Abstract
Aims: To delineate the pattern of growth in prepubertal children with congenital disorder of glycosylation type Ia (CDG-Ia) in order to identify critical period(s) and possible cause(s) of growth failure.
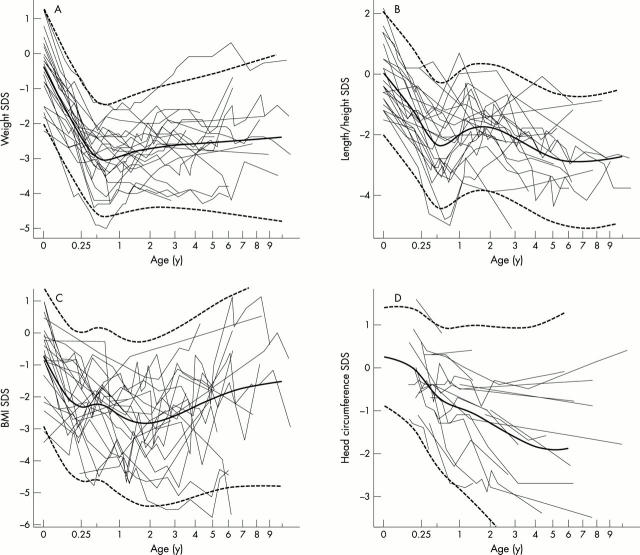
Methods: Longitudinal measurements of weight, length/height, and head circumference from birth to 10 years of age in 25 CDG-Ia patients with the R141H/F119L PMM2 genotype were analysed. The data and derived body mass indices (BMI) were compared with standards and expressed as standard deviation scores (SDS). A linear mixed effects model was fitted to each set of data, and mean curves were estimated.
Results: The mean weight SDS decreased from -0.3 at birth to -3.0 at 7 months of age and remained low or increased slightly. The mean length SDS decreased from zero at birth to -2.4 at 7 months of age followed by a slight increase to a maximum of -1.8 SDS at the end of the second year of life. After age 2 the mean length/height SDS decreased again. The mean BMI SDS at birth was -0.7 and declined to a minimum of -2.8 at the end of the second year of life followed by a gradual increase. The mean head circumference SDS declined gradually from 0 at 3 months of age to -1.9 at age 5.
Conclusion: CDG-Ia patients with the R141H/F119L genotype have normal fetal growth and an immediate postnatal onset of severe growth failure. A notable decline in weight end length SDS takes place during the first seven months of life with no prepubertal catch up.
Full Text
The Full Text of this article is available as a PDF (122.9 KB).
Figure 1 .
Weight (A), length/height (B), BMI (C), and head circumference (D) SDS versus age (square root transformed age scale). Individual curves are shown as thin lines. The estimated mean curve is shown as a solid line, and the boundaries of the tolerance interval (95%) are shown as dashed lines.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andersen E., Hutchings B., Jansen J., Nyholm M. Højde og vaegt hos danske børn. Ugeskr Laeger. 1982 Jun 14;144(24):1760–1765. [PubMed] [Google Scholar]
- Clayton P., Winchester B., Di Tomaso E., Young E., Keir G., Rodeck C. Carbohydrate-deficient glycoprotein syndrome: normal glycosylation in the fetus. Lancet. 1993 Apr 10;341(8850):956–956. doi: 10.1016/0140-6736(93)91244-g. [DOI] [PubMed] [Google Scholar]
- Jaeken J., Stibler H., Hagberg B. The carbohydrate-deficient glycoprotein syndrome. A new inherited multisystemic disease with severe nervous system involvement. Acta Paediatr Scand Suppl. 1991;375:1–71. [PubMed] [Google Scholar]
- Jansen J. Måling af hovedomfang ved helbredsundersøgelser af børn. En multicenterundersøgelse. Ugeskr Laeger. 1982 Nov 8;144(45):3337–3342. [PubMed] [Google Scholar]
