Abstract
Pathological gambling (PG) is a prevalent and highly disabling impulse-control disorder. Two dominant phenomenological models for PG have been presented in the literature. According to one model, PG is included as an obsessive-compulsive spectrum disorder, while according to the second model, PG represents a form of nonpharmacologic addiction. In this article, we present an expanded conceptualization of the phenomenology of PG. On the basis of our clinical research experience and a review of data in the field, we propose 3 subtypes of pathological gamblers: the “impulsive” subtype, the “obsessive-compulsive” subtype, and the “addictive” subtype. We also review the current pharmacologic and nonpharmacologic treatment strategies for PG. A further aim of this article is to encourage awareness of the importance of improved screening procedures for the early detection of PG.
Pathological gambling (PG) is classified in the DSM-IV as a disorder of impulse control with the essential feature being recurrent and maladaptive gambling behavior.1 In the International Classification of Diseases of the World Health Organization, PG is coded under the heading of Habit and Impulse Disorders together with kleptomania, pyromania, and trichotillomania.2 Impulse-control disorders are characterized by an overwhelming urge to perform a harmful act. Pathological gambling is a chronic, progressive, male-dominated disorder that has a prevalence of 1.0% to 3.4% among U.S. adults.3 Individuals with PG engage in persistent and recurrent maladaptive patterns of gambling behavior. Typically, the patient's life becomes dominated by gambling behavior, leading to overwhelming financial burdens, an inability to maintain a career, and the eventual disintegration of family relationships. The enormous personal and social consequences of this disorder include a high rate of suicide attempts, increased rates of legal problems, and criminal behavior.4 Recent data have shown that PG that is comorbid with substance abuse confers an increased risk of health problems on the substance abuser5,6 and is associated with increased treatment resistance of the substance abuse.7
Epidemiologic studies have suggested that PG may be a familial disorder with a genetic component. Results of a twin study by Shah et al.8 showed evidence of genetic transmission in men. Furthermore, Black and colleagues,9 in a controlled study, showed that the first-degree relatives of pathological gamblers had significantly increased rates of PG as well as significantly increased rates of substance abuse. Data from this family study also suggested that PG coaggregates with antisocial personality disorder.9
Pathological gambling appears to be associated with other psychiatric disorders, most notably mood disorders, anxiety disorders, personality disorders, other impulse-control disorders, and alcohol and other substance abuse and dependence.10–12 Given the prominence of psychiatric comorbidity in PG, the current standard of care is to modify the choice of pharmacologic treatment according to the comorbid psychiatric conditions.13,14 We note that PG has been demonstrated to be highly prevalent in a cohort of hospitalized psychiatric patients,15 suggesting an association with severe psychiatric disorders. Interestingly, recent epidemiologic data have confirmed clinical observations that pathological gamblers do not tend to seek out treatment for gambling behavior.16 Indeed, most PG patients are referred for psychiatric treatment due to a comorbid psychiatric or somatic disorder,5 and so the clinician must actively screen for the presence of pathological gambling behavior.
Hollander and Wong17 suggested that impulsive disorders such as PG are associated with strong compulsive and impulsive features, and, hence, PG can be viewed as an “impulsive” subtype of the “obsessive-compulsive (OC) spectrum” disorders.
Recently, investigators have looked at the role of impulsivity in both disorders of substance abuse and PG. Chambers and Potenza18 propose that the common trait of impulsivity might underlie PG, commonly comorbid psychiatric disorders, and related aspects of adolescent behavior. They postulate that immaturity of the frontal cortical and subcortical monoaminergic systems during adolescent neurodevelopment is a predisposing factor for adolescent impulsive behavior. It is of interest that lesions in the ventromedial prefrontal cortex can result in faulty decision-making based on the need for immediate as opposed to delayed gratification.19 Several theoretical models of addiction have suggested that addiction might be related to abnormality in the activity of the prefrontal cortex system that is necessary for inhibiting the immediate reward and excitement seeking behavior.20,21
Over the past 7 years, we have conducted a number of clinical research protocols in our cohort of Israeli pathological gamblers. Our protocols included case-controlled family studies,22,23 blind-rater medication studies,24–26 neurocognitive studies (reference 27 and S. Kertzman, M.D.; K.L.; A. Aizer, M.D.; et al., unpublished data), and gender comparison studies.28 Based on our research experience, we have seen that PG tends to be a heterogeneous disorder in which patients differ with respect to type and intensity of gambling behavior, psychiatric comorbidity, family history, age at onset, and gender. Based on the results of our clinical research experience and a review of data in the field (as discussed above), we propose that pathological gamblers may be classified according to 1 of 3 subtypes: (1) the “impulsive” subtype, (2) the “obsessive-compulsive” (OC) subtype, and (3) the “addictive” subtype. We will discuss these subtypes in terms of demographic characteristics, psychiatric comorbidity, and possible etiopathology.
