Abstract
Aim—To determine the frequency of skip lesions in an unselected series of temporal artery biopsies and compare the results with other series.
Methods—The study was a retrospective review of 102 consecutive temporal artery biopsies taken in a five year period (1992–1997) in one large hospital.
Results—35 cases (34.3%) showed evidence of active cranial vasculitis with pathological evidence of inflammation of the intima or media, with or without giant cells. Three of these cases (8.5%) showed apparent skip lesions: normal intima, media, and adventitia in one segment while in other segments there was clear evidence of active vasculitis. Immunocytochemical stains for leucocyte common antigen (LCA) and CD15 were helpful in identifying the absence of intimal or medial inflammatory cell infiltrates within skip lesions. Skip lesions have been described in up to 28.3% of cases in some series, while others have not found evidence of skip lesions or have identified them in a much smaller percentage of cases.
Conclusions—In this series skip lesions were relatively rare, accounting for 8.5% of cases of active vasculitis. The degree of inflammation in temporal arteritis is discontinuous. Immunostaining for inflammatory cells, for example LCA and CD15, may be helpful in identifying the presence of an inflammatory cell infiltrate in skip lesion segments of the temporal artery.
Key Words: temporal arteritis • inflammation • skip lesion • immunohistochemistry
Full Text
The Full Text of this article is available as a PDF (133.7 KB).
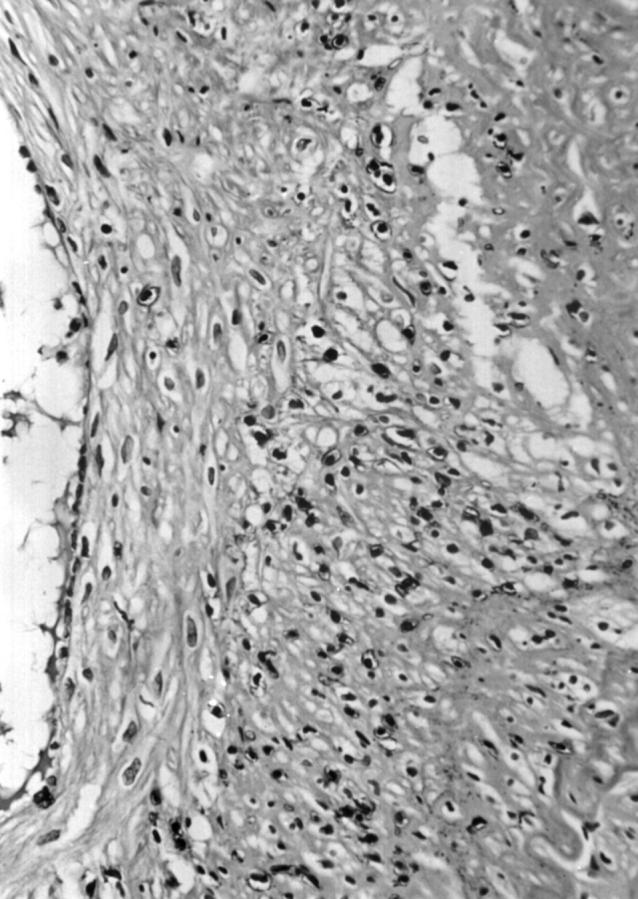
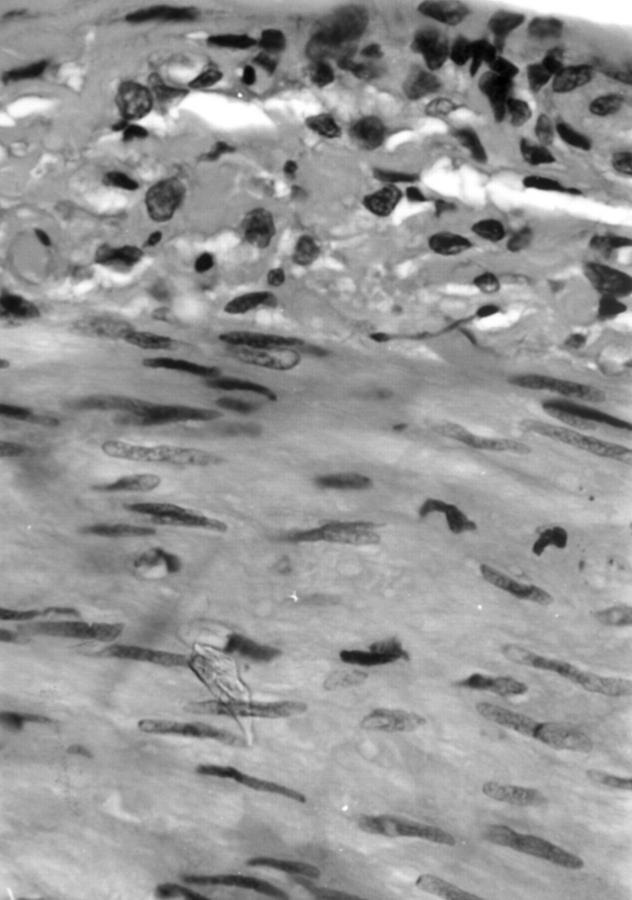
Figure 1 Segment of vessel wall showing active inflammation. Haematoxylin and eosin stain.
