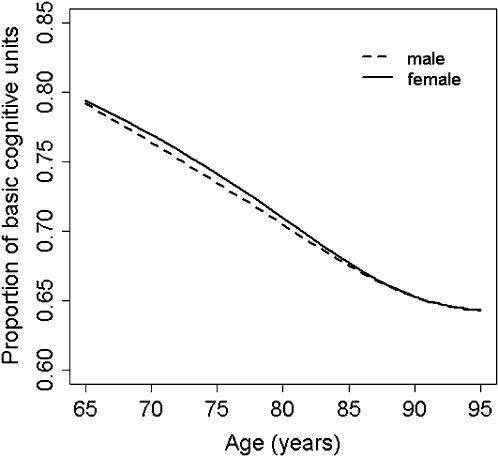
The BCU curves obtained for women and men also showed a similar overall pattern, with a leveling off at advanced age (Fig. 3). However, while the female and male BCU curves run in close proximity up to age 75 years, women deteriorate further at older ages. This difference was statistically significant (for log incidence rates of Alzheimer's disease: sm ancova, P<0.001; generalized additive model using loess, P = 0.0015). Remarkably, the two BCU curves become virtually identical at older ages (Fig. 4) after crude adjustment for gender differences in survival using general population data (generalized additive model for log incidence rates of Alzheimer's disease including age-specific female/male survival ratios as a covariate, P = 0.16) [56], [57].
Figure 3. Non-parametric regression curves of basic cognitive units (BCU) on age, for women and men.
The overall pattern of these two BCU loess curves was similar to that found for the total population (see Fig. 2), with a leveling off at older ages.
However, there were statistically highly significant differences between women and men (generalized additive model for log incidence rates of Alzheimer's disease, P = 0.0015).
While the two curves are very similar up to age 75 years, women deteriorate more than men at older ages.
Figure 4. Adjusted non-parametric regression curves of basic cognitive units (BCU) on age, for women and men.
There were no statistically significant differences in BCU curves between women and men after correcting for gender differences in survival (generalized additive model for log incidence rates of Alzheimer's disease, P = 0.16).
Effect of neuroprotection
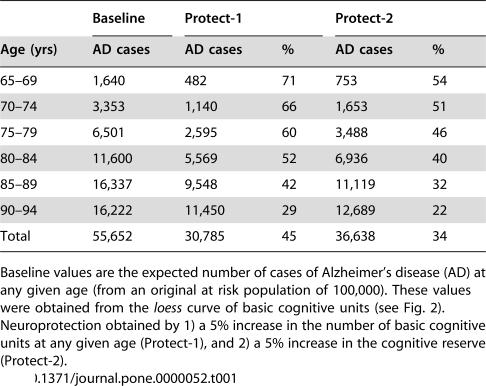
Two different types of neuroprotection were tested: 1) Cell-rescuing therapies (Protect-1), which lead to increased number of BCU at any given age; and 2) Neuroprotective strategies aimed at increasing the cognitive reserve (Protect-2). The model shows that for 5% neuroprotection in age-specific BCU counts (Protect-1), the total number of Alzheimer's cases is expected to decrease by 45% between ages 65 and 94 years (Table 1); for 20% neuroprotection, 96% of Alzheimer's cases would be prevented. On the other hand, a 5% increase in the cognitive reserve (i.e., lowering of the threshold value from 0.5 to 0.475; Protect-2) would save 34% of Alzheimer's cases in the age range 65–94 years (Table 1).
Table 1. Effect of neuroprotection on Alzheimer's disease (AD).
| Baseline | Protect-1 | Protect-2 | |||
| Age (yrs) | AD cases | AD cases | % | AD cases | % |
| 65–69 | 1,640 | 482 | 71 | 753 | 54 |
| 70–74 | 3,353 | 1,140 | 66 | 1,653 | 51 |
| 75–79 | 6,501 | 2,595 | 60 | 3,488 | 46 |
| 80–84 | 11,600 | 5,569 | 52 | 6,936 | 40 |
| 85–89 | 16,337 | 9,548 | 42 | 11,119 | 32 |
| 90–94 | 16,222 | 11,450 | 29 | 12,689 | 22 |
| Total | 55,652 | 30,785 | 45 | 36,638 | 34 |
Baseline values are the expected number of cases of Alzheimer's disease (AD) at any given age (from an original at risk population of 100,000). These values were obtained from the loess curve of basic cognitive units (see Fig. 2). Neuroprotection obtained by 1) a 5% increase in the number of basic cognitive units at any given age (Protect-1), and 2) a 5% increase in the cognitive reserve (Protect-2).