THEORETICAL SUBTYPES
First, we propose that the impulsive subtype of PG comprises primarily young adult men who have high levels of risk-taking behavior and lack the ability to plan ahead. Those with impulsive PG tend have an increased severity of symptoms compared to other subtypes and tend to lose large sums of money at one sitting. Commonly comorbid psychiatric conditions include attention deficit disorder (ADD) and alcohol and other substance abuse and dependence, as well as other impulse-control disorders.29 First-degree relatives tend to have high rates of gambling and addiction problems.30 Neuropsychological studies of subjects with PG31,32 have demonstrated that these individuals have deficits in the frontal lobe/reward system, and we hypothesize that impairment of executive function may play an important role in the impulsive subtype of pathological gambler. These patients may respond best to medications such as bupropion33,34 or mood stabilizers,34 which are thought to target impulsive behavior.
In the OC subtype of PG, we propose that there is a preponderance of female patients who tend to have the onset of symptoms in mid-life. These patients may develop pathological gambling behavior in response to a perceived psychological trauma such as divorce or the “empty nest syndrome.” We note that preliminary studies show that there may be gender differences among pathological gamblers. For example, a recent comparison study between male and female gamblers showed higher rates of depression and more maladaptive coping styles in the female versus the male PG patients.28 Similarly, in a gender comparison study, Blanco et al.35 showed that subclinical gambling behavior may be more common in women than in men and is associated with increased rates of lifetime mood and anxiety disorders. Blanco et al. also demonstrated that women reported the onset of gambling behavior as a way to cope with depressed mood. In a gender comparison study of adolescent gamblers, Desai et al.36 reported that girls had significantly higher rates of dysphoria and depression. Commonly comorbid psychiatric disorders for the OC subtype of PG may include affective and anxiety disorders.17 According to Blaszczynski,37 PG and obsessive-compulsive disorder tend to overlap in a treatment population, and heavy gamblers reported more hoarding symptoms and compulsive buying than light gamblers. In our experience, the primarily female pathological gamblers of the OC subtype tend to prefer slot machines and lottery and scratch tickets, while male patients tend to prefer playing cards, blackjack, poker, and sporting bets. Given the accumulated evidence regarding the high comorbidity of depressive and anxiety disorders in female gamblers,22,23,28 we suggest that these patients may be preferentially responsive to antidepressive agents such as the selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs). Psychotherapy addressing stress resolution and coping mechanisms may be particularly helpful in the group of women gamblers.
It is our opinion that the addictive PG subtype represents the largest subgroup of pathological gamblers and is associated with a moderate severity of pathological gambling. Like the obsessive-compulsive subtype, this group tends to gamble small amounts of money at a time in a repetitive and compulsive fashion. The addictive subtype is distinguished from the OC subtype by a larger ratio of male patients and higher rates of comorbid alcohol abuse and dependence.22 The association between PG and substance abuse in males is well documented in the literature.38,39 In a comorbidity study of male and female gamblers,28 our group demonstrated that male patients suffered from high rates of comorbid substance abuse and alcohol abuse. In contrast, the women in our sample had higher rates of obsessive-compulsive disorder, panic disorder, and generalized anxiety disorder. We note that comorbid substance abuse was also seen in the women pathological gamblers, but at lower rates compared with the men's cohort. Comorbid eating disorders were seen in our female patients but not in their male counterparts. Notably, comorbid depression was seen in both groups but was higher in the women. In a cross-sectional study, Goudriaan et al.40 showed that pathological gamblers and abstinent alcoholics had similar patterns of deficits in executive functioning (such as impaired decision-making and feedback processing) and suggested a common neurocognitive etiology. We propose that the addictive subtype pathological gambler may respond well to opioid antagonists that target the frontal lobe reward system.
