Abstract
Background: Polyarteritis nodosa is a necrotising vasculitis of the medium sized and small muscular arteries. The inflammatory and subsequent reparative processes may alter the arterial mechanical properties. The effect of vasculitic damage on arterial distensibility has never been explored however.
Aim: To determine the normal values and the effect of childhood vasculitis on arterial distensibility in children and teenagers.
Methods: Distensibility of the brachioradial arterial segment was studied using pulse wave velocity (PWV ∝1/√distensibility), in 13 children with polyarteritis nodosa at a median age of 11.8 (range 4.9–16) years. As a control group, 155 healthy schoolchildren (6–18 years, 81 boys) were studied. PWV was assessed using a photoplethysmographic technique; blood pressure was measured by an automatic sphygmomanometer (Dinamap). Data from patients were expressed as z scores adjusted for age and compared to a population mean of 0 by a single sample t test. Determinants of PWV in normal children were assessed by univariate and multivariate linear regression analyses.
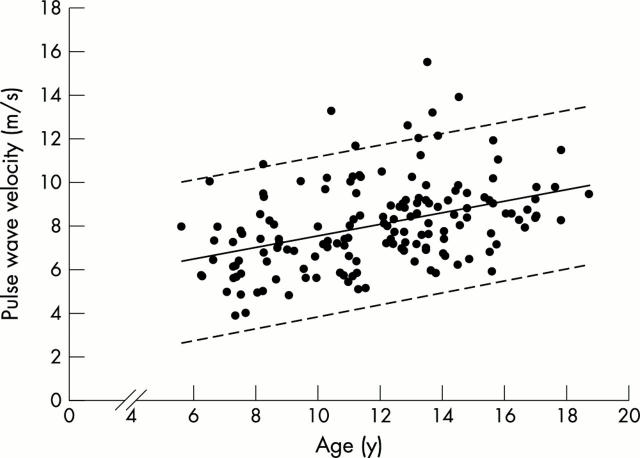
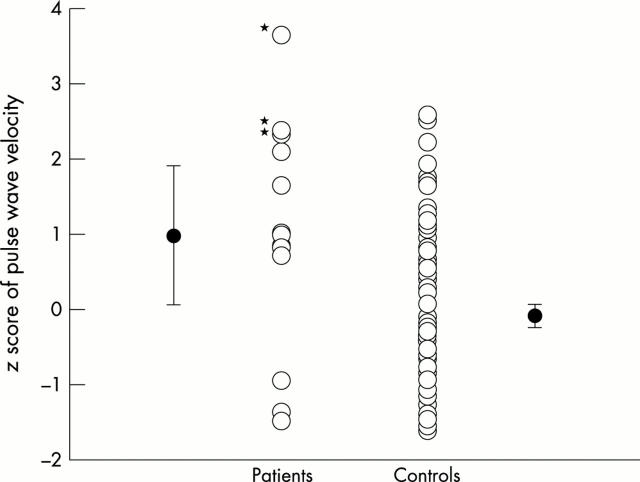
Results: Age, height, weight, and systolic blood pressure correlated individually with the brachioradial PWV. Multivariate analysis identified age as the only independent determinant. Ten of the patients were in clinical remission, while three had evidence of disease activity at the time of study. The PWV in the patient group as a whole was significantly greater than those in healthy children (mean z score +0.99). Raised C reactive protein concentration (>2 mg/dl) in the three patients with active disease was associated with a higher PWV when compared to those in remission (z score +2.78 v +0.45). The diastolic blood pressure of the patients was higher than those of the controls (z score +1.04) while the systolic pressure was similar (z score -0.36).
Conclusions: PWV in the brachioradial arterial segment increases gradually during childhood independent of body weight, height, mass, and blood pressure. Increased PWV, and hence decreased distensibility, in this peripheral arterial segment occurs in polyarteritis nodosa and is amplified during acute inflammatory exacerbation.
Full Text
The Full Text of this article is available as a PDF (126.4 KB).
Figure 1 .
Scatter plot of pulse wave velocity against age. The lines represent the mean (solid line) and the 95% prediction interval (dashed lines).
Figure 2 .