Discussion
This study shows that the incidence rate of Alzheimer's disease increases with age but slows down at older ages. Although not all [42], most previous meta-analyses found a similar deceleration in incidence rates of Alzheimer's disease [41], [43], [44]. The model consistently shows that the number of BCU decreases with age but tends to reach a plateau at advanced age. This observation likely reflects the combination of two different phenomena: 1) The earlier development of dementia in subjects at higher risk (e.g., carriers of the apolipoprotein ε4 allele), which then gives rise to a healthier normal population; and 2) A within-subject constant (or decreasing) risk of neuron death with age, which has experimentally been shown to govern cell kinetics in Alzheimer's disease and other neurodegenerative disorders [58]. It should be emphasized that while different threshold and variance values give different BCU curves, the overall pattern of the curve (i.e., a leveling off at older ages) is mostly independent of these parameter values and consistently suggests a decreasing risk of neuron death at advanced age. In fact, Fig. 3 shows that the average BCU count may indeed increase in older men. This result is in keeping with recent post-mortem results [59], and suggests that men surviving to advanced age might represent a ‘super-normal’ subpopulation [60].
The model also shows gender differences in BCU curves. There is experimental evidence suggesting that estrogens likely have a protective effect on cognitive function [7]. Therefore, it could be argued that estrogen deprivation at advanced age might explain why women have in general higher incidence rates of Alzheimer's disease compared to men [41]–[45]. However, the overall pattern of the BCU curves (i.e., no gender difference up to age 75 years) is difficult to reconcile with this notion. Likewise, constant gender differences in the cognitive reserve (e.g., differences in the level of education) should be associated with differences in BCU curves at any given age, not simply in the older range. The most likely explanation is a survival effect. Indeed, the female and male BCU curves become virtually identical at older ages after correcting for gender differences in survival (Fig. 4). This observation suggests that, in relative terms, socio-economic growth and improvements in public heath care policies and services may tend to favor the survival of relatively frail subjects, particularly at advanced age. Hence, incidence rates of late-onset Alzheimer's disease are likely to increase as the number of subjects surviving to older ages increases in future generations with longer life expectancy. For example, if life expectancy of men increased to match the current life expectancy of women, so too would the male incidence rate of Alzheimer's disease.
Most importantly, the model allows us to predict the impact of preventive neuroprotective strategies on incidence rates of Alzheimer's disease [61]. Cell-rescuing neuroprotective therapies are expected to slow down the rate of neuron loss. As the probability that a neuron can be rescued from Alzheimer-related pathology is not diminished by age [58], the model can be easily accommodated to estimate the effect of cell-rescuing neuroprotection on incidence rates of Alzheimer's disease. It was found that even relatively modest neuroprotective effects on BCU counts can lead to dramatic reductions in incidence rates of Alzheimer's disease. Nonetheless, these results could only be obtained if such ‘hypothetical’ neuroprotective treatment were universally applied to the general population (with the additional problem of treatment-related side effects).
A more realistic neuroprotective strategy, which has important implications for public health decisions on putative preventive methods for Alzheimer's disease, refers to measures aimed at increasing the cognitive reserve. There is a growing body of evidence that higher levels of education and intellectual skills are associated with less cognitive impairment [9]–[14]. Intellectual activity likely improves the efficiency of brain networks and may also increase the level of redundancy in BCU circuits (i.e., more BCU need to be lost to reach the same level of cognitive deterioration) [10]. The model shows that a 5% increase in the cognitive reserve would prevent one third of Alzheimer's cases in the world. This result suggests that health policies aimed at increasing the level of education in the general population, as well as programs implementing cognitive training interventions, are likely the most effective method of preventing Alzheimer's disease. In fact, preliminary results from randomized controlled trials have already shown that cognitive stimulation slows down cognitive decline [62], [63].
Acknowledgments
I thank Michael Schulzer for statistical advice, Anthony F. Jorm and Maria C. Norton for helping in data collection, A. Jon Stoessl for comments on a previous draft of the manuscript, and Donald B. Calne for being a continuous source of inspiration.
Footnotes
Competing Interests: The author has declared that no competing interests exist.
Funding: The author has no support or funding to report.