TREATMENT STRATEGIES
Psychological Interventions
Cognitive-behavioral therapy (CBT) currently represents the dominant psychological approach in the treatment of PG. Several outcome studies have shown CBT to be effective in the treatment of PG.41–43 Models of CBT for PG have been drawn, in part, from experience in the field of addiction. Multiple studies have supported the theory that cognitive distortions or irrational beliefs pertaining to addictive behavior may operate at automatic levels.44 Examples of cognitive distortion in the field of PG include magnification of gambling skills, superstitious beliefs, and selective memory,45 as well as gambling-related cognitions such as “I feel lucky today” or “I know I can win.”7 The CBT model most often used for impulse-control disorders consists of 4 components: (1) cognitive restructuring to correct irrational and dysfunctional beliefs that precede impulsive behavior, (2) problem-solving skills aimed at generating alternative responses to stress, (3) social skills training, and (4) relapse prevention in which the patient is taught to identify and avoid high-risk situations.46
Dynamic and psychoanalytic psychotherapy may also have a role in the treatment of PG. A recent study by Kausch et al.47 showed that pathological gamblers have high rates of childhood trauma (including sexual and physical trauma). Psychoanalytic theories provide insight into the sadomasochistic personality functioning and deeper object relational issues that may lie behind the gambling behavior.48 Alternatively, recent data regarding neurocognitive deficits in pathological gamblers show that neuropsychological treatments could target deficits in executive function.40
Pharmacologic Interventions
Emerging data in the field show that PG may be responsive to a range of psychopharmacologic agents including SSRIs, mood stabilizers, opioid antagonists, and the psychostimulant bupropion. We note that there is also preliminary evidence that combination pharmacotherapy has a role in the treatment of impulse-control disorders (S. Kertzman, M.D.; K.L.; A. Aizer, M.D.; et al., unpublished data).
To date, there have been 5 double-blind trials of SSRIs for the treatment of PG. Hollander et al.,49 in a 16-week double-blind, crossover study, reported the superior effect of fluvoxamine (40.6% improvement on the pathological gambling modification of the Clinical Global Impressions scale [PG-CGI]) compared with placebo (16.6%). However, in a 6-month, double-blind, placebo-controlled study (N = 34), Blanco et al.50 found that fluvoxamine treatment did not result in statistically significant improvement as measured by reduction in money and time spent gambling. Kim et al.,51 in an 8-week, double-blind trial (N = 41), found a significantly greater improvement (using patient-rated PG-CGI and clinician-rated PG-CGI) in the paroxetine group as compared with placebo. Grant et al.52 conducted a 16-week, multicenter, randomized, controlled study of paroxetine versus placebo in the treatment of PG (N = 76) and found no significant statistical superiority of paroxetine compared to placebo. Similarly, in a double-blind study, Saiz-Ruiz et al.53 found that sertraline was not superior to placebo for the treatment of PG. Grant and Potenza,54 in an open-label pilot study, reported that esci-talopram treatment was associated with improvement in gambling and anxiety symptoms in patients with comorbid PG and anxiety. Pallanti et al.,55 in a prospective, open-label trial, demonstrated that nefazadone, a novel SSRI that is a specific 5-HT2 antagonist, was effective in reducing gambling urges and gambling behavior. This is of interest because there is evidence that 5-HT2 receptors may play a role in disorders of impulsive aggression.56 While showing mixed success overall, previous SSRI studies have had limitations including low numbers of women subjects, high dropout rates, and variability in the magnitude of the placebo response observed in different trials.
Pallanti et al.34 describe a connection between the clinical features of PG and bipolar disorder. They discuss characteristics common to both disorders, such as impulsive risk-taking behavior, mood swings, poor judgment, and grandiose thinking. In support of this theory, they present findings of a single-blind, 14-week trial (N = 42) that demonstrate the efficacy of lithium carbonate and valproate monotherapy in the treatment of PG. Hollander et al.,57 in a double-blind study, showed that PG patients with comorbid bipolar spectrum disorder had a positive response to lithium in terms of gambling severity and impulsivity scales.
