Abstract
Objective: Strategies to effectively and efficiently screen for depression remain elusive in the primary care setting. The purpose of this study was to assess the feasibility of a depression screening program in which patients completed a validated questionnaire in the waiting room. Using Optical Mark Reader technology (PatientLink), patient responses were interfaced into the electronic health record (EHR), where the responses and score were available to practitioners at the time of the visit.
Method: This was a prospective, observational study that enrolled all consenting patients, aged 18 years and older, who spoke English and arrived for any type of visit during a 1-week period at a family practice clinic (the first week of August 2004). Patient feedback was sought using a standardized survey. Feedback from practitioners and staff was sought using focus group methodology. The primary outcome measure was the proportion of patients successfully screened for depression by the front desk personnel using PatientLink.
Results: A total of 189 patients met eligibility criteria. Of those, 169 (89.4%) were successfully screened for depression. Of the patients who completed PHQ-9 questionnaires, 30 (17.8%) met DSM-IV criteria for moderate to severe depression. Four (2.4%) of these subjects with major depressive disorder were found not to have preexisting documentation of a depressive disorder in the medical record. In no case was the lack of successful screening due to technology error. Patients, staff, and practitioners supported this new screening strategy. No additional staff were needed to conduct the screening program.
Conclusion: This study demonstrates that depression screening using a Scantron-based PHQ-9 questionnaire completed by patients in the waiting room and uploaded into an EHR is technically feasible and resource efficient.
Depression is a common disorder associated with significant psychosocial and physical impairment as well as increased mortality. The direct and indirect cost of depression has been estimated at $44 billion per year, placing it among the top 10 most costly illnesses in the United States.1 Lost years of healthy life attributed to depression is second only to ischemic heart disease.2 The majority of patients with depression seek treatment from their primary care provider (PCP).3 Evidence suggests that depression screening programs are associated with improved patient outcomes, particularly when screening is coupled with systems that also support adequate treatment and monitoring.4 On the basis of this evidence, the U.S. Preventive Services Task Force (USPSTF) recommends screening adults for depression in clinical practices that have systems to assure accurate diagnosis, effective treatment, and follow-up.2 However, in the current primary care environment, up to half of all depressed patients go unrecognized.5 In 15 randomized controlled trials evaluating depression screening in primary care, 14 utilized research staff to accomplish the screening activities.6–20 Although information from these studies has resulted in the recommendation to screen adults for depression, these studies did little to illuminate optimal methods for accomplishing the task. In the single study that utilized existing clinic staff to conduct depression screening, the staff were registered nurses and received extensive training.20 Increasingly, financial constraints are causing community-based primary care clinics to replace the role of nurses with medical assistants. Thus, the staffing and expense required to administer a routine depression screening process remains a significant barrier to implementation.
A caveat of the USPSTF recommendation to screen all adults for depression is that screening be coupled with a diagnosis, treatment, and monitoring support system. Inherent in such “support systems” or disease management programs is the ability to accurately identify the population targeted for management. The increasing prevalence of electronic health records (EHRs) in the primary care environment provides access to accurate and timely information, facilitating disease management programs.21 However, depression screening results, unlike vital signs and laboratory data, are not routinely entered and stored in EHR systems.
In recognition of these issues, a depression screening process was piloted with the goals of requiring minimal staff, facilitating electronic collection of screening responses, and making the results immediately available to clinicians at the time of the visit. Accordingly, we proposed (1) shifting the time burden of depression screening from clinic personnel to the patient in an attempt to reduce the resources required to accomplish screening and (2) using information technology to capture and store patient responses prior to the patient's examination. Therefore, this study was conducted to determine if it is feasible to accomplish depression screening in a primary care office waiting room using a patient-completed questionnaire and Optical Mark Reader (OMR) technology that interfaces with an EHR.
METHOD
This was a prospective, observational study approved by the local institutional review board. The study was funded internally by the Providence Primary Care Research Network. Research investigators and staff have no affiliation with the purveyors of the technology evaluated in this study and report no conflict of interest.
Setting and Study Population
This study was conducted at one clinic in the Providence Primary Care Research Network in Oregon. The Providence Milwaukie Family Medicine Clinic was selected on the basis of their adoption of a paper-based depression screening process 6 months prior to study initiation.
