Abstract
Objective: We sought to derive preliminary estimates of the prevalence of bipolar disorder among a sample of emergency department (ED) patients.
Method: For 1 week in November 2003, consecutive patients aged ≥ 18 years presenting to an urban ED between 8:00 a.m. and midnight were screened for bipolar disorder. We used the National Depression Screening Day protocol, which includes the Mood Disorder Questionnaire. Patients who were severely ill or who had altered mental status were excluded. Demographic factors, past mental health history, and medical history also were assessed.
Results: Of the 212 patients that were approached and eligible, 182 (86%) were enrolled. Our sample's point prevalence for positive screen for bipolar disorder was 6.6% (95% CI = 3.5% to 11.2%).
Conclusion: Nearly 7% of ED patients screened positive for bipolar disorder, which is considerably higher than community estimates of 1.3%. Further prospective research on bipolar disorders among ED patients is needed to further define the scope of the problem and to inform the development of appropriate screening, assessment, and intervention programs.
Bipolar disorder is associated with elevated mortality, functional impairment, and medical/societal costs.1 Recent developments that suggest bipolar spectrum disorders may be more common than once believed argue for heightened awareness among medical and mental healthcare providers.2,3
There are over 110 million emergency department (ED) visits annually.4 The ED often plays a vital role in the identification of disease and intervention for those who would not otherwise find care, such as those with severe psychiatric illnesses. Recently, Hazlett and colleagues5 studied a nationally representative sample of ED visits using the National Hospital Ambulatory Medical Care Survey database. Psychiatric-related ED visits increased by 15% from 1992 to 2000, and they accounted for approximately 5.4% of all ED visits in 2000. However, the Hazlett study used retrospective reviews of medical chart and billing data, a method that is likely to underrepresent the true prevalence of psychiatric conditions in ED patients. We conducted a prospective screening study to obtain preliminary prevalence estimates of bipolar disorder among general population of adult ED patients.
METHOD
Study Design
Using a protocol developed for the National Depression Screening Day (NDSD) (http://www.mentalhealthscreening.org), investigators at an urban, academic ED (Level 1; annual census = 48,000 visits) provided coverage during peak volume hours (8:00 a.m. to midnight) for 7 consecutive days in November 2003. All patients ≥ 18 years old were considered for participation. Exclusion criteria included severe illness (e.g., major trauma, intubation, vomiting), acute distress (e.g., crying, hostility, agitation), contact precautions, cognitive problems preventing interview (e.g., intoxication, delirium, psychosis, dementia), insurmountable language barrier, and refusal to participate. Hospital-provided, Spanish-speaking interpreters assisted with Hispanic patients. All subjects who screened positive for bipolar disorder received an informational brochure and a referral list for outpatient treatment resources, and they were encouraged to discuss their symptoms with their primary care provider. The Institutional Review Board of the hospital approved the study, and informed consent was obtained for all participants.
Data Collection
All patients who agreed to participate were administered the standard questions composed of the NDSD screening protocol. The Harvard Department of Psychiatry's National Depression Screening Day Scale (HANDS),6 which assesses depressive symptoms, is summarized in a separate article.7
The Mood Disorder Questionnaire (MDQ)
The MDQ2,3 consists of 3 sections patterned after the DSM-IV8 symptoms for a manic episode and was created specifically to allow rapid screening for bipolar disorder across a range of settings. For section 1, respondents indicated whether they had ever had a period of time when they were not their usual selves and had experienced any of 13 symptoms. Section 2 asked respondents to record whether the symptoms checked in section 1 occurred during the same time period. Section 3 asked respondents to rate their degree of impairment: 3 = serious problem, 2 = moderate problem, 1 = minor problem, and 0 = no problem. A patient was considered at risk for bipolar disorder if the total score for section 1 was 7 or greater, the answer for section 2 was “Yes,” and the rating for section 3 was “moderate” or “serious.” Past studies2,3 have found the MDQ to be reliable (α = 0.84) and to possess good construct validity as evidenced by moderate to strong correlations ranging from 0.36 to 0.63 with other bipolar symptom tools. The sensitivity and specificity of the MDQ for detecting DSM-IV–diagnosed bipolar disorder are 73% and 90%, respectively, in a clinical population, and 28% and 97%, respectively, in a community population.2,3 An alternate scoring method that uses only the section 1 symptom criteria has been suggested since it has been shown to reduce false-negative screens in a mental health sample.9
Psychiatric history
Patients indicated whether they had ever been treated for depression, bipolar disorder, generalized anxiety disorder, or posttraumatic stress disorder. For the purposes of examining trends, we created a dichotomous variable that represented treatment for any psychiatric condition (0 = no psychiatric treatment, 1 = treatment for 1 or more psychiatric conditions). One question assessed presence of a previous suicide attempt.
