Abstract
Objectives To determine the impact on outcomes in patients of the Evercare approach to case management of elderly people.
Design Practice level before and after analysis of hospital admissions data with control group.
Setting Nine primary care trusts in England that, in 2003-5, piloted case management of elderly people selected as being at high risk of emergency admission.
Main outcome measures Rates of emergency admission, emergency bed days, and mortality from April 2001 to March 2005 in 62 Evercare practices and 6960-7695 control practices in England (depending on the analysis being carried out).
Results The intervention had no significant effect on rates of emergency admission (increase 16.5%, (95% confidence interval −5.7% to 38.7%), emergency bed days (increase 19.0%, −5.3% to 43.2%), and mortality (increase 34.4%, −1.7% to 70.3%) for a high risk population aged >65 with a history of two or more emergency admissions in the preceding 13 months. For the general population aged ≥65 effects on the rates of emergency admission (increase 2.5%, −2.1% to 7.0%), emergency bed days (decrease −4.9%, −10.8% to 1.0%), and mortality (increase 5.5%, −3.5% to 14.5%) were also non-significant.
Conclusions Case management of frail elderly people introduced an additional range of services into primary care without an associated reduction in hospital admissions. This may have been because of identification of additional cases. Employment of community matrons is now a key feature of case management policy in the NHS in England. Without more radical system redesign this policy is unlikely to reduce hospital admissions.
Introduction
Case management of frail elderly people was recently introduced into the NHS, through the Evercare pilot projects run by UnitedHealth Europe1 and subsequently became a key component of the national community matron policy.2 Case management aims to improve outcomes in patients and, in particular, to reduce unplanned hospital admission. In the United States, Evercare substantially reduced hospital admissions among residents in nursing homes,3 but the US version of Evercare was markedly different to the version in the United Kingdom as the former included intensive domiciliary nursing care of patients when they became ill.
A systematic review of home based support for older people found no overall impact on hospital admission.4 A wider review of integrated care experiments in elderly people, however, suggested that they can reduce admission rates and costs of care, but these effects are highly dependent on the system of care.5 Two further reviews concluded that there is limited evidence that case management of elderly people can reduce use of health services, but both suggest that the results from individual studies cannot readily be generalised to different healthcare settings.6 7 The authors suggest that the effects of complex approaches to case management probably depend on the nature of the intervention and on the context in which it is introduced.
In England case management was introduced in the Evercare pilots in April 2003. Evercare sites initially selected patients on the basis of age (≥65) and two or more emergency admissions in the previous year. Over time the selection criteria for patients were broadened, though they generally still included a history of emergency admissions. The selection criteria identified some patients who were not in contact with regular primary care or community services but who could potentially benefit from case management. An advanced practice nurse carried out a comprehensive geriatric assessment,8 using structured assessment tools, and a physical examination, which resulted in an individualised care plan agreed with the patient, the general practitioner, and other staff. Patients were then monitored at a frequency determined by their classification of risk. The benefits that the nurses reported included altering medication to avoid adverse reactions, coordinating care to reduce fragmentation among services, arranging access to community based services, and a range of other interventions. They judged that the intervention improved patients' functional status and quality of life and avoided hospital admissions.9
We carried out a quantitative and qualitative evaluation of the Evercare pilots. The qualitative part included interviews with staff from UnitedHealth and primary care trusts, general practitioners, patients, carers, and advanced practice nurses, and the findings from these are reported elsewhere.10 11 In this paper we report on the effect of Evercare pilots on hospital admissions, bed days, and mortality.
Methods
Study population and outcomes
The Evercare intervention pilots started in nine primary care trusts on 1 April 2003, though few patients were enrolled before 1 July 2003,1 which we took as the start of the intervention. The intervention pilots ran until June 2004, though the intervention was continued in all nine trusts at least until the end of our study period (31 March 2005). The intervention practices (n=64) were those that had patients enrolled in Evercare at any time between 1 July 2003 and 31 March 2005.
We took as the control group all other practices in England, excluding practices with incomplete data, non-Evercare practices in the nine trusts that were piloting Evercare, practices in a small number of trusts that we were aware had introduced similar interventions, and practices with particularly high or low rates of emergency admissions. The number of control practices varied between 6960 and 7695, depending on the analysis being carried out.