References
- 1.Rocca WA. Dementia, Parkinson's disease, and stroke in Europe: a commentary. Neurology. 2000;54(Suppl 5):S38–S40. [PubMed] [Google Scholar]
- 2.Ritchie K, Kildea D. Is senile dementia “age-related” or “ageing-related”? – evidence from meta-analysis of dementia prevalence in the oldest old. Lancet. 1995;346:931–934. doi: 10.1016/s0140-6736(95)91556-7. [DOI] [PubMed] [Google Scholar]
- 3.Morris JC. Is Alzheimer's disease inevitable with age? Lessons from clinicopathologic studies of healthy aging and very mild Alzheimer's disease. J Clin Invest. 1999;104:1171–1173. doi: 10.1172/JCI8560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grady CL, Craik FI. Changes in memory processing with age. Curr Opin Neurobiol. 2000;10:224–231. doi: 10.1016/s0959-4388(00)00073-8. [DOI] [PubMed] [Google Scholar]
- 5.Small SA. Age-related memory decline: current concepts and future directions. Arch Neurol. 2001;58:360–364. doi: 10.1001/archneur.58.3.360. [DOI] [PubMed] [Google Scholar]
- 6.Braak H, Braak E. Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol Aging. 1997;18:351–357. doi: 10.1016/s0197-4580(97)00056-0. [DOI] [PubMed] [Google Scholar]
- 7.Morrison JH, Hof PR. Life and death of neurons in the aging brain. Science. 1997;278:412–419. doi: 10.1126/science.278.5337.412. [DOI] [PubMed] [Google Scholar]
- 8.MRC CFAS. Pathological correlates of late-onset dementia in a multicentre, community-based population in England and Wales. Lancet. 2001;357:169–175. doi: 10.1016/s0140-6736(00)03589-3. [DOI] [PubMed] [Google Scholar]
- 9.Bennett DA, Wilson RS, Schneider JA, Evans DA, Mendes de Leon CF, et al. Education modifies the relation of AD pathology to cognitive function in older persons. Neurology. 2003;60:1909–1915. doi: 10.1212/01.wnl.0000069923.64550.9f. [DOI] [PubMed] [Google Scholar]
- 10.Scarmeas N, Stern Y. Cognitive reserve: implications for diagnosis and prevention of Alzheimer's disease. Curr Neurol Neurosci Rep. 2004;4:374–380. doi: 10.1007/s11910-004-0084-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Terry RD, Katzman R. Life span and synapses: will there be a primary senile dementia? Neurobiol Aging. 2001;22:347–348. doi: 10.1016/s0197-4580(00)00250-5. [DOI] [PubMed] [Google Scholar]
- 12.Verghese J, Lipton RB, Katz MJ, Hall CB, Derby CA et al. Leisure activities and the risk of dementia in the elderly. N Engl J Med. 2003;348:2508–2516. doi: 10.1056/NEJMoa022252. [DOI] [PubMed] [Google Scholar]
- 13.Riley KP, Snowdon DA, Desrosiers MF, Markesbery WR. Early life linguistic ability, late life cognitive function, and neuropathology: findings from the Nun Study. Neurobiol Aging. 2005;26:341–347. doi: 10.1016/j.neurobiolaging.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 14.Wang JY, Zhou DHD, Li J, Zhang M, Deng J, et al. Leisure activity and risk of cognitive impairment: the Chongqing aging study. Neurology. 2006;66:911–913. doi: 10.1212/01.wnl.0000192165.99963.2a. [DOI] [PubMed] [Google Scholar]
- 15.Hagnell O, Ojesjo L, Rorsman B. Incidence of dementia in the Lundby Study. Neuroepidemiology. 1992;11(Suppl 1):61–66. doi: 10.1159/000110981. [DOI] [PubMed] [Google Scholar]
- 16.Letenneur L, Commenges D, Dartigues JF, Barberger-Gateau P. Incidence of dementia and Alzheimer's disease in elderly community residents of south-western France. Int J Epidemiol. 1994;23:1256–1261. doi: 10.1093/ije/23.6.1256. [DOI] [PubMed] [Google Scholar]