All patients, 18 years of age or older, seen in the clinic during the first week of August 2004 were eligible for participation in the study. Subjects were excluded if they were not proficient in the English language.
Screening Strategy
The Providence Primary Care Research Network had previously evaluated depression screening tools appropriate for the primary care environment. The Primary Care Evaluation of Mental Disorders (PRIME-MD) Patient Health Questionnaire–Depression Subscale 9 (PHQ-9)22 was selected because it is short, is self-administered by the patient, assesses the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria, evaluates disease severity, performs well (75% sensitivity, 90% specificity, and 85% overall accuracy), and has been validated in many primary and tertiary care populations.23 Since the clinics in the Research Network utilize the Centricity EHR (GE Healthcare, Hillsboro, Ore.) and are predominantly paperless, a patient depression screening strategy that would interface with the EHR system was sought. PatientLink (PatientLink, Inc., Harrisonville, Mo.) was selected for 2 reasons. First, Scantron-based questionnaires (Scantron, Irvine, Calif.) are a common and widely accepted format for patient self-administered surveys. Second, PatientLink uses OMR technology to capture patient Scantron responses and upload the information into the EHR, where practitioners can immediately view the results.
All eligible patients arriving for any type of visit who provided consent to participate in the study were asked to complete the PHQ-9 Scantron. Since the primary objective of the pilot project was feasibility of the screening strategy in actual practice, research staff were not involved in the screening process. The purpose and suggested work flow of the depression screening process were presented at a staff meeting. The work flow entailed the front desk personnel's distributing the depression screening Scantron along with brief written patient instructions at the time of check-in. Completed Scantron questionnaires were returned to front desk personnel, who inserted the card into the OMR scanner. The Scantron cards were scanned through the PatientLink OMR in approximately 5 seconds, making the information immediately available to practitioners upon opening the patient's chart in the EHR. A single mouse click was required to view the completed questionnaire. Although practitioners and staff were introduced to the study's purpose and methods, they were not given specific instructions or education on handling PHQ-9 results once they were interfaced into the EHR.
Data Collection and Analysis
The primary outcome measure was the proportion of patients successfully screened for depression by front desk personnel using PatientLink. Any subject was considered to have met the primary outcome if the PHQ-9 questionnaire was completed and imported into the EHR prior to the patient's entering the examination room.
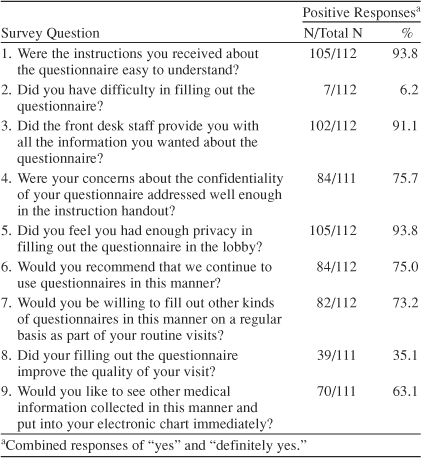
Several secondary outcome measures ascertained the performance of the technology and the patient, staff, and practitioner perspectives on the screening strategy. At the end of the clinic visit, patients were invited to complete a 9-item survey to ascertain their perspective on the instructions, privacy, process, and value of the screening strategy. For purposes of reporting the results of the PatientLink Satisfaction Survey, affirmative responses (“yes” and “definitely yes”) were grouped and described by percentages (see Table 1).
Table 1.
PatientLink Satisfaction Survey and Number of Patients With a Positive Response for Each Question
The perspectives of staff and practitioners were solicited during 2 separate focus group sessions conducted within 2 weeks of the study. Semistructured moderator's guides were constructed for the focus groups. An experienced moderator facilitated each discussion in keeping with the interview guide. A research assistant recorded the groups' responses. Transcripts of the sessions were analyzed by 2 investigators (J.S.H. and B.H.L.) to generate lists of key ideas reflecting the groups' sentiments. Key ideas were clustered into categories and themes were identified. The authors then discussed the themes, reaching consensus on the final emergent topics.
RESULTS
A total of 189 patients met eligibility criteria during the 1-week study. Of those, 169 (89.4%) successfully met the primary outcome measure based on an imported PHQ-9 result available in the EHR prior to the patient's entering the exam room. There were 20 occurrences of unsuccessful depression screening. Half of these cases involved patients who were too ill to complete the PHQ-9 in the lobby prior to the visit. In this study, only 5 (2.6%) of the 189 patients refused to complete the PHQ-9 survey. In no case was the lack of successful screening due to error of the PatientLink technology.