Our data on the Evercare patients were limited to their practice, age, sex, and dates of enrolment and discharge from Evercare. As we did not have information on their use of NHS services and could not identify and track individual Evercare patients in hospital episode statistics (HES), we measured outcomes at practice level.
The outcomes were practice rates of emergency admissions, emergency bed days, and mortality estimated from hospital episode statistics. These statistics record deaths for patients admitted to hospital if they die in hospital or if they die outside hospital up to one month after the end of the hospital statistics year (April to March) in which they were admitted. This measure of mortality is therefore an underestimate of the total mortality of patients in a practice as it fails to count the deaths outside hospital of patients who die more than one month after the HES year in which they were last admitted to hospital.12 However, it represents the best available national data on mortality at practice level.
We measured outcome rates for two populations: a high risk cohort of patients aged ≥65 with two or more emergency admissions in the preceding 13 months (similar to the original entry criteria for Evercare1) and all patients aged ≥65 (the general ≥65 population). We included the latter group in the analysis to allow for the possibility that the intervention had spillover effects into the wider population of elderly people. For our analysis of the high risk cohort we could not construct a high risk cohort for before the intervention for two Evercare practices as data for 2000-1 were not available in hospital episode statistics, so the intervention group has 62 practices for this analysis.
To estimate outcomes for the high risk cohort we used two denominators. The first was the initial number of patients in the cohort.13 The second denominator was number of patient years at risk, derived by subtracting deaths in the hospital episode statistics from the estimate of the surviving high risk population at the beginning of the period being analysed and calculating person years at risk as the mean of initial and final populations for the period. The first calculation has more policy relevance as knowing that the intervention reduced the admission rate per person years at risk does not allow us to conclude that it has reduced total admissions unless we also know that mortality was unchanged.
The numerator for the outcome rates for the general ≥65 population was the number of admissions, bed days, or deaths during the period for patients aged ≥65 registered with the practice at the time of admission. The denominator was the practice population aged ≥65.
Analysis
As practices were not randomised into Evercare and control groups we used a design that compared the change in outcomes in the Evercare practices before and during the intervention with the change in outcomes in the control practices before and during the intervention.14 This design removes the effect of baseline differences between the groups.
We defined three periods before the intervention (period 1: July 2001 to March 2002; period 2: April 2002 to September 2002; period 3: October 2002 to March 2003) and three during the intervention (period 4: July 2003 to March 2004; period 5: April 2004 to September 2004; period 6: October 2004 to March 2005). We then compared period 4 against period 1, 5 against 2, and 6 against 3 to remove possible seasonal effects. To allow for the slow implementation of the intervention, and because of possible delayed effect, we have reported the effects of the intervention between period 6 and period 3 for intervention and control groups. Comparisons between other time periods did not alter our conclusions.10
We regressed the outcome rate on indicators to denote the period being analysed, an indicator for the intervention group, and interactions between the intervention group indicator and the period indicators. The effect of the intervention in period 6 was estimated as the coefficient on the interaction of the intervention indicator and the period 6 indicator minus the coefficient on the interaction of the intervention indicator and the period 3 indicator. The effects for period 4 and 5 were estimated in a similar way. The regressions were run with STATA v9, with most models using a fixed effects panel data estimator with robust standard errors and clustering within practices to allow for any serial correlation of errors.
In some of the regression analyses, we included a measure of the proportion of the practice's patients enrolled in Evercare. Other models included the population denominator as an additional explanatory variable to allow for possible bias due to measurement error. Full details of the statistical methods used are available elsewhere.10
We also controlled for differences between Evercare and control practices using propensity score matching.15 16 This method allowed us to compare Evercare practices with control practices that were similar in terms of the factors that influenced the probability of a practice being enrolled in Evercare. We used a probit regression model to predict the probability (or propensity score) that a practice would be enrolled in Evercare using the total list size, the attributed health deprivation score from the index of multiple deprivation,17and the average growth rate in emergency admissions for the ≥65 population as predictors. We stratified practices by propensity scores to compare the change in the outcome rate for Evercare practices with the change in the outcome rate for control practices.
As the intervention could have reduced the rates of increases in any of the outcomes, we repeated both the regression and the matching analyses to test for an effect of the intervention on the growth rates.
Results
Table 1 shows the baseline characteristics for the groups. At baseline, intervention practices had significantly higher rates of admission and use of emergency bed days and faster growth rates in admissions for the general population aged ≥65. Although intervention practices had more high risk patients, the outcomes of their high risk population were similar to those in the control practices. Intervention practices also served populations with more health deprivation.