- 17.Brayne C, Gill C, Huppert FA, Barkley C, Gehlhaar E, et al. Incidence of clinically diagnosed subtypes of dementia in an elderly population. Cambridge Project for Later Life. Br J Psychiatry. 1995;167:255–262. doi: 10.1192/bjp.167.2.255. [DOI] [PubMed] [Google Scholar]
- 18.Aevarsson O, Skoog I. A population-based study on the incidence of dementia disorders between 85 and 88 years of age. J Am Geriatr Soc. 1996;44:1455–1460. doi: 10.1111/j.1532-5415.1996.tb04070.x. [DOI] [PubMed] [Google Scholar]
- 19.Fratiglioni L, Viitanen M, von Strauss E, Tontodonati V, Herlitz A, et al. Very old women at highest risk of dementia and Alzheimer's disease: incidence data from the Kungsholmen Project, Stockholm. Neurology. 1997;48:132–138. doi: 10.1212/wnl.48.1.132. [DOI] [PubMed] [Google Scholar]
- 20.Ott A, Breteler MM, van Harskamp F, Stijnen T, Hofman A. Incidence and risk of dementia. The Rotterdam Study. Am J Epidemiol. 1998;147:574–580. doi: 10.1093/oxfordjournals.aje.a009489. [DOI] [PubMed] [Google Scholar]
- 21.Andersen K, Nielsen H, Lolk A, Andersen J, Becker I, et al. Incidence of very mild to severe dementia and Alzheimer's disease in Denmark: the Odense Study. Neurology. 1999;52:85–90. doi: 10.1212/wnl.52.1.85. [DOI] [PubMed] [Google Scholar]
- 22.Copeland JR, McCracken CFM, Dewey ME, Wilson KC, Doran M, et al. Undifferentiated dementia, Alzheimer's disease and vascular dementia: age- and gender-related incidence in Liverpool. The MRC-ALPHA Study. Br J Psychiatry. 1999;175:433–438. doi: 10.1192/bjp.175.5.433. [DOI] [PubMed] [Google Scholar]
- 23.Di Carlo A, Baldereschi M, Amaducci L, Lepore V, Bracco L, et al. Incidence of dementia, Alzheimer's disease, and vascular dementia in Italy. The ILSA Study. J Am Geriatr Soc. 2002;50:41–48. doi: 10.1046/j.1532-5415.2002.50006.x. [DOI] [PubMed] [Google Scholar]
- 24.Lopez-Pousa S, Vilalta-Franch J, Llinas-Regla J, Garre-Olmo J, Roman GC. Incidence of dementia in a rural community in Spain: the Girona cohort study. Neuroepidemiology. 2004;23:170–177. doi: 10.1159/000078502. [DOI] [PubMed] [Google Scholar]
- 25.Ravaglia G, Forti P, Maioli F, Martelli M, Servadei L, et al. Incidence and etiology of dementia in a large elderly Italian population. Neurology. 2005;64:1525–1530. doi: 10.1212/01.WNL.0000160107.02316.BF. [DOI] [PubMed] [Google Scholar]
- 26.Hebert LE, Scherr PA, Beckett LA, Albert MS, Pilgrim DM, et al. Age-specific incidence of Alzheimer's disease in a community population. JAMA. 1995;273:1354–1359. [PubMed] [Google Scholar]
- 27.Ganguli M, Dodge HH, Chen P, Belle S, DeKosky ST. Ten-year incidence of dementia in a rural elderly US community population: the MoVIES Project. Neurology. 2000;54:1109–1116. doi: 10.1212/wnl.54.5.1109. [DOI] [PubMed] [Google Scholar]
- 29.Tang MX, Cross P, Andrews H, Jacobs DM, Small S, et al. Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology. 2001;56:49–56. doi: 10.1212/wnl.56.1.49. [DOI] [PubMed] [Google Scholar]
- 30.Kukull WA, Higdon R, Bowen JD, McCormick WC, Teri L, et al. Dementia and Alzheimer disease incidence: a prospective cohort study. Arch Neurol. 2002;59:1737–1746. doi: 10.1001/archneur.59.11.1737. [DOI] [PubMed] [Google Scholar]
- 31.Miech RA, Breitner JCS, Zandi PP, Khachaturian AS, Anthony JC, et al. Incidence of AD may decline in the early 90s for men, later for women: The Cache County study. Neurology. 2002;58:209–218. doi: 10.1212/wnl.58.2.209. [DOI] [PubMed] [Google Scholar]
- 32.Evans DA, Bennett DA, Wilson RS, Bienias JL, Morris MC, et al. Incidence of Alzheimer disease in a biracial urban community: relation to apolipoprotein E allele status. Arch Neurol. 2003;60:185–189. doi: 10.1001/archneur.60.2.185. [DOI] [PubMed] [Google Scholar]