Topiramate is a newer anticonvulsant that is effective in the treatment of grand mal and partial seizures in epilepsy in children and adults and also effective in the treatment of Lennox-Gastaut disorder. The mechanism of action of to-piramate includes both GABAergic and antiglutamatergic mechanisms. In a preliminary study, our group reported the possible usefulness of topiramate for the treatment of PG.24
Naltrexone, an opioid antagonist that works on the reward system, has been shown to be effective for the treatment of alcohol and substance abuse58,59 and recently has been studied in the treatment of impulse-control disorders. Kim and colleagues,60 in a double-blind study (N = 83), showed that naltrexone treatment significantly reduced the average intensity of gambling urges, gambling thoughts, and gambling behavior. In another double-blind study, Grant et al.,61 in a multicenter investigation, showed the efficacy of low-dose (25 mg/day) nalmefene in the treatment of PG. We note that treatment with naltrexone may be limited by the risk of hepatotoxicity, especially at higher doses. Kim et al.62 designed a study to address the issue of hepatotoxicity and reported that prolonged use of high-dose oral naltrexone (150 mg/day) appears to be safe in otherwise healthy patients if over-the-counter analgesic use is restricted.
Bupropion sustained release is a selective reuptake inhibitor of dopamine and norepinephrine and has been found to reduce nicotine withdrawal symptoms and the urge to smoke.63 Bupropion has a chemical structure similar to the psychostimulants and indirectly stimulates the acetylcholine, hydroxytryptamine, and γ-aminobutyric acid receptors, as well as endorphins. Black33 postulated that psychostimulants may be useful in the treatment of PG because of the overlap with ADD in terms of comorbidity, attentional deficits, and impulsivity. Black designed a small pilot study to test this hypothesis and found that bupropion treatment was associated with an increased ability to resist gambling urges. Our group reported the effectiveness of bupropion in a randomized drug comparison study (bupropion vs. naltrexone) and in a group of treatment-resistant pathological gamblers.25
CONCLUSIONS
Our experience supports current evidence that PG may represent a heterogeneous disorder with different subtypes. Studies of psychiatric comorbidity, family studies, demographic information, and psychological profiles (i.e., attentional deficits and impulsivity) are useful in building models of PG subtypes. An increased understanding of patient subtypes can potentially allow clinicians to use specific therapeutic strategies for specific subtypes of patients. Consistent with recommendations by Dell'Osso et al.,14 we propose that subtyping of pathological gamblers may have implications for pharmacologic treatment recommendations. For example, impulsive subtype patients may respond best to bupropion or mood stabilizers, which appear to target impulsivity. The obsessive-compulsive subtype may respond best to SSRIs or SNRIs, which may target related depressive and anxious symptoms as well as compulsive behavior. In addictive subtype patients, it would be logical to use opioid antagonists such as naltrexone or nalmefene as first-line agents.
Building a model of patient subtypes in PG may also have prognostic implications. Traditionally, PG has been thought of as a chronic disorder, but a recent epidemiologic study showed that the clinical course may be characterized as one of natural recovery.16 We propose that individuals with the impulsive and OC subtypes may be more likely to have remission of symptoms because these subtypes may be associated with lower rates of comorbid substance abuse. It is well accepted that comorbid substance abuse and PG leads to increased treatment resistance for both conditions, and therefore the addictive subtype pathological gambler will likely have a more chronic course if not treated aggressively.
We believe that a knowledge of risk factors for PG and knowledge of commonly comorbid psychiatric conditions may enable the psychiatrist to more effectively screen for this disorder. For example, given the high comorbidity between PG and alcohol abuse, it would be reasonable to screen all alcoholic patients for the presence of comorbid gambling behavior. Other potential risk factors for PG include living in a “disadvantaged” neighborhood and living in close proximity to gambling opportunities.64 Clearly, early identification and treatment of PG are important in order to prevent the potentially devastating social, occupational, financial, medical, and legal consequences of this disorder. We suggest that future studies address the question of how to serve a broader patient population, and we hope that future treatment research can lead to expert consensus and treatment guidelines for pathological gambling.
Drug names: bupropion (Wellbutrin, Zyban, and others), escitalopram (Lexapro and others), lithium (Eskalith, Lithobid, and others), nalmefene (Revex), naltrexone (ReVia and others), paroxetine (Paxil, Pexeva, and others), sertraline (Zoloft and others), topiramate (Topamax and others).
Disclosure of off-label usage: The authors have determined that, to the best of their knowledge, bupropion, escitalopram, lithium, nalmefene, naltrexone, paroxetine, sertraline, topiramate, fluvoxamine, and valproate are not approved by the U.S. Food and Drug Administration for the treatment of pathological gambling.