Table 1.
Baseline characteristics of intervention and control practices. Figures are means (SD) unless otherwise stated
| Intervention group (n=64) | Control group | No in control group | Standardised difference* | P value† | |
|---|---|---|---|---|---|
| Outcomes in high risk cohort‡ before intervention (period 3§) | |||||
| Emergency admission/patient/year | 0.56 (0.50) | 0.58 (0.36) | 7811 | −0.05 | 0.70 |
| Emergency bed days/patient/year | 6.96 (5.25) | 6.63 (7.37) | 7799 | 0.05 | 0.63 |
| HES mortality | 0.09 (0.09) | 0.10 (0.13) | 7710 | −0.07 | 0.436 |
| Outcomes in population aged ≥65 (period 3§) | |||||
| Emergency admission/patient/year | 0.23 (0.07) | 0.21 (0.07) | 7695 | 0.38 | 0.01 |
| Emergency bed days/patient/year | 3.042 (0.86) | 2.56 (1.00) | 7672 | 0.482 | 0.00 |
| HES mortality | 0.05 (0.02) | 0.05 (0.02) | 7653 | 0.212 | 0.11 |
| Other characteristics of practices | |||||
| Average growth in admissions¶ | 0.13 (0.26) | 0.03 (0.20) | 7589 | 0.48 | 0.00 |
| Total on practice list | 7596 (3325) | 6148 (3745) | 7589 | 0.39 | 0.00 |
| Index of multiple deprivation-health | 0.64 (0.89) | 0.26 (0.93) | 7589 | 0.40 | 0.00 |
| Proportion aged ≥65 | 0.16 (0.05) | 0.15 (0.05) | 7589 | 0.06 | 0.60 |
| Proportion of women aged ≥65 | 0.57 (0.04) | 0.56 (0.04) | 7589 | 0.19 | 0.08 |
| Number in high risk population | 32.24 (17.17) | 24.00 (18.69) | 7589 | 0.44 | 0.00 |
| Proportion of high risk population | 0.03 (0.01) | 0.026 (0.01) | 7589 | 0.32 | 0.03 |
| List/whole time equivalent GP | 2138 (628) | 2125 (599) | 7589 | 0.02 | 0.87 |
| Low income scheme index** | 12.56 (7.12) | 11.48 (7.86) | 7589 | 0.14 | 0.23 |
*Standardised difference: intervention group mean minus control group mean divided by pooled SD.
†t test for differences in means.
‡N=62 as HES data for 2000-1 for two intervention practices could not be found.
§October 2002 to March 2003. Pre-intervention high risk cohort: 65+, 2+emergency admissions in 13 months to 31 January 2001, not recorded as dead in HES by 1 July 2001. Post-intervention high risk cohort population: number of patients 65+, 2+ emergency admissions in 13 months to 31 January 2003, not recorded as dead in HES by 1 July 2003.
¶Growth rate in emergency admissions in those aged ≥65 is geometric mean of growth rates in four years to 2002-3.
**Proportion of prescriptions dispensed without charge on grounds of low income.
The results from the multiple regression probit models (see table A1 on bmj.com) showed that practices with a larger total list, with a higher health deprivation score, and with a higher growth rate in admissions were more likely to be in the intervention group. We therefore included these variables in the matched control analyses. The other variables in table 1 had no significant effect on the probability of being an Evercare practice.
Tables 2 and 3 show the effect of the intervention as the estimated change in outcome between the last period before the intervention (period 3) and the last period during the intervention (period 6) for the Evercare practices minus the estimated change between period 3 and period 6 for the control practices. We report the effect of the intervention on the level of the three outcome measures and also as a percentage of the baseline rate in period 3. Table 2 shows the effects of the intervention in high risk patients (aged ≥65 and two admissions in the previous 13 months). The rates of admission and bed days and mortality were all higher in the intervention group, though none of the effects was significant at the 5% level. Table 3 presents the results for the general population aged ≥65, showing that the rate of admissions and mortality were higher in Evercare practices and the bed day rate reduced. But again, none of these differences was significant.
Table 2.