- 33.Fitzpatrick AL, Kuller LH, Ives DG, Lopez OL, Jagust W, et al. Incidence and prevalence of dementia in the Cardiovascular Health Study. J Am Geriatr Soc. 2004;52:195–204. doi: 10.1111/j.1532-5415.2004.52058.x. [DOI] [PubMed] [Google Scholar]
- 34.Fukunishi I, Hayabara T, Hosokawa K. Epidemiological surveys of senile dementia in Japan. Int J Soc Psychiatry. 1991;37:51–56. doi: 10.1177/002076409103700107. [DOI] [PubMed] [Google Scholar]
- 35.Yoshitake T, Kiyohara Y, Kato I, Ohmura T, Iwamoto H, et al. Incidence and risk factors of vascular dementia and Alzheimer's disease in a defined elderly Japanese population: the Hisayama Study. Neurology. 1995;45:1161–1168. doi: 10.1212/wnl.45.6.1161. [DOI] [PubMed] [Google Scholar]
- 36.Liu CK, Lai CL, Tai CT, Lin RT, Yen YY, et al. Incidence and subtypes of dementia in southern Taiwan: impact of socio-demographic factors. Neurology. 1998;50:1572–1579. doi: 10.1212/wnl.50.6.1572. [DOI] [PubMed] [Google Scholar]
- 37.Chandra V, Pandav R, Dodge HH, Johnston JM, Belle SH, et al. Incidence of Alzheimer's disease in a rural community in India: the Indo-US study. Neurology. 2001;57:985–989. doi: 10.1212/wnl.57.6.985. [DOI] [PubMed] [Google Scholar]
- 38.Hendrie HC, Ogunniyi A, Hall KS, Baiyewu O, Unverzagt FW, et al. Incidence of dementia and Alzheimer disease in 2 communities: Yoruba residing in Ibadan, Nigeria, and African Americans residing in Indianapolis, Indiana. JAMA. 2001;285:739–747. doi: 10.1001/jama.285.6.739. [DOI] [PubMed] [Google Scholar]
- 39.Waite LM, Broe GA, Grayson DA, Creasey H. The incidence of dementia in an Australian community population: the Sydney Older Persons Study. Int J Geriatr Psychiatry. 2001;16:680–689. doi: 10.1002/gps.404. [DOI] [PubMed] [Google Scholar]
- 40.Nitrini R, Caramelli P, Herrera E, Jr, Bahia VS, Caixeta LF, et al. Incidence of dementia in a community-dwelling Brazilian population. Alzheimer Dis Assoc Disord. 2004;18:241–246. [PubMed] [Google Scholar]
- 41.Gao S, Hendrie HC, Hall KS, Hui S. The relationship between age, sex, and the incidence of dementia and Alzheimer's disease: A meta-analysis. Arch Gen Psychiatry. 1998;55:809–815. doi: 10.1001/archpsyc.55.9.809. [DOI] [PubMed] [Google Scholar]
- 42.Jorm AF, Jolley D. The incidence of dementia: A meta-analysis. Neurology. 1998;51:728–733. doi: 10.1212/wnl.51.3.728. [DOI] [PubMed] [Google Scholar]
- 43.Launer LJ, Andersen K, Dewey ME, Letenneur L, Ott A, et al. Rates and risk factors for dementia and Alzheimer's disease: Results from EURODEM pooled analyses. Neurology. 1999;52:78–84. doi: 10.1212/wnl.52.1.78. [DOI] [PubMed] [Google Scholar]
- 44.Fratiglioni L, Launer LJ, Andersen K, Breteler MM, Copeland JR, et al. Incidence of dementia and major subtypes in Europe: a collaborative study of population-based cohorts. Neurology. 2000;54(Suppl 5):10–15. [PubMed] [Google Scholar]
- 45.Irizarry MC, Hyman BT. Alzheimer's disease. In: Batchelor T, Cudkowicz ME, editors. Principles of neuroepidemiology. Boston: Butterworth-Heinemann; 2001. pp. 69–98. [Google Scholar]
- 46.West MJ, Coleman PD, Flood DG, Troncoso JC. Differences in the pattern of hippocampal neuronal loss in normal ageing and Alzheimer's disease. Lancet. 1994;344:769–772. doi: 10.1016/s0140-6736(94)92338-8. [DOI] [PubMed] [Google Scholar]