Substance abuse history
Patients indicated whether they had ever been treated for alcohol or drug abuse.
Medical history
Patients indicated whether they had ever been treated for cancer, chronic pain, diabetes, heart disease, stroke, human immunodeficiency virus, seizure disorder, thyroid disorder, or asthma. We created a dichotomous variable that represented presence of any chronic medical condition (0 = no medical condition, 1 = at least 1 medical condition).
Data Analyses
All statistical analyses were performed using SPSS 11.5 (SPSS Inc., Chicago, Ill.). Descriptive statistics are presented. Due to low statistical power, we did not conduct statistical tests to examine differences in prevalence based on other variables. However, we did calculate the proportions of positive screens broken down by the sample's characteristics for the purpose of hypothesis generation.
RESULTS
Of the 665 adult patients treated in the ED during the study period, 556 presented during the hours of enrollment, and 379 were recorded on the study log. Fifty-seven of those recorded on the study log were discharged before the research assistant could approach them, while 110 were approached but did not meet inclusion/exclusion criteria. Of the 212 patients that were approached and eligible, 30 refused to participate, leaving 182 (33% of total presenting during hours of enrollment; 86% of eligible patients approached) to be enrolled. Data from “missed” or excluded patients were not collected due to the anonymous nature of the study, making a comparison of the enrolled versus nonenrolled groups impossible. However, the demographic characteristics were largely consistent with our ED as a whole. The internal consistency reliability of the 13 symptoms comprising section 1 on the MDQ was acceptable (α = 0.69).
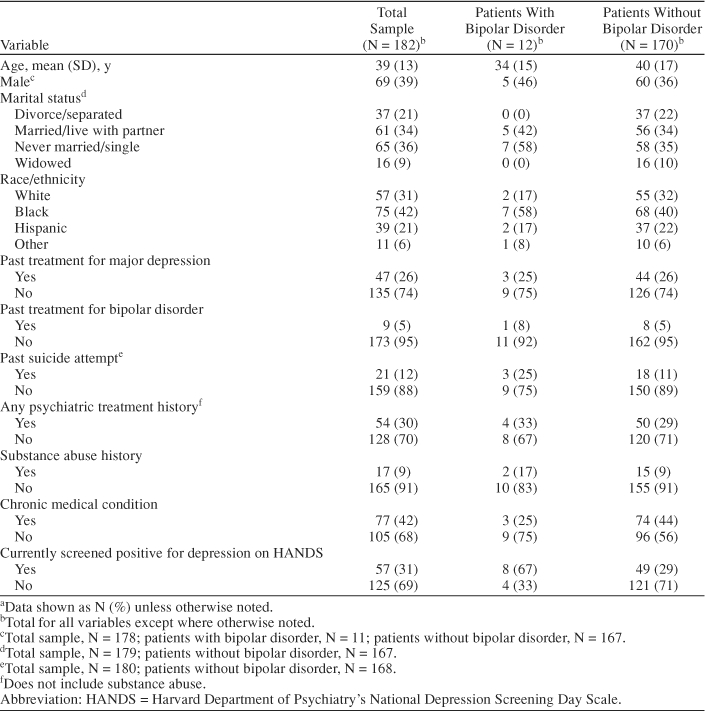
The sample's point prevalence of a positive screen for bipolar disorder using the standard cut-off criteria was 12 of 182, or 6.6% (95% CI = 3.5% to 11.2%). When the alternate criterion using only a symptom count of greater than 7 was used, 29 of 182 screened positive, or 15.9% (95% CI = 10.9% to 22.1%). Table 1 provides additional detail on the descriptive statistics.
Table 1.
