Abstract
Aims: To determine the prevalence, clinical characteristics, and outcome of hypoglycaemia on admission in children at a rural Kenyan district hospital.
Methods: Observational study of 3742 children (including 280 neonates) in Kilifi District Hospital, Kenya. Main outcome measures: hypoglycaemia (blood glucose <2.2 mmol/l) and hyperglycaemia (blood glucose >10.0 mmol/l).
Results: Non-neonates: the prevalence of hypoglycaemia on admission was 7.3%. Severe illness, malnutrition, last meal >12 hours ago, and a positive malaria slide were independently associated with hypoglycaemia. Overall, mortality in hypoglycaemic children was 20.2% compared to 3.8% in normoglycaemic children (p < 0.001). The brunt of mortality in hypoglycaemic children was borne by those who were severely ill or malnourished (31.8%) as opposed to those who were neither severely ill nor malnourished (9.0%). Neonates: 23.0% of neonates were hypoglycaemic on admission. Inability to breast feed and weight <2500 g were independently associated with hypoglycaemia. Mortality was 45.2% compared to 19.6% in normoglycaemic neonates (p < 0.001). Hyperglycaemia was present in 2.7% of children and was associated with a higher mortality than normoglycaemia, 14.0% versus 3.8% respectively (p < 0.001).
Conclusions: Hypoglycaemia is common in children admitted to a rural Kenyan district hospital and is associated with an increased mortality. Apart from features of severe illness and poor feeding, clinical signs have a low sensitivity and specificity for hypoglycaemia. Where diagnostic facilities are lacking, presumptive treatment of severely ill children is recommended. For other children, the continuation of feeding (by nasogastric tube if necessary) should be part of standard management.
Full Text
The Full Text of this article is available as a PDF (134.4 KB).
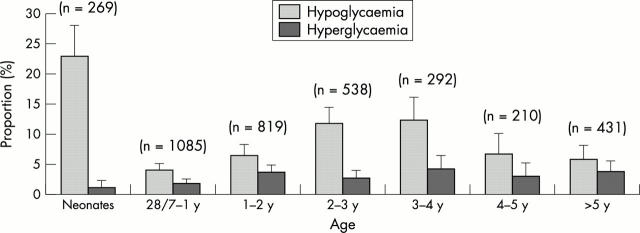
Figure 1.
Prevalence of hypoglycaemia and hyperglycaemia with age.
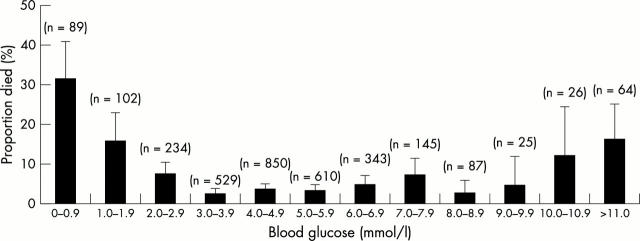
Figure 2.