Among the 169 PHQ-9 questionnaires successfully scanned into the EMR, 14 (8.3%) had 1 or more items left blank. The items most commonly left blank asked about “poor appetite or overeating” and “thoughts that you would be better off dead or of hurting yourself in some way.” Both of these questions were left blank on 4 (2.4%) questionnaires. In only one instance did a primary care provider amend the scanned patient PHQ-9 responses during the course of the visit. In that case, the provider changed a patient's initial response.
Diagnosis of Depression
Of the subjects who completed PHQ-9 questionnaires, 30 (17.8%) met the DSM-IV criteria for moderate to severe depression as defined by a PHQ-9 score of 10 or higher. Four (2.4%) of these subjects were found not to have a preexisting diagnosis of a depressive disorder in the medical record. The mean PHQ-9 score of these 4 subjects was 17.3 (SD = 5.6).
Patient Perspective
Of the 169 subjects completing the PHQ-9 questionnaire, 66% also agreed to complete the PatientLink Satisfaction Survey following their visit. As seen in Table 1, most subjects felt the instructions were easy to understand, reported no difficulty in completing the questionnaire, felt the brief introduction from the front desk personnel was sufficient, and reported having enough privacy in the lobby. Somewhat fewer subjects felt their concerns regarding the confidentiality of their PHQ-9 responses were sufficiently addressed. Of the 27 subjects with confidentiality concerns, however, only 9 would also refrain from recommending continued use of the PHQ-9 questionnaire and 11 would not wish to fill out other types of questionnaires. Almost an equal number of subjects felt that the depression screening strategy improved the quality of their visit (35%) as compared to 39% who felt that it did not improve the quality of the visit.
Staff Perspective
A total of 11 staff attended the focus group meeting, including 4 front desk personnel and 7 medical assistants. In response to questions regarding the process involved in implementing the screening program, the front desk personnel felt that the process worked well. Despite the potential burden of distributing the PHQ-9 questionnaire and then collecting and scanning the forms prior to each subject's visit, staff did not feel that it detracted from their ability to perform their normal work activities. They felt that patients were able to follow the printed directions given to them without the need for further instruction. When asked about the functionality of the PatientLink technology, they reported that it took one day to acclimate to the additional noise and workflow adjustment, but that it performed without problems.
The perspective of the medical assistants differed, reflecting their distinct job responsibilities in the clinic. Medical assistants reported a disruption in workflow based on a delay in rooming patients who were still completing surveys. To remedy this problem, they suggested the screening workflow be altered to allow the flexibility to complete the screening and scanning of results after rooming the patients. They did report that the PatientLink depression screening process reduced their direct workload by replacing a previous process in which they were expected to ask each patient 2 depression screening questions, give the paper PHQ-9 survey to patients who screened positive, and then enter the patients' PHQ-9 responses into the EHR. Staff reported a high degree of patient acceptance with the screening program.
Practitioner Perspective
Five of 7 clinicians participating in the study were available to also participate in the focus group session. Practitioners reported that the use of PatientLink technology was a powerful tool for depression screening and resulted in improved chart documentation. Notably, practitioners rarely needed to alter patient self-administered PHQ-9 responses after interviewing the patient. There was significant variance in the reported frequency of viewing interfaced PHQ-9 data. Although some practitioners reported viewing the information during most visits, others reported seldom viewing the information. Physicians who commonly viewed the information in the EHR reported 2 additional benefits of accessing the PHQ-9 results. First, the information was beneficial in determining if currently treated patients with depression had successfully achieved remission. Second, having the information available for documentation in the patient record could facilitate higher reimbursement coding levels. Like medical assistants, practitioners were concerned about the potential for depression screening in the lobby to delay rooming the patients. However, they believed that the workflow could be sufficiently modified to facilitate a timely workflow and were interested in expanding the pilot to collect additional information (e.g., new patient histories, review of systems) using Scantron-based technology.