Vertical scatter plots of z scores of pulse wave velocity in patients and controls. The error bar represents mean (SEM); z scores of the three patients with flare of disease activity at the time of study are marked by asterisks.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Asar R, Scuteri A, Topouchian J, Brisac AM, Maldonado J, Cloarec L, Safar M. Arterial distensibility and circadian blood pressure variability. Blood Press Monit. 1996 Aug;1(4):333–338. [PubMed] [Google Scholar]
- Asmar R. G., Brunel P. C., Pannier B. M., Lacolley P. J., Safar M. E. Arterial distensibility and ambulatory blood pressure monitoring in essential hypertension. Am J Cardiol. 1988 May 1;61(13):1066–1070. doi: 10.1016/0002-9149(88)90127-0. [DOI] [PubMed] [Google Scholar]
- Avolio A. P., Chen S. G., Wang R. P., Zhang C. L., Li M. F., O'Rourke M. F. Effects of aging on changing arterial compliance and left ventricular load in a northern Chinese urban community. Circulation. 1983 Jul;68(1):50–58. doi: 10.1161/01.cir.68.1.50. [DOI] [PubMed] [Google Scholar]
- Avolio A. P., Deng F. Q., Li W. Q., Luo Y. F., Huang Z. D., Xing L. F., O'Rourke M. F. Effects of aging on arterial distensibility in populations with high and low prevalence of hypertension: comparison between urban and rural communities in China. Circulation. 1985 Feb;71(2):202–210. doi: 10.1161/01.cir.71.2.202. [DOI] [PubMed] [Google Scholar]
- Bendeck M. P., Langille B. L. Rapid accumulation of elastin and collagen in the aortas of sheep in the immediate perinatal period. Circ Res. 1991 Oct;69(4):1165–1169. doi: 10.1161/01.res.69.4.1165. [DOI] [PubMed] [Google Scholar]
- Blacher J., Asmar R., Djane S., London G. M., Safar M. E. Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension. 1999 May;33(5):1111–1117. doi: 10.1161/01.hyp.33.5.1111. [DOI] [PubMed] [Google Scholar]
- Blacher J., Guerin A. P., Pannier B., Marchais S. J., Safar M. E., London G. M. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999 May 11;99(18):2434–2439. doi: 10.1161/01.cir.99.18.2434. [DOI] [PubMed] [Google Scholar]
- Bloch D. A., Michel B. A., Hunder G. G., McShane D. J., Arend W. P., Calabrese L. H., Edworthy S. M., Fauci A. S., Fries J. F., Leavitt R. Y. The American College of Rheumatology 1990 criteria for the classification of vasculitis. Patients and methods. Arthritis Rheum. 1990 Aug;33(8):1068–1073. doi: 10.1002/art.1780330803. [DOI] [PubMed] [Google Scholar]
- Cheung Y. F., Taylor M. J., Fisk N. M., Redington A. N., Gardiner H. M. Fetal origins of reduced arterial distensibility in the donor twin in twin-twin transfusion syndrome. Lancet. 2000 Apr 1;355(9210):1157–1158. doi: 10.1016/s0140-6736(00)02068-7. [DOI] [PubMed] [Google Scholar]
- Gardner M. J., Altman D. G. Confidence intervals rather than P values: estimation rather than hypothesis testing. Br Med J (Clin Res Ed) 1986 Mar 15;292(6522):746–750. doi: 10.1136/bmj.292.6522.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gribbin B., Pickering T. G., Sleight P. Arterial distensibility in normal and hypertensive man. Clin Sci (Lond) 1979 May;56(5):413–417. doi: 10.1042/cs0560413. [DOI] [PubMed] [Google Scholar]
- Haverkate F., Thompson S. G., Pyke S. D., Gallimore J. R., Pepys M. B. Production of C-reactive protein and risk of coronary events in stable and unstable angina. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Lancet. 1997 Feb 15;349(9050):462–466. doi: 10.1016/s0140-6736(96)07591-5. [DOI] [PubMed] [Google Scholar]
- Laogun A. A., Gosling R. G. In vivo arterial compliance in man. Clin Phys Physiol Meas. 1982 Aug;3(3):201–212. doi: 10.1088/0143-0815/3/3/004. [DOI] [PubMed] [Google Scholar]
- Martyn C. N., Greenwald S. E. Impaired synthesis of elastin in walls of aorta and large conduit arteries during early development as an initiating event in pathogenesis of systemic hypertension. Lancet. 1997 Sep 27;350(9082):953–955. doi: 10.1016/s0140-6736(96)10508-0. [DOI] [PubMed] [Google Scholar]
- ROACH M. R., BURTON A. C. The reason for the shape of the distensibility curves of arteries. Can J Biochem Physiol. 1957 Aug;35(8):681–690. [PubMed] [Google Scholar]
- Smulyan H., Csermely T. J., Mookherjee S., Warner R. A. Effect of age on arterial distensibility in Asymptomatic humans. Arteriosclerosis. 1983 May-Jun;3(3):199–205. doi: 10.1161/01.atv.3.3.199. [DOI] [PubMed] [Google Scholar]
- Zhang Y. X., Cliff W. J., Schoefl G. I., Higgins G. Coronary C-reactive protein distribution: its relation to development of atherosclerosis. Atherosclerosis. 1999 Aug;145(2):375–379. doi: 10.1016/s0021-9150(99)00105-7. [DOI] [PubMed] [Google Scholar]