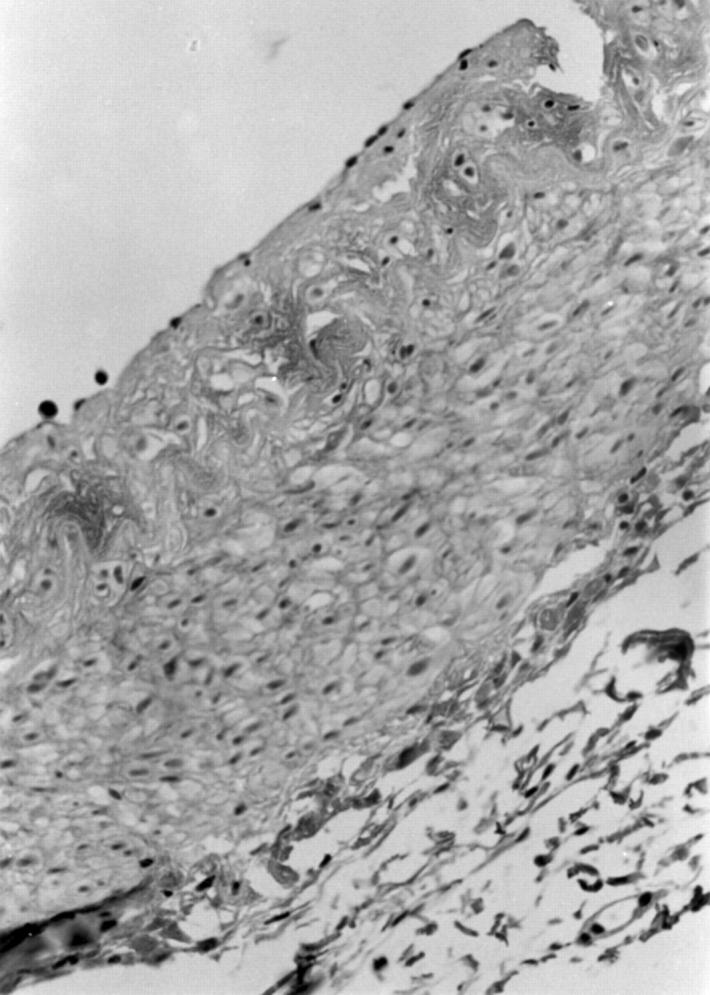
Figure 2 Segment of vessel wall from the same biopsy specimen showing no evidence of mural inflammation (skip lesion). Haematoxylin and eosin stain.
Figure 3 Photomicrograph of leucocyte common antigen (LCA) stain of inflammatory cells in the adventitia of the same vessel wall as in figs 1 and 2, not readily apparent on H&E but confirmed on LCA staining
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Hunder G. G., Bloch D. A., Michel B. A., Stevens M. B., Arend W. P., Calabrese L. H., Edworthy S. M., Fauci A. S., Leavitt R. Y., Lie J. T. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990 Aug;33(8):1122–1128. doi: 10.1002/art.1780330810. [DOI] [PubMed] [Google Scholar]
- Klein R. G., Campbell R. J., Hunder G. G., Carney J. A. Skip lesions in temporal arteritis. Mayo Clin Proc. 1976 Aug;51(8):504–510. [PubMed] [Google Scholar]
- Lie J. T. Temporal artery biopsy diagnosis of giant cell arteritis: lessons from 1109 biopsies. Anat Pathol. 1996;1:69–97. [PubMed] [Google Scholar]
- Sudlow C. Diagnosing and managing polymyalgia rheumatica and temporal arteritis. Sensitivity of temporal artery biopsy varies with biopsy length and sectioning strategy. BMJ. 1997 Aug 30;315(7107):549–549. [PMC free article] [PubMed] [Google Scholar]