Abstract
Background: There are few data on the optimal micronutrient composition of paediatric enteral feeds. The recent European Directive on Foods for Special Medical Purposes (1999/21/EC) did not distinguish between the composition of adult and paediatric feeds.
Aims: To evaluate, in an open, observational study, the long term nutritional biochemistry of 12 children aged 1–6 years and/or 8–20 kg.
Methods: The children were receiving at least 50% of their estimated average requirement (EAR) for energy from paediatric enteral formulae: 1.0 kcal/ml (Nutrison Paediatric Standard) or 1.5 kcal/ml (Nutrison Paediatric Energy Plus). Venous blood samples for trace elements, vitamins, and minerals were taken at study entry and six months later. Parents kept three day food and feed records every month.
Results: Despite a median energy intake of only 75% EAR (range 52–158%), 67% (n = 8) achieved their reference nutrient intake (RNI) for all micronutrients. No significant micronutrient deficiencies were seen on blood analysis after six months. Eighty three per cent (n = 10) had vitamin B12 and 92% (n = 11) had copper intake >150% RNI. Fifty eight per cent (n = 7) had high plasma B12 (>733 µmol/l) and 75% (n = 9) had high serum copper (>22 µmol/l) concentrations.
Conclusions: Children without excess losses maintain adequate micronutrient status on long term enteral feeding. Subjects had high blood concentrations of vitamin B12 and copper, and had high dietary intakes of these micronutrients. We suggest that the maximum nutrient guidelines for paediatric enteral feeds should be more clearly defined.