DISCUSSION
This pilot demonstrated that a Scantron-based PHQ-9 questionnaire with responses uploaded into an EHR prior to the office visit is technically feasible and requires minimal staff resources. Unlike previous depression screening programs that notified physicians in the EHR within approximately 24 hours of depression screening,24,25 the strategy studied in this pilot provides the practitioner with the information at the time of the office visit when there is the opportunity to immediately interact with the patient. This strategy identified a total of 30 subjects (17.8%) meeting criteria for moderate to severe depression based on PHQ-9 score. This identification rate is lower than generally reported in the literature.4 Of those screening positive, 4 subjects (2.4%) were previously undiagnosed according to their medical records. It is unknown if these were cases of depression that would have otherwise been identified during the visit. Patient acceptance of this screening strategy was predominantly positive. Given that the prevalence of depression is 6% to 10%,26 numerous patients without depression will be subjected to mass depression screening without personal benefit. However, it is important to recognize that approximately one third of participants felt that this screening strategy improved the quality of their visit. Although 75% of survey respondents felt their concerns regarding confidentiality were sufficiently addressed, future screening programs might explore better ways to address the concerns of the remaining 25%.
Given that a pilot goal was to minimize clinic resources involved in depression screening, feedback from staff was encouraging. Front desk personnel felt the program was important and did not interfere with other duties. Medical assistants were pleased to shift the burden of depression screening to this patient self-administered strategy. However, they were concerned about the possible delay in rooming patients.
This study also showed a favorable physician response. Practitioners were not surprised that relatively few new cases of depression were detected using this screening strategy, as their clinic had previously implemented a depression screening program. Despite this, physicians felt that the electronic solution offered additional functionality. Specifically, they noted instances in which previously resistant patients felt more comfortable with this screening method. They also recognized an advantage to having the PHQ-9 results available for follow-up of patients with known depression and appreciated the ability to easily support higher reimbursement coding.
This pilot project also had several limitations. First, the study period was limited to 1 week. Further investigation of longer duration may elucidate issues of sustainability. Second, the study was conducted in a single academic family medicine clinic. Since family medicine practitioners provide care to patients throughout the age spectrum, only a portion of the patients attending clinic were eligible for this adult screening program. Further evaluation is needed to determine if these results can be generalized to an internal medicine clinic where potentially all patients attending clinic would be eligible for screening. Third, this pilot program did not include a system to facilitate treatment and monitoring of identified depression cases. However, accurate and timely information is a prerequisite for any disease management program. Only by instituting a program to systematically collect information on depression status of patients with new and preexisting depression can such clinic-based disease management programs be developed.
CONCLUSION
Practical strategies to accomplish depression screening in primary care clinics are of paramount importance. This pilot study demonstrated that the technology employed did accomplish screening of nearly 90% of eligible adults in an academic family practice clinic. The screening strategy was also acceptable to patients, physicians, and staff, with the caveat that an alternative workflow be created for patients who arrive late for their appointment. This depression screening method is notable because it did not involve or require additional staff. Further study is needed to determine if this strategy is equally effective in a busier primary care office with no preestablished depression screening program. Additionally, future investigation should analyze the sustainability of this approach over time and examine the effect of this screening method on patient outcomes.
Pretest and Objectives
Footnotes
This study was funded internally by the Providence Primary Care Research Network. Research investigators and staff have no affiliation with the purveyors of the technology evaluated in this study and report no conflict of interest.
Previously presented at the 25th Forum for Behavioral Science in Family Medicine, Chicago, Ill., September 2004.
The authors thank Patricia A. Bragg, R.H.I.A., Quality Coordinator for Providence Medical Group, who assisted with data collection.