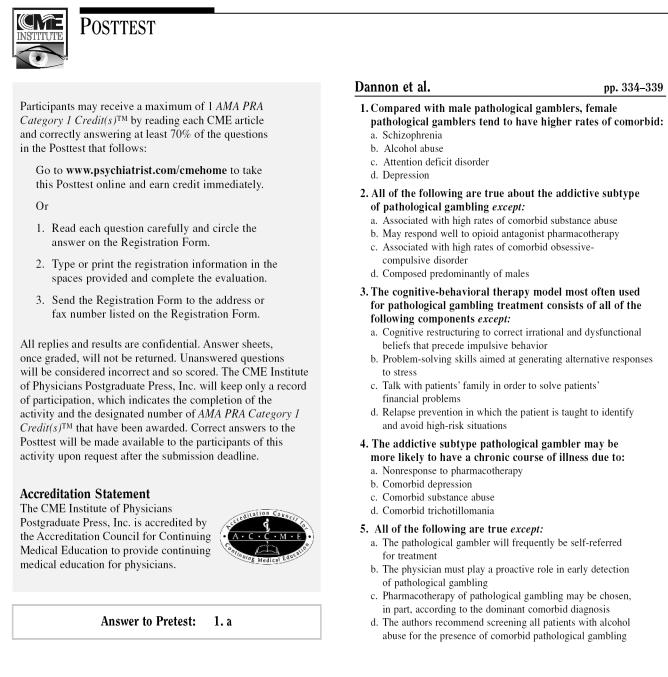
Instructions and Posttest
Registration Form
Footnotes
In the spirit of full disclosure and in compliance with all ACCME Essential Areas and Policies, the faculty for this CME article were asked to complete a statement regarding all relevant financial relationships between themselves or their spouse/partner and any commercial interest (i.e., any proprietary entity producing health care goods or services consumed by, or used on, patients) occurring within at least 12 months prior to joining this activity. The CME Institute has resolved any conflicts of interest that were identified. The disclosures are as follows: Drs. Dannon, Lowengrub, Gonopolski, Musin, and Kotler have no personal affiliations or financial relationships with any proprietary entity producing health care goods or services consumed by, or used on, patients to disclose relative to the article.
REFERENCES
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association. 1994 [Google Scholar]
- World Health Organization. International Classification of Diseases, Tenth Revision. Geneva, Switzerland: World Health Organization. 1992 [Google Scholar]
- Shaffer HJ, Hall MN, Vander Bilt J. Estimating the prevalence of disordered gambling behavior in the United States and Canada: a research synthesis. Am J Public Health. 1999;89:1369–1376. doi: 10.2105/ajph.89.9.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander E, Buchalter AJ, DeCaria CM. Pathological gambling. Psychiatr Clin North Am. 2000;23:629–642. doi: 10.1016/s0193-953x(05)70185-4. [DOI] [PubMed] [Google Scholar]
- Morasco BJ, Vom Eigen KA, Petry NM. Severity of gambling is associated with physical and emotional health in urban primary care patients. Gen Hosp Psychiatry. 2006;28:94–100. doi: 10.1016/j.genhosppsych.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Weinstock J, Blanco C, Petry NM. Health correlates of pathological gambling in a methadone maintenance clinic. Exp Clin Psychopharmacol. 2006;14:87–93. doi: 10.1037/1064-1297.14.1.87. [DOI] [PubMed] [Google Scholar]
- Milton S, Crino R, and Hunt C. et al. The effect of compliance-improving interventions on the cognitive-behavioural treatment of pathological gambling. J Gambl Stud. 2002 18:207–229. [DOI] [PubMed] [Google Scholar]
- Shah KR, Eisen SA, and Xian H. et al. Genetic studies of pathological gambling: a review of methodology and analyses of data from the Vietnam era twin registry. J Gambl Stud. 2005 21:179–203. [DOI] [PubMed] [Google Scholar]
- Black DW, Monahan PO, and Temkit M. et al. A family study of pathological gambling. Psychiatry Res. 2006 141:295–303. [DOI] [PubMed] [Google Scholar]
- Blanco C, Moreyra P, and Nunes EV. et al. Pathological gambling: addiction or compulsion? Semin Clin Neuropsychiatry. 2001 6:167–176. [DOI] [PubMed] [Google Scholar]
- Grant JE, Kim SW. Comorbidity of impulse control disorders in pathological gamblers. Acta Psychiatr Scand. 2003;108:203–207. doi: 10.1034/j.1600-0447.2003.00162.x. [DOI] [PubMed] [Google Scholar]
- Sood ED, Pallanti S, Hollander E. Diagnosis and treatment of pathologic gambling. Curr Psychiatry Rep. 2003;5:9–15. doi: 10.1007/s11920-003-0003-7. [DOI] [PubMed] [Google Scholar]
- Dell'Osso B, Hollander E. The impact of comorbidity on the management of pathological gambling. CNS Spectr. 2005;10:619–621. doi: 10.1017/s109285290001957x. [DOI] [PubMed] [Google Scholar]