Full Text
The Full Text of this article is available as a PDF (91.1 KB).
Figure 1 .
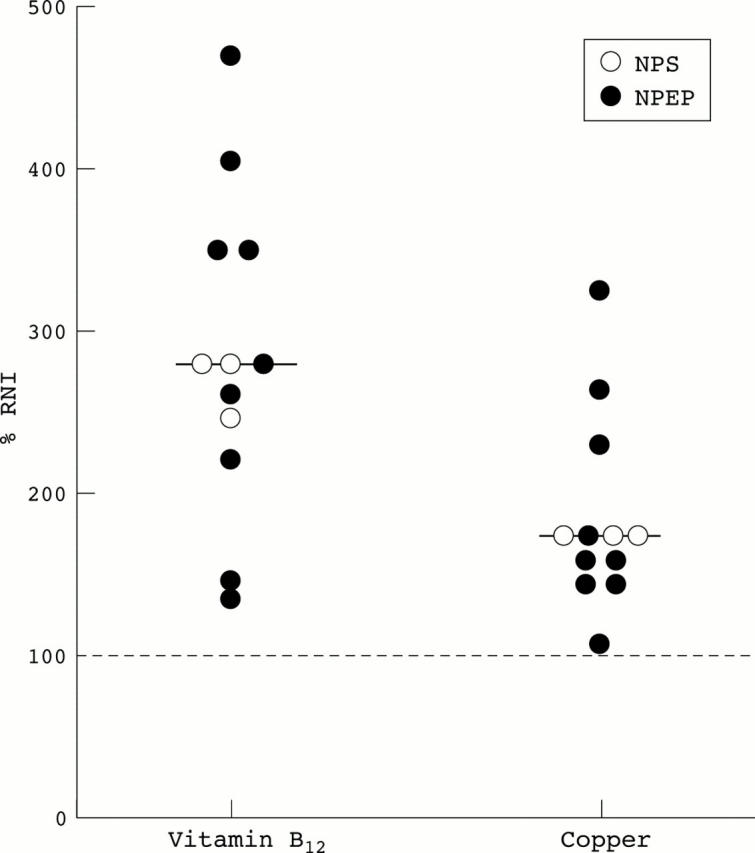
Vitamin B12 and copper intake as a percentage of RNI.2
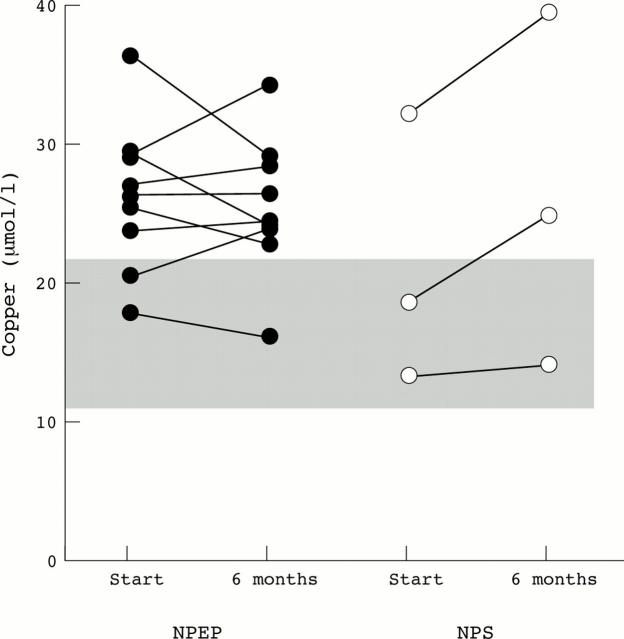
Figure 2 .
Serum copper concentrations.
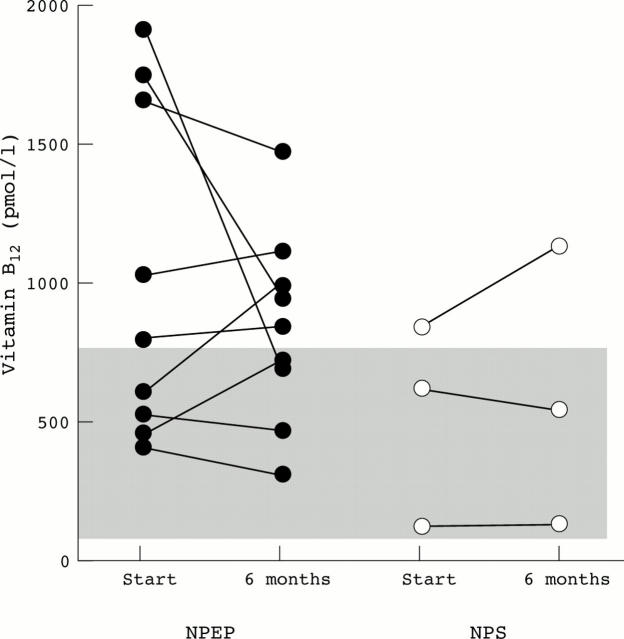
Figure 3 .
Plasma vitamin B12 concentrations.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aggett P. J., Bresson J., Haschke F., Hernell O., Koletzko B., Lafeber H. N., Michaelsen K. F., Micheli J., Ormisson A., Rey J. Recommended Dietary Allowances (RDAs), Recommended Dietary Intakes (RDIs), Recommended Nutrient Intakes (RNIs), and Population Reference Intakes (PRIs) are not "recommended intakes". J Pediatr Gastroenterol Nutr. 1997 Aug;25(2):236–241. doi: 10.1097/00005176-199708000-00022. [DOI] [PubMed] [Google Scholar]
- Suresh-Babu M. V., Thomas A. G. Nutrition in children with cerebral palsy. J Pediatr Gastroenterol Nutr. 1998 Apr;26(4):484–485. doi: 10.1097/00005176-199804000-00026. [DOI] [PubMed] [Google Scholar]
- Van Geet C., Van Damme-Lombaerts R., Vanrusselt M., de Mol A., Proesmans W., Vermylen J. Recombinant human erythropoietin increases blood pressure, platelet aggregability and platelet free calcium mobilisation in uraemic children: a possible link? Thromb Haemost. 1990 Aug 13;64(1):7–10. [PubMed] [Google Scholar]