Association between blood glucose and mortality.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aynsley-Green A. Glucose, the brain and the paediatric endocrinologist. Horm Res. 1996 Jul;46(1):8–25. doi: 10.1159/000184971. [DOI] [PubMed] [Google Scholar]
- Bennish M. L., Azad A. K., Rahman O., Phillips R. E. Hypoglycemia during diarrhea in childhood. Prevalence, pathophysiology, and outcome. N Engl J Med. 1990 May 10;322(19):1357–1363. doi: 10.1056/NEJM199005103221905. [DOI] [PubMed] [Google Scholar]
- Bhisitkul D. M., Morrow A. L., Vinik A. I., Shults J., Layland J. C., Rohn R. Prevalence of stress hyperglycemia among patients attending a pediatric emergency department. J Pediatr. 1994 Apr;124(4):547–551. doi: 10.1016/s0022-3476(05)83132-4. [DOI] [PubMed] [Google Scholar]
- Bondi F. S. Childhood coma in Ibadan. Relationship to socio-economic factors. Trop Geogr Med. 1991 Jul;43(3):288–292. [PubMed] [Google Scholar]
- English M., Sauerwein R., Waruiru C., Mosobo M., Obiero J., Lowe B., Marsh K. Acidosis in severe childhood malaria. QJM. 1997 Apr;90(4):263–270. doi: 10.1093/qjmed/90.4.263. [DOI] [PubMed] [Google Scholar]
- Kawo N. G., Msengi A. E., Swai A. B., Chuwa L. M., Alberti K. G., McLarty D. G. Specificity of hypoglycaemia for cerebral malaria in children. Lancet. 1990 Aug 25;336(8713):454–457. doi: 10.1016/0140-6736(90)92009-7. [DOI] [PubMed] [Google Scholar]
- Marsh K., Forster D., Waruiru C., Mwangi I., Winstanley M., Marsh V., Newton C., Winstanley P., Warn P., Peshu N. Indicators of life-threatening malaria in African children. N Engl J Med. 1995 May 25;332(21):1399–1404. doi: 10.1056/NEJM199505253322102. [DOI] [PubMed] [Google Scholar]
- Newton C. R., Warn P. A., Winstanley P. A., Peshu N., Snow R. W., Pasvol G., Marsh K. Severe anaemia in children living in a malaria endemic area of Kenya. Trop Med Int Health. 1997 Feb;2(2):165–178. doi: 10.1046/j.1365-3156.1997.d01-238.x. [DOI] [PubMed] [Google Scholar]
- Ronan A., Azad A. K., Rahman O., Phillips R. E., Bennish M. L. Hyperglycemia during childhood diarrhea. J Pediatr. 1997 Jan;130(1):45–51. doi: 10.1016/s0022-3476(97)70309-3. [DOI] [PubMed] [Google Scholar]
- Shehadeh N., On A., Kessel I., Perlman R., Even L., Naveh T., Soloveichik L., Etzioni A. Stress hyperglycemia and the risk for the development of type 1 diabetes. J Pediatr Endocrinol Metab. 1997 May-Jun;10(3):283–286. doi: 10.1515/jpem.1997.10.3.283. [DOI] [PubMed] [Google Scholar]
- Solomon T., Felix J. M., Samuel M., Dengo G. A., Saldanha R. A., Schapira A., Phillips R. E. Hypoglycaemia in paediatric admissions in Mozambique. Lancet. 1994 Jan 15;343(8890):149–150. doi: 10.1016/s0140-6736(94)90937-7. [DOI] [PubMed] [Google Scholar]
- Villalpando Hernández S., Hernández Zamora A., Vázquez O., Junco Lorenzana E. Hiperglicemia del lactante deshidratado. Bol Med Hosp Infant Mex. 1980 Mar-Apr;37(2):185–193. [PubMed] [Google Scholar]
- Watson A. R., Coovadia H. M., Bhoola K. D. The clinical syndrome of Impila (Callilepis laureola) poisoning in children. S Afr Med J. 1979 Feb 24;55(8):290–292. [PubMed] [Google Scholar]
- Wharton B. Protein energy malnutrition: problems and priorities. Acta Paediatr Scand Suppl. 1991;374:5–14. doi: 10.1111/j.1651-2227.1991.tb12001.x. [DOI] [PubMed] [Google Scholar]
- White N. J., Miller K. D., Marsh K., Berry C. D., Turner R. C., Williamson D. H., Brown J. Hypoglycaemia in African children with severe malaria. Lancet. 1987 Mar 28;1(8535):708–711. doi: 10.1016/s0140-6736(87)90354-0. [DOI] [PubMed] [Google Scholar]
- Yang S. Y., Zhang S., Wang M. L. Clinical significance of admission hyperglycemia and factors related to it in patients with acute severe head injury. Surg Neurol. 1995 Oct;44(4):373–377. doi: 10.1016/0090-3019(96)80243-6. [DOI] [PubMed] [Google Scholar]