Effect of intervention for the high risk population (aged ≥65, two emergency admissions in preceding 13 months) in 62 intervention practices and at least 6960 control practices. Effects shown with 95% confidence intervals
| Outcome | Regression based estimates* | Propensity score matched estimates† | |||||
|---|---|---|---|---|---|---|---|
| Estimated effect‡/ person/year | Percentage effect§ (%) | P value¶ | Estimated effect‡/person/year | Percentage effect§ (%) | P value¶ | ||
| Emergency admissions | 0.10 (−0.03 to 0.22) | 16.5 (−5.7 to 38.7) | 0.14 | 0.09 (−0.03 to 0.22) | 16.3 (−6.0 to 38.5) | 0.15 | |
| Emergency bed days | 1.3 (−0.4 to 3.0) | 19.0 (−5.3 to 43.2) | 0.13 | 1.08 (−0.61 to 2.77) | 15.6 (−8.7 to 39.9) | 0.21 | |
| HES mortality | 0.03 (0.0 to 0.07) | 34.3 (−1.7 to 70.3) | 0.06 | 0.03 (0.0 to 0.07) | 34.9 (−1.1 to 71.1) | 0.06 | |
*From fixed effect panel regression, allowing for clustering within practices and heteroscedasticity.
†From matching by propensity score and stratification.
‡Estimated change (period 6 minus period 3) in mean outcome for intervention minus control. Period 3=six months from October 2002; period 6=six months from October 2004.
§100*estimated effect/mean outcome rate for Evercare practices in period 3.
¶For two sided test of null hypothesis of no effect. Rates for high risk cohort in period 3 are per person in cohort at 1 July 2001 and those for after intervention in high risk population in period 6 are per person in cohort at 1 July 2003.
Table 3.
Effect of intervention for the general practice population aged ≥65 in 64 intervention practices and at least 6938 control practices. Effects shown with 95% confidence intervals
| Outcome | Regression based estimates* | Propensity score matched estimates† | |||||
|---|---|---|---|---|---|---|---|
| Estimated effect‡/person/year | Percentage effect§ (%) | P value¶ | Estimated effect/person/year | Percentage effect§ (%) | P value¶ | ||
| Emergency admissions | 0.01 (−0.01 to 0.02) | 2.5 (−2.1 to 7.0) | 0.29 | 0.005 (−0.005 to 0.016) | 2.3 (−2.2 to 6.7) | 0.31 | |
| Emergency bed days** | −0.15 (−0.33 to 0.03) | −4.9 (−10.8 to 1.0) | 0.10 | −0.17 (−0.35 to 0.002) | −5.7 (−11.4 to 0.1) | 0.05 | |
| HES mortality | 0.003 (−0.002 to 0.007) | 5.5 (−3.5 to 14.5) | 0.23 | 0.003 (−0.001 to 0.007 | 5.7 (4.9 to 14.2) | 0.19 | |
*From fixed effect panel regression, allowing for clustering within practices and heteroscedasticity.
†From matching by propensity score and stratification.
‡Estimated change (period 6 minus period 3) in mean outcome for intervention minus control. Period 3=six months from October 2002; period 6=six months from October 2004.
§100*estimated effect/mean outcome rate for Evercare practices in period 3.
¶For two sided test of null hypothesis of no effect.
**Estimated from models with log of emergency bed days as dependent variable.
The results were the same when we used patient years at risk as the denominator for the analysis of the high risk group (see table A2 on bmj.com) and when we included a measure of practice population exposure or the rate denominator in the regression models in an attempt to allow for errors in population measurement. The intervention then had positive but non-significant effects on the growth rates of admissions, bed days, and mortality for both the high risk cohorts (see table A3 on bmj.com) and for the general population aged ≥65.
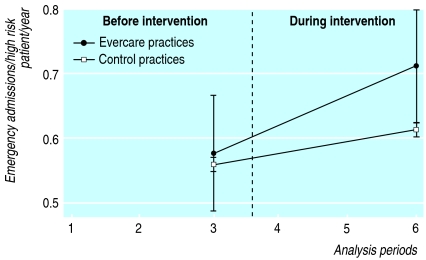
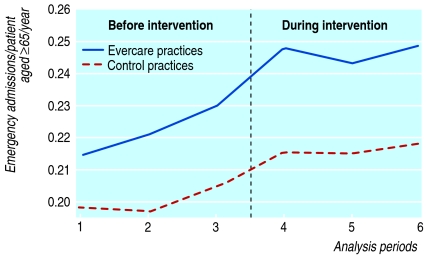
Figures 1 and 2 illustrate differences in admission rates in high risk patients before and during the intervention (fig 1) and in the general population aged ≥65 (fig 2). The rates for the high risk group are expressed in terms of the initial cohort of patients. In period 3 (the last period before the intervention) the admission rates were slightly higher in the Evercare practices than in the control practices. By period 6 (the last intervention period) all practices had higher admission rates than before the intervention, but the increase was greater in the Evercare practices. None of the changes potentially attributable to the Evercare intervention was significant.