- Dell'Osso B, Allen A, Hollander E. Comorbidity issues in the pharmacological treatment of pathological gambling: a critical review. Clin Pract Epidemol Ment Health. 2005;1:21. doi: 10.1186/1745-0179-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JE, Levine L, and Kim D. et al. Impulse control disorders in adult psychiatric inpatients. Am J Psychiatry. 2005 162:2184–2188. [DOI] [PubMed] [Google Scholar]
- Slutske WS. Natural recovery and treatment-seeking in pathological gambling: results of two US national surveys. Am J Psychiatry. 2006;163:297–302. doi: 10.1176/appi.ajp.163.2.297. [DOI] [PubMed] [Google Scholar]
- Hollander E, Wong CM. Obsessive-compulsive spectrum disorders. J Clin Psychiatry. 1995 56suppl 4. 3–6.discussion 53–55. [PubMed] [Google Scholar]
- Chambers RA, Potenza MN. Neurodevelopment, impulsivity, and adolescent gambling. J Gambl Stud. 2003;19:53–84. doi: 10.1023/a:1021275130071. [DOI] [PubMed] [Google Scholar]
- Bechara A. Risky business: emotion, decision-making, and addiction. J Gambl Stud. 2003;19:23–51. doi: 10.1023/a:1021223113233. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H. Decision-making and addiction, pt 1: impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia. 2002;40:1675–1689. doi: 10.1016/s0028-3932(02)00015-5. [DOI] [PubMed] [Google Scholar]
- Bechara A, Dolan S, Hindes A. Decision-making and addiction, pt 2: myopia for the future or hypersensitivity to reward? Neuropsychologia. 2002;40:1690–1705. doi: 10.1016/s0028-3932(02)00016-7. [DOI] [PubMed] [Google Scholar]
- Dannon PN, Lowengrub K, and Sasson M. et al. Comorbid psychiatric diagnoses in kleptomania and pathological gambling: a preliminary comparison study. Eur Psychiatry. 2004 19:299–302. [DOI] [PubMed] [Google Scholar]
- Dannon PN, Lowengrub K, and Aizer A. et al. Pathological gambling: comorbid psychiatric diagnoses in patients and their families. Isr J Psychiatry Relat Sci. 2006 43:88–92. [PubMed] [Google Scholar]
- Dannon PN, Lowengrub K, and Gonopolski Y. et al. Topiramate versus fluvoxamine in the treatment of pathological gambling: a randomized, blind-rater comparison study. Clin Neuropharmacol. 2005 28:6–10. [DOI] [PubMed] [Google Scholar]
- Dannon PN, Lowengrub K, and Musin E. et al. Sustained-release bupropion versus naltrexone in the treatment of pathological gambling: a preliminary blind-rater study. J Clin Psychopharmacol. 2005 25:593–596. [DOI] [PubMed] [Google Scholar]
- Dannon PN, Lowengrub K, and Musin E. et al. Sustained release bupropion in the treatment of SSRI nonresponder pathological gamblers: pilot study and review of the literature. Therapy. 2005 2:753–759. [Google Scholar]
- Kertzman S, Lowengrub K, and Aizer A. et al. Stroop performance in pathological gamblers. Psychiatry Res. 2006 142:1–10. [DOI] [PubMed] [Google Scholar]
- Dannon PN, Lowengrub K, and Shalgi B. et al. Dual psychiatric diagnoses and substance abuse in pathological gamblers: a preliminary gender comparison study. J Addict Dis. 2006 25:49–54. [DOI] [PubMed] [Google Scholar]
- Lynch WJ, Maciejewski PK, Potenza MN. Psychiatric correlates of gambling in adolescents and young adults grouped by age at gambling onset. Arch Gen Psychiatry. 2004;61:1116–1122. doi: 10.1001/archpsyc.61.11.1116. [DOI] [PubMed] [Google Scholar]
- Vachon J, Vitaro F, and Wanner B. et al. Adolescent gambling: relationships with parent gambling and parenting practices. Psychol Addict Behav. 2004 18:398–401. [DOI] [PubMed] [Google Scholar]