REFERENCES
- Hirschfeld RM, Keller MB, and Panico S. et al. The National Depressive and Manic-Depressive Association consensus statement on the under-treatment of depression. JAMA. 1997 277:333–340. [PubMed] [Google Scholar]
- US Preventive Services Task Force. Screening for depression: recommendations and rationale. Ann Intern Med. 2002;136:760–764. doi: 10.7326/0003-4819-136-10-200205210-00012. [DOI] [PubMed] [Google Scholar]
- Perez-Stable EJ, Miranda J, and Munoz RF. et al. Depression in medical outpatients: underrecognition and misdiagnosis. Arch Intern Med. 1990 150:1083–1088. [DOI] [PubMed] [Google Scholar]
- Pignone MP, Gaynes BN, and Rushton JL. et al. Screening for depression in adults: a summary of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2002 136:765–776. [DOI] [PubMed] [Google Scholar]
- Simon GE, VonKorff M. Recognition, management, and outcomes of depression in primary care. Arch Fam Med. 1995;4:99–105. doi: 10.1001/archfami.4.2.99. [DOI] [PubMed] [Google Scholar]
- Dowrick C. Does testing for depression influence diagnosis or management by general practitioners? Fam Pract. 1995;12:461–465. doi: 10.1093/fampra/12.4.461. [DOI] [PubMed] [Google Scholar]
- Johnstone A, Goldberg D. Psychiatric screening in general practice: a controlled trial. Lancet. 1976;1:605–608. doi: 10.1016/s0140-6736(76)90415-3. [DOI] [PubMed] [Google Scholar]
- Moore JT, Silimperi DR, Bobula JA. Recognition of depression by family medicine residents: the impact of screening. J Fam Pract. 1978;7:509–513. [PubMed] [Google Scholar]
- Linn LS, Yager J. The effect of screening, sensitization, and feedback on notation of depression. J Med Educ. 1980;55:942–949. doi: 10.1097/00001888-198011000-00007. [DOI] [PubMed] [Google Scholar]
- Zung WWK, King RE. Identification and treatment of masked depression in a general medical practice. J Clin Psychiatry. 1983;44:365–368. [PubMed] [Google Scholar]
- Magruder-Habib K, Zung WW, Feussner JR. Improving physicians' recognition and treatment of depression in general medical care: results from a randomized clinical trial. Med Care. 1990;28:239–250. doi: 10.1097/00005650-199003000-00004. [DOI] [PubMed] [Google Scholar]
- Callahan CM, Hendrie HC, and Dittus RS. et al. Improving treatment of late life depression in primary care: a randomized clinical trial. J Am Geriatr Soc. 1994 42:839–846. [DOI] [PubMed] [Google Scholar]
- Callahan CM, Dittus RS, Tierney WM. Primary care physicians' medical decision making for late-life depression. J Gen Intern Med. 1996;11:218–225. doi: 10.1007/BF02642478. [DOI] [PubMed] [Google Scholar]
- Lewis G, Sharp D, and Bartholomew J. et al. Computerized assessment of common mental disorders in primary care: effect on clinical outcome. Fam Pract. 1996 13:120–126. [DOI] [PubMed] [Google Scholar]
- Reifler DR, Kessler HS, and Bernhard EJ. et al. Impact of screening for mental health concerns on health service utilization and functional status in primary care patients. Arch Intern Med. 1996 156:2593–2599. [PubMed] [Google Scholar]
- Williams JW Jr, Mulrow CD, and Kroenke K. et al. Case-finding for depression in primary care: a randomized trial. Am J Med. 1999 106:36–43. [DOI] [PubMed] [Google Scholar]
- Katzelnick DJ, Simon GE, and Pearson SD. et al. Randomized trial of a depression management program in high utilizers of medical care. Arch Fam Med. 2000 9:345–351. [DOI] [PubMed] [Google Scholar]
- Wells KB, Sherbourne C, and Schoenbaum M. et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000 283:212–220. [DOI] [PubMed] [Google Scholar]
- Whooley MA, Stone B, Soghikian K. Randomized trial of case-finding for depression in elderly primary care patients. J Gen Intern Med. 2000;15:293–300. doi: 10.1046/j.1525-1497.2000.04319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rost K, Nutting P, and Smith J. et al. Improving depression outcomes in community primary care practice: a randomized trial of the quEST intervention: quality enhancement by strategic teaming. J Gen Intern Med. 2001 16:143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam KB, Karlan VJ. Electronic medical record systems: trends in large group practices. Group Pract J. 2002;51:18–24. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Rollman BL, Hanusa BH, and Gilbert T. et al. The electronic medical record: a randomized trial of its impact on primary care physicians' initial management of major depression. Arch Intern Med. 2001 161:189–197.correction 2001;161:705. [DOI] [PubMed] [Google Scholar]
- Gill JM, Dansky BS. Use of an electronic medical record to facilitate screening for depression in primary care. Prim Care Companion J Clin Psychiatry. 2003;5:125–128. doi: 10.4088/pcc.v05n0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiatry. 1992;14:237–247. doi: 10.1016/0163-8343(92)90094-q. [DOI] [PubMed] [Google Scholar]