- 47.Gomez-Isla T, Price JL, McKeel DW, Jr, Morris JC, Growdon JH, et al. Profound loss of layer II entorhinal cortex neurons occurs in very mild Alzheimer's disease. J Neurosci. 1996;16:4491–4500. doi: 10.1523/JNEUROSCI.16-14-04491.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gomez-Isla T, Hollister R, West H, Mui S, Growdon JH, et al. Neuronal loss correlates with but exceeds neurofibrillary tangles in Alzheimer's disease. Ann Neurol. 1997;41:17–24. doi: 10.1002/ana.410410106. [DOI] [PubMed] [Google Scholar]
- 49.Simic G, Kostovic I, Winblad B, Bogdanovic N. Volume and number of neurons of the human hippocampal formation in normal aging and Alzheimer's disease. J Comp Neurol. 1997;379:482–494. doi: 10.1002/(sici)1096-9861(19970324)379:4<482::aid-cne2>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 50.Price JL, Ko AI, Wade MJ, Tsou SK, McKeel DW, et al. Neuron number in the entorhinal cortex and CA1 in preclinical Alzheimer's disease. Arch Neurol. 2001;58:1395–1402. doi: 10.1001/archneur.58.9.1395. [DOI] [PubMed] [Google Scholar]
- 51.Falke E, Nissanov J, Mitchell TW, Bennett DA, Trojanowski JQ, et al. Subicular dendritic arborization in Alzheimer's disease correlates with neurofibrillary tangle density. Am J Pathol. 2003;163:1615–1621. doi: 10.1016/S0002-9440(10)63518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cleveland WS, Loader C. Smoothing by local regression: principles and methods. In: Haerdle W, Schimek MG, editors. Statistical theory and computational aspects of smoothing. New York: Springer; 1996. pp. 10–49. [Google Scholar]
- 53.Bowman AW, Azzalini A. Applied smoothing techniques for data analysis: the kernel approach with S-Plus illustrations. Oxford, England: Oxford University Press; 1997. [Google Scholar]
- 54.Scrucca L. Nonparametric kernel smoothing methods: the sm library in Xlisp-Stat. J Stat Software. 2001;6:1–49. [Google Scholar]
- 55.Clayton D, Hills M. Statistical models in epidemiology. Oxford, England: Oxford University Press; 1993. [Google Scholar]
- 56.Arias E. United States Life Tables, 2001. National Vital Statistical Reports. 2004;52((14)):1–40. Available: http://www.cdc.gov/nchs/data/nvsr/nvsr52/nvsr52_14.pdf. [PubMed] [Google Scholar]
- 57.U.S. Census BureauInternational Data BaseIDB Population Pyramids. Available: http://www.census.gov/ipc/www/idbpyr.html. Accessed 2006, May 8. [Google Scholar]
- 58.Clarke G, Collins RA, Leavitt BR, Andrews DF, Hayden MR, et al. A one-hit model of cell death in inherited neuronal degenerations. Nature. 2000;406:195–199. doi: 10.1038/35018098. [DOI] [PubMed] [Google Scholar]
- 59.Kubis N, Faucheux BA, Ransmayr G, Damier P, Duyckaerts C, et al. Preservation of midbrain catecholaminergic neurons in very old human subjects. Brain. 2000;123:366–373. doi: 10.1093/brain/123.2.366. [DOI] [PubMed] [Google Scholar]
- 60.Calne DB, Eisen A, Meneilly G. Normal aging of the nervous system. Ann Neurol. 1991;30:206–207. doi: 10.1002/ana.410300213. [DOI] [PubMed] [Google Scholar]
- 61.Shoulson I. Experimental therapeutics of neurodegenerative disorders: unmet needs. Science. 1998;282:1072–1074. doi: 10.1126/science.282.5391.1072. [DOI] [PubMed] [Google Scholar]
- 62.Ball K, Berch DB, Helmers KF, Jobe JB, Leveck MD, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA. 2002;288:2271–2281. doi: 10.1001/jama.288.18.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Spector A, Thorgrimsen L, Woods B, Royan L, Davies S, et al. Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial. Br J Psychiatry. 2003;183:248–254. doi: 10.1192/bjp.183.3.248. [DOI] [PubMed] [Google Scholar]