- Steel Z, Blaszczynski A. Impulsivity, personality disorders and pathological gambling severity. Addiction. 1998;93:895–905. doi: 10.1046/j.1360-0443.1998.93689511.x. [DOI] [PubMed] [Google Scholar]
- Spinella M. Evolutionary mismatch, neural reward circuits, and pathological gambling. Int J Neurosci. 2003;113:503–512. doi: 10.1080/00207450390162254. [DOI] [PubMed] [Google Scholar]
- Black DW. An open-label trial of bupropion in the treatment of pathological gambling. J Clin Psychopharmacol. 2004;24:108–110. doi: 10.1097/01.jcp.0000114844.58996.4a. [DOI] [PubMed] [Google Scholar]
- Pallanti S, Quercioli L, and Sood E. et al. Lithium and valproate treatment of pathological gambling: a randomized single-blind study. J Clin Psychiatry. 2002 63:559–564. [DOI] [PubMed] [Google Scholar]
- Blanco C, Hasin DS, and Petry N. et al. Sex differences in subclinical and DSM-IV pathological gambling: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006 36:943–953. [DOI] [PubMed] [Google Scholar]
- Desai RA, Maciejewski PK, and Pantalon MV. et al. Gender differences in adolescent gambling. Ann Clin Psychiatry. 2005 17:249–258. [DOI] [PubMed] [Google Scholar]
- Blaszczynski A. Pathological gambling and obsessive-compulsive spectrum disorders. Psychol Rep. 1999;84:107–113. doi: 10.2466/pr0.1999.84.1.107. [DOI] [PubMed] [Google Scholar]
- Potenza MN, Fiellin DA, and Heninger GR. et al. Gambling: an addictive behavior with health and primary care implications. J Gen Intern Med. 2002 17:721–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM. How treatments for pathological gambling can be informed by treatments for substance use disorders. Exp Clin Psychopharmacol. 2002;10:184–192. doi: 10.1037//1064-1297.10.3.184. [DOI] [PubMed] [Google Scholar]
- Goudriaan AE, Oosterlaan J, and de Beurs E. et al. Neurocognitive functions in pathological gambling: a comparison with alcohol dependence, Tourette syndrome and normal controls. Addiction. 2006 101:534–547. [DOI] [PubMed] [Google Scholar]
- Sylvain C, Ladouceur R, Boisvert JM. Cognitive and behavioral treatment of pathological gambling: a controlled study. J Consult Clin Psychol. 1997;65:727–732. doi: 10.1037//0022-006x.65.5.727. [DOI] [PubMed] [Google Scholar]
- Echeburua E, Baez C, Fernandez-Montalvo J. Comparative effectiveness of three therapeutic modalities in the psychological treatment of pathological gambling. Behav Cog Psychother. 1996;24:51–72. [Google Scholar]
- Echeburua E, Fernandez-Montalvo J, Baez C. Prevention in the treatment of slot-machine pathological gambling: long-term outcome. Behav Ther. 2000;31:351–364. [Google Scholar]
- McCusker CG. Cognitive biases and addiction: an evolution in theory and method. Addiction. 2001;96:47–56. doi: 10.1046/j.1360-0443.2001.961474.x. [DOI] [PubMed] [Google Scholar]
- Toneatto T. Cognitive psychopathology of problem gambling. Subst Use Misuse. 1999;34:1593–1604. doi: 10.3109/10826089909039417. [DOI] [PubMed] [Google Scholar]
- Petry NM, Roll JM. A behavioral approach to understanding and treating pathological gambling. Semin Clin Neuropsychiatry. 2001;6:177–183. doi: 10.1053/scnp.2001.22920. [DOI] [PubMed] [Google Scholar]
- Kausch O, Rugle L, Rowland DY. Lifetime histories of trauma among pathological gamblers. Am J Addict. 2006;15:35–43. doi: 10.1080/10550490500419045. [DOI] [PubMed] [Google Scholar]