Fig 1 Emergency admission rates in two high risk cohorts in Evercare and control practices. Period 3 (last before intervention): 1 October 2002 to 31 March 2003; period 6 (last intervention period): 1 October 2004 to 31 March 2005. Emergency admission rate in period is number of admissions in period divided by initial size of cohort at 1 July 2001 (for before intervention) or 1 July 2003 (for during intervention) all multiplied by 2. Bars on vertical lines denote 95% confidence intervals
Fig 2 Emergency admission rates for general population aged ≥65 in Evercare and control practices. Before intervention: period 1: 1 July 2001 to 31 March 2002; period 2: 1 April 2002 to 30 September 2002; period 3: 1 October 2002 to 31 March 2003). During intervention: period 4: 1 July 2003 to 31 March 2004; period 5: 1 April 2004 to 30 September 2004; period 6: 1 October 2004 to 31 March 2005
Discussion
The Evercare pilots represent the first widespread implementation of case management in the NHS. Our qualitative evidence suggests that access to case management added a frequency of contact, regular monitoring, psychosocial support, and a range of referral options that had not previously been provided to frail elderly people, and in some cases nurses reported that they had been able to intervene to avoid admission.10 In this quantitative analysis, however, we found that case management had no significant impact on rates of emergency admission, bed days, or mortality in high risk cohorts. These results are consistent with those from a small case-control study from a single Evercare site18 and with the limited evaluation at patient level published by UnitedHealth Europe.1 9
Caveats on interpretation
Our criterion for defining the high risk group was based on data from hospital episode statistics and does not correspond exactly with the criteria used to select Evercare patients. However, there is probably considerable overlap between our high risk group and Evercare patients as at least 69% of Evercare patients had two or more emergency admissions in the previous 13 months.9 The small number of intervention practices meant that the study had relatively low power to detect changes in outcomes. Our estimates of power suggest that the study was adequately powered to detect outcome changes of 25% for the high risk population and 10% for the general population aged ≥65.
We did not collect data on a range of other important outcomes, especially on any direct measures of the health of the target population. The intervention and control practices had different admission rates at baseline, though both our regression based estimates and the matched control analyses controlled for these.
Our estimate of mortality failed to count some deaths outside hospital, and we probably underestimated mortality less in practices with higher rates of admission as more of their patients who die will have been in hospital recently and hence have their death recorded by hospital episode statistics. But if the intervention is successful in reducing admission rates, the death rate recorded in the hospital episode statistics for intervention practices after the intervention could be reduced even if there is no real effect of the intervention on mortality. Hence our estimates of the effect of the Evercare intervention on mortality may be biased in its favour. Our finding was, if anything, an increase in recorded mortality as a result of the intervention.
The apparent conflict between nurses' accounts of avoided admissions in the qualitative data and this quantitative analysis may arise because Evercare led to increased case finding. Two commentators on the Australian coordinated care trials suggested: “The possibility remains that the essential premise that better coordination reduces hospitalisation is misguided . . . better care coordination [may] reveal unmet needs rather than resolving them.”19
The introduction of case management of frail elderly people into the NHS provided an additional range of services in primary care without reducing hospital admissions. Although lessons have been learnt from these initial pilots—for example, better methods of identifying high risk groups20—we predict the same outcome from the newly introduced community matron policy, as the community matron model is based on the same principles as Evercare advanced primary nurses. Community matrons are likely to be popular with patients and increase access to care, but they are unlikely to reduce hospital admissions unless there is also a more radical system redesign.