- Kjaergaard S., Schwartz M., Skovby F. Congenital disorder of glycosylation type Ia (CDG-Ia): phenotypic spectrum of the R141H/F119L genotype. Arch Dis Child. 2001 Sep;85(3):236–239. doi: 10.1136/adc.85.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjaergaard S., Skovby F., Schwartz M. Absence of homozygosity for predominant mutations in PMM2 in Danish patients with carbohydrate-deficient glycoprotein syndrome type 1. Eur J Hum Genet. 1998 Jul-Aug;6(4):331–336. doi: 10.1038/sj.ejhg.5200194. [DOI] [PubMed] [Google Scholar]
- Kristiansson B., Borulf S., Conradi N., Erlanson-Albertsson C., Ryd W., Stibler H. Intestinal, pancreatic and hepatic involvement in carbohydrate-deficient glycoprotein syndrome type I. J Pediatr Gastroenterol Nutr. 1998 Jul;27(1):23–29. doi: 10.1097/00005176-199807000-00005. [DOI] [PubMed] [Google Scholar]
- Macchia P. E., Harrison H. H., Scherberg N. H., Sunthornthepfvarakul T., Jaeken J., Refetoff S. Thyroid function tests and characterization of thyroxine-binding globulin in the carbohydrate-deficient glycoprotein syndrome type I. J Clin Endocrinol Metab. 1995 Dec;80(12):3744–3749. doi: 10.1210/jcem.80.12.8530628. [DOI] [PubMed] [Google Scholar]
- Matthijs G., Schollen E., Bjursell C., Erlandson A., Freeze H., Imtiaz F., Kjaergaard S., Martinsson T., Schwartz M., Seta N. Mutations in PMM2 that cause congenital disorders of glycosylation, type Ia (CDG-Ia). Hum Mutat. 2000 Nov;16(5):386–394. doi: 10.1002/1098-1004(200011)16:5<386::AID-HUMU2>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- Matthijs G., Schollen E., Pardon E., Veiga-Da-Cunha M., Jaeken J., Cassiman J. J., Van Schaftingen E. Mutations in PMM2, a phosphomannomutase gene on chromosome 16p13, in carbohydrate-deficient glycoprotein type I syndrome (Jaeken syndrome). Nat Genet. 1997 May;16(1):88–92. doi: 10.1038/ng0597-88. [DOI] [PubMed] [Google Scholar]
- Nysom K., Mølgaard C., Hutchings B., Michaelsen K. F. Body mass index of 0 to 45-y-old Danes: reference values and comparison with published European reference values. Int J Obes Relat Metab Disord. 2001 Feb;25(2):177–184. doi: 10.1038/sj.ijo.0801515. [DOI] [PubMed] [Google Scholar]
- Petersen M. B., Brostrøm K., Stibler H., Skovby F. Early manifestations of the carbohydrate-deficient glycoprotein syndrome. J Pediatr. 1993 Jan;122(1):66–70. doi: 10.1016/s0022-3476(05)83488-2. [DOI] [PubMed] [Google Scholar]
- Stibler H., Skovby F. Failure to diagnose carbohydrate-deficient glycoprotein syndrome prenatally. Pediatr Neurol. 1994 Jul;11(1):71–71. doi: 10.1016/0887-8994(94)90097-3. [DOI] [PubMed] [Google Scholar]
- Van Schaftingen E., Jaeken J. Phosphomannomutase deficiency is a cause of carbohydrate-deficient glycoprotein syndrome type I. FEBS Lett. 1995 Dec 27;377(3):318–320. doi: 10.1016/0014-5793(95)01357-1. [DOI] [PubMed] [Google Scholar]
- de Zegher F., Jaeken J. Endocrinology of the carbohydrate-deficient glycoprotein syndrome type 1 from birth through adolescence. Pediatr Res. 1995 Apr;37(4 Pt 1):395–401. doi: 10.1203/00006450-199504000-00003. [DOI] [PubMed] [Google Scholar]