Abstract
Objective: To determine the levels of sound to which infants are exposed during routine transport by ambulance, aircraft, and helicopter.
Design: Sound levels during 38 consecutive journeys from a regional level III neonatal intensive care unit were recorded using a calibrated data logging sound meter (Quest 2900). The meter was set to record "A" weighted slow response integrated sound levels, which emulates the response of the human ear, and "C" weighted response sound levels as a measure of total sound level exposure for all frequencies. The information was downloaded to a computer using MS HyperTerminal. The resulting data were stored, and a graphical profile was generated for each journey using SigmaPlot software.
Setting: Eight journeys involved ambulance transport on country roads, 24 involved fixed wing aircraft, and four were by helicopter.
Main outcome measures: Relations between decibel levels and events or changes in transport mode were established by correlating the time logged on the sound meter with the standard transport documentation sheet.
Results: The highest sound levels were recorded during air transport. However, mean sound levels for all modes of transport exceeded the recommended levels for neonatal intensive care. The maximum sound levels recorded were extremely high at greater than 80 dB in the "A" weighted hearing range and greater than 120 dB in the total frequency range.
Conclusions: This study raises major concerns about the excessive exposure of the sick newborn to sound during transportation.
Full Text
The Full Text of this article is available as a PDF (186.8 KB).
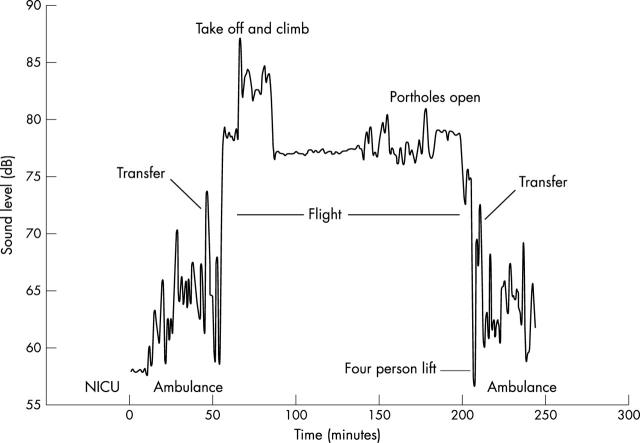
Figure 1 .
Transport of a non-ventilated infant to a specialised cardiac unit in Auckland, New Zealand from Christchurch Womens Hospital, lasting 240 minutes. Note the increased noise exposure during take off and when the portholes of the incubator were opened, and the variation in ambulance noise levels due to acceleration, speed, and road surface. Also note that all recordings are above the recommended level of 60 dB. NICU, Neonatal intensive care unit.
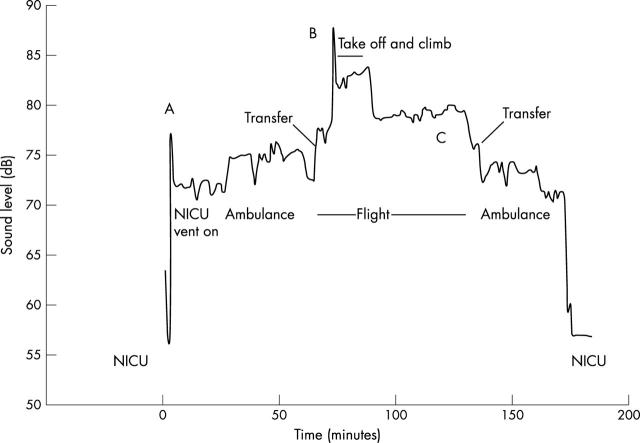
Figure 2 .
Transport of ventilated infant by ambulance and air over 180 minutes. Note: (A) the impact of the internal air compressor used to drive the ventilator, which raises sound levels above 70 dB before the start of transport; (B) the highest sound level recorded was on aircraft take off; (C) the high (close to 80 dB) continuous level of exposure for more than an hour. NICU, Neonatal intensive care unit.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Borradori C., Fawer C. L., Buclin T., Calame A. Risk factors of sensorineural hearing loss in preterm infants. Biol Neonate. 1997;71(1):1–10. doi: 10.1159/000244391. [DOI] [PubMed] [Google Scholar]
- Ciesielski S., Kopka J., Kidawa B. Incubator noise and vibration--possible iatrogenic influence on neonate. Int J Pediatr Otorhinolaryngol. 1980 Feb;1(4):309–316. doi: 10.1016/0165-5876(80)90005-1. [DOI] [PubMed] [Google Scholar]
- Gajendragadkar G., Boyd J. A., Potter D. W., Mellen B. G., Hahn G. D., Shenai J. P. Mechanical vibration in neonatal transport: a randomized study of different mattresses. J Perinatol. 2000 Jul-Aug;20(5):307–310. doi: 10.1038/sj.jp.7200349. [DOI] [PubMed] [Google Scholar]
- Long J. G., Lucey J. F., Philip A. G. Noise and hypoxemia in the intensive care nursery. Pediatrics. 1980 Jan;65(1):143–145. [PubMed] [Google Scholar]
- Macnab A., Chen Y., Gagnon F., Bora B., Laszlo C. Vibration and noise in pediatric emergency transport vehicles: a potential cause of morbidity? Aviat Space Environ Med. 1995 Mar;66(3):212–219. [PubMed] [Google Scholar]
- Magnavita V., Arslan E., Benini F. Esposizione a rumore nelle terapie neonatali intensive. Acta Otorhinolaryngol Ital. 1994 Sep-Oct;14(5):489–501. [PubMed] [Google Scholar]
- Miller C. The physiologic effects of air transport on the neonate. Neonatal Netw. 1994 Oct;13(7):7–10. [PubMed] [Google Scholar]
- Noise: a hazard for the fetus and newborn. American Academy of Pediatrics. Committee on Environmental Health. Pediatrics. 1997 Oct;100(4):724–727. [PubMed] [Google Scholar]
- Philbin M. K. Some implications of early auditory development for the environment of hospitalized preterm infants. Neonatal Netw. 1996 Dec;15(8):71–73. [PubMed] [Google Scholar]
- Philbin M. K. The influence of auditory experience on the behavior of preterm newborns. J Perinatol. 2000 Dec;20(8 Pt 2):S77–S87. doi: 10.1038/sj.jp.7200453. [DOI] [PubMed] [Google Scholar]
- Todd N. W. At-risk populations for hearing impairment in infants and young children. Int J Pediatr Otorhinolaryngol. 1994 Mar;29(1):11–21. doi: 10.1016/0165-5876(94)90104-x. [DOI] [PubMed] [Google Scholar]
- Zahr L. K., de Traversay J. Premature infant responses to noise reduction by earmuffs: effects on behavioral and physiologic measures. J Perinatol. 1995 Nov-Dec;15(6):448–455. [PubMed] [Google Scholar]