What is already known on this topic
Case management of frail elderly people can affect outcomes, depending on the context in which it is introduced
The NHS introduced case management using the Evercare approach provided by UnitedHealth Europe in nine trusts in England
Employment of community matrons is now a key feature of case management policy in the NHS in England
What this study adds
Evercare's approach to case management in the NHS in England did not reduce emergency admissions, emergency bed days, or mortality
Supplementary Material
Contributors: All authors contributed to the design and execution of the overall evaluation. HG and MD designed and carried out the quantitative analyses. All authors commented on the analysis and contributed to writing the paper. MR is guarantor.
Funding: Department of Health grant to the National Primary Care Research and Development Centre.
Competing interests: None declared.
Ethical approval: Thames Valley multi-centre ethics committee.
References
- 1.UnitedHealth Group. Implementing the Evercare programme. Interim report. London: UHG, 2004. www.networks.nhs.uk/40.php#Evercar.
- 2.Department of Health. Supporting people with long term conditions: liberating the talents of nurses who care for people with long term conditions. London: Department of Health, 2005.
- 3.Kane R, Keckhafer G, Flood S, Bershadsky B, Siadaty M. The effect of Evercare on hospital use. J Am Geriatr Soc 2003;51:1427-34. [DOI] [PubMed] [Google Scholar]
- 4.Elkan R, Kendrick D, Dewey M, Hewitt M, Robinson J, Blair M, et al. Effectiveness of home based support for older people: systematic review and meta-analysis. BMJ 2001;323:719-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johri M, Beland F, Bergman H. International experiments in integrated care for the elderly: a synthesis of the evidence. Int J Geriatr Psychiatry 2003;18:222-35. [DOI] [PubMed] [Google Scholar]
- 6.Hutt R, Rosen R, McCauley J. Case managing long term conditions. London: King's Fund, 2004. www.kingsfund.org.uk/resources/publications/case_managing.html.
- 7.Singh D. Transforming chronic care: evidence about improving care for people with long term conditions. Birmingham: Health Services Management Centre, University of Birmingham, 2005. www.hsmc.bham.ac.uk/news/Improving%20Care-Apr06.pdf.
- 8.Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet 1993;342:1032-6. [DOI] [PubMed] [Google Scholar]
- 9.UnitedHealth Europe. Assessment of the Evercare programme in England 2003-2004. www.cat.csip.org.uk/_library/evercare%20final%20report.pdf
- 10.Boadeb R, Dusheiko M, Gravelle H, Parker S, Pickard S, Roland M, et al. Evaluation of Evercare: final report. Manchester: National Primary Care Research and Development Centre, University of Manchester, 2006. www.npcrdc.ac.uk/pr33
- 11.Boaden R, Dusheiko M, Gravelle H, Parker S, Pickard S, Roland M, et al. Evaluation of Evercare: executive summary. Manchester: National Primary Care Research and Development Centre, University of Manchester, 2006. www.npcrdc.ac.uk.es42
- 12.HESonline. HES extract pack. NHS information centre, 2006.www.hesonline.org.uk.
- 13.Roland M, Dusheiko M, Gravelle H, Parker S. Follow up of people aged 65 and over with a history of emergency admissions: analysis of routine admission data. BMJ 2005;330:289-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wooldridge JM. Econometric analysis of cross section and panel data. Cambridge, MA: MIT Press, 2002.
- 15.Rubin DB. Estimating causal effects for large data sets using propensity scores. Ann Intern Med 1997;127:757-63. [DOI] [PubMed] [Google Scholar]
- 16.Becker SO, Ichino A. Estimation of average treatment effects based on propensity scores. Stata Journal 2002;2:358-77. [Google Scholar]
- 17.Department of Environment, Transport and the Regions. Indices of deprivation 2000. London: DETR, 2000. (Regeneration Research Summary No 31, 2000.) www.communities.gov.uk/pub/632/IndicesofDeprivation2000summaryPDF158Kb_id1128632.pdf
- 18.Patrick H, Roberts N, Hutt R, Hewitt P, Connelly J, Oliver D. Evaluation of innovations in nursing practice: report and discussion. Br J Nursing 2006;15:520-3. [DOI] [PubMed] [Google Scholar]
- 19.Esterman AJ, Ben-Tovim DI. The Australian coordinated care trials: success or failure? Med J Aust 2002;177:469-70. [DOI] [PubMed] [Google Scholar]
- 20.Billings J, Dixon J, Mijanovich T, Wennberg D. Case finding for patients at risk of readmisison to hospital: development of algorithm to identify high risk patients. BMJ 2006;333:327-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.