- Waska R. Addictions and the quest to control the object. Am J Psychoanal. 2006;66:43–62. doi: 10.1007/s11231-005-9002-2. [DOI] [PubMed] [Google Scholar]
- Hollander E, DeCaria CM, and Finkell JN. et al. A randomized double-blind fluvoxamine/placebo crossover trial in pathologic gambling. Biol Psychiatry. 2000 47:813–817. [DOI] [PubMed] [Google Scholar]
- Blanco C, Petkova E, and Ibanez A. et al. A pilot placebo-controlled study of fluvoxamine for pathological gambling. Ann Clin Psychiatry. 2002 14:9–15. [DOI] [PubMed] [Google Scholar]
- Kim SW, Grant JE, and Adson DE. et al. A double-blind, placebo-controlled study of the efficacy and safety of paroxetine in the treatment of pathological gambling. J Clin Psychiatry. 2002 63:501–507. [DOI] [PubMed] [Google Scholar]
- Grant JE, Kim SW, and Potenza MN. et al. Paroxetine treatment of pathological gambling: a multi-centre randomized controlled trial. Int Clin Psychopharmacol. 2003 18:243–249. [DOI] [PubMed] [Google Scholar]
- Saiz-Ruiz J, Blanco C, and Ibanez A. et al. Sertraline treatment of pathological gambling: a pilot study. J Clin Psychiatry. 2005 66:28–33. [DOI] [PubMed] [Google Scholar]
- Grant JE, Potenza MN. Escitalopram treatment of pathological gambling with co-occurring anxiety: an open-label pilot study with double-blind discontinuation. Int Clin Psychopharmacol. 2006;21:203–209. doi: 10.1097/00004850-200607000-00002. [DOI] [PubMed] [Google Scholar]
- Pallanti S, Baldini Rossi N, and Sood E. et al. Nefazodone treatment of pathological gambling: a prospective open-label controlled trial. J Clin Psychiatry. 2002 63:1034–1039. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Kavoussi RJ, and Sheline YI. et al. Impulsive aggression in personality disorder correlates with tritiated paroxetine binding in the platelet. Arch Gen Psychiatry. 1996 53:531–536. [DOI] [PubMed] [Google Scholar]
- Hollander E, Pallanti S, and Allen A. et al. Does sustained-release lithium reduce impulsive gambling and affective instability versus placebo in pathological gamblers with bipolar spectrum disorders? Am J Psychiatry. 2005 162:137–145. [DOI] [PubMed] [Google Scholar]
- Hollister LE, Schwin RL, Kasper P. Naltrexone treatment of opiate-dependent persons. Drug Alcohol Depend. 1977;2:203–209. doi: 10.1016/0376-8716(77)90027-8. [DOI] [PubMed] [Google Scholar]
- Anton RF. Pharmacologic approaches to the management of alcoholism. J Clin Psychiatry. 2001 62suppl 20. 11–17. [PubMed] [Google Scholar]
- Kim SW, Grant JE, and Adson DE. et al. Double-blind naltrexone and placebo comparison study in the treatment of pathological gambling. Biol Psychiatry. 2001 49:914–921. [DOI] [PubMed] [Google Scholar]
- Grant JE, Potenza MN, and Hollander E. et al. Multicenter investigation of the opioid antagonist nalmefene in the treatment of pathological gambling. Am J Psychiatry. 2006 163:303–312. [DOI] [PubMed] [Google Scholar]
- Kim SW, Grant JE, and Yoon G. et al. Safety of high-dose naltrexone treatment: hepatic transaminase profiles among outpatients. Clin Neuropharmacol. 2006 29:77–79. [DOI] [PubMed] [Google Scholar]
- Zwar N, Richmond R. Bupropion sustained release: a therapeutic review of Zyban. Aust Fam Physician. 2002;31:443–447. [PubMed] [Google Scholar]
- Welte JW, Wieczorek WF, and Barnes GM. et al. The relationship of ecological and geographic factors to gambling behavior and pathology. J Gambl Stud. 2004 20:405–410. [DOI] [PubMed] [Google Scholar]