Characteristics of Adult Patients With and Without Bipolar Disorder in an Emergency Departmenta
DISCUSSION
Nearly 7% of our sample screened positive for bipolar disorder. When the criteria were relaxed and only the symptom threshold was used, as suggested by Miller et al.,9 nearly 16% screened positive. Regardless of which figure is considered, the prevalence was markedly higher than the 1.3% estimate for 12-month prevalence of DSM-IV–diagnosed bipolar disorder in a nationally representative community cohort.10 While it is certainly possible that the MDQ yielded many false positives, the psychometrics of the instrument have been established in several studies, and it has been shown to yield a relatively low false-positive rate.2,3,9 Even if the MDQ yielded a false-positive rate of 50%, the prevalence of bipolar disorder in our sample would remain more than double that of community rates (3.3% vs. 1.3%, respectively). Nevertheless, further studies validating the MDQ against the gold standard structured diagnostic interview within an ED sample are needed, especially considering the marginally acceptable internal consistency reliability coefficient (α = 0.69) and the variable test performance characteristics reported between clinical and community populations.2,3,9
There are several strengths associated with this study. We could identify no other published studies that prospectively screened for bipolar disorder in the ED setting using a validated screening instrument. Our preliminary findings suggest there may be a tremendous reservoir of patients with bipolar symptoms who are being treated in the ED setting. The survey was completely anonymous and carried out via paper and pencil, which allowed patients to feel comfortable disclosing their symptoms and increased our confidence that patients were not minimizing their symptoms for socially desirable reasons. Finally, although we did not have sufficient power for traditional statistical analyses, the trends we observed were noteworthy. For example, 8 (6%) of 120 patients reporting that they had not had a previous psychiatric treatment history screened positive for bipolar disorder, which was similar to the rate for those with a psychiatric treatment history (7%). If these trends are validated, they suggest that many patients reporting bipolar symptoms that are impairing their lives are not receiving psychiatric care. Since the ED setting acts as the safety net for many patients who have no other resources, like the economically disadvantaged, immigrants, and the uninsured, it may be a particularly important setting in which to establish identification and referral systems.
Our study had several potential limitations. First, only 12 patients screened positive for bipolar disorder, which translated into a large percentage (6.6%) because the sample size was so small. This proportion may, therefore, be misleading and awaits larger studies for confirmation. Second, we were able to collect data on only 33% of the adult patients who visited the ED during the time of the study. Most were simply missed because of high volume. Additionally, of those that were recorded on the study log (N = 379), 110 (29%) were excluded because they were severely ill, acutely distressed, or cognitively disabled patients. The most likely effect of the exclusion criteria was to yield an underestimate of bipolar disorder (i.e., acutely ill bipolar disorder patients presenting with psychosis or agitation probably would not have been enrolled). Third, the ED was located in a northeastern, urban city, which may not represent the rest of the country. Fourth, while the reliability, validity, and operating characteristics of the MDQ have been established in community and mental health samples, these have not been validated in ED samples.
CONCLUSION
Nearly 7% of ED patients screened positive for bipolar disorder, which is considerably higher than community estimates. Further prospective research on bipolar disorders among ED patients is needed in order to further define the scope of the problem and to inform the development of appropriate screening, assessment, and intervention programs.
Footnotes
Dr. Boudreaux is supported by the National Institutes of Health/National Institute on Drug Abuse grant #DA-16698-01 and a UMDNJ Foundation seed grant.
The authors report no additional financial or other relationships relevant to the subject of this article.
REFERENCES
- Kleinman L, Lowin A, and Flood E. et al. Costs of bipolar disorder. Pharmacoeconomics. 2003 21:601–622. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RMA, Holzer C, and Calabrese JR. et al. Validity of the Mood Disorder Questionnaire: a general population study. Am J Psychiatry. 2003 160:178–180. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RMA, Williams JBW, and Spitzer RL. et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000 157:1873–1875. [DOI] [PubMed] [Google Scholar]
- McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2001 emergency department summary. Adv Data. 2003;335:1–29. [PubMed] [Google Scholar]
- Hazlett SB, McCarthy ML, and Londner MS. et al. Epidemiology of adult psychiatric visits to US emergency departments. Acad Emerg Med. 2004 11:193–195. [PubMed] [Google Scholar]
- Baer L, Jacobs DG, and Meszler-Reizes J. et al. Development of a brief screening instrument: the HANDS. Psychother Psychosom. 2000 69:35–41. [DOI] [PubMed] [Google Scholar]
- Boudreaux ED, Cagande C, and Kilgannon H. et al. A prospective study of depression among adults in an urban emergency department. Prim Care Companion J Clin Psychiatry. 2006 8:66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association. 1994 [Google Scholar]
- Miller CJ, Klugman J, and Berv DA. et al. Sensitivity and specificity of the Mood Disorder Questionnaire for detecting bipolar disorder. J Affect Disord. 2004 81:167–171. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, and Zhao S. et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Study. Arch Gen Psychiatry. 1994 51:8–19. [DOI] [PubMed] [Google Scholar]


