Abstract
Background
The impact of the use of drug-eluting stents in percutaneous coronary intervention (PCI) on cardiac care is still uncertain. We examined the influence of systemic factors, such as hospital ownership status, organizational characteristics and payment structure, on the use of drug-eluting stents in PCI and the effect on cardiac surgery volume.
Methods
We conducted a cross-sectional analysis of drug-eluting stent use in 12 993 patients undergoing PCI with stenting (drug-eluting or bare-metal) and time-series regression analyses of the monthly number of cardiac surgery and PCI procedures performed using data collected from 1998 to 2004 at 13 public and private hospitals in the Emilia-Romagna region of Italy.
Results
Public hospitals used drug-eluting stents more selectively than private hospitals, targeting the new device to patients at high risk of adverse events. The time-series regression analyses showed that the number of PCI procedures performed per year increased during this period, both in public (slope coefficient 36.4, 95% confidence interval [CI] 30.2 to 43.1) and private centres (slope coefficient 6.4, 95% CI 3.1 to 9.2 ). Concurrently, there was a reduction in the number of isolated coronary artery bypass graft (CABG) surgeries, although the degree of change was higher in public than in private hospitals (coefficient –16.1 v. –6.2 respectively ). The number of CABG procedures associated with valve surgery decreased in public hospitals (coefficient –5.0, 95% CI –6.1 to –3.8) but increased in private hospitals (coefficient 4.1, 95% CI 2.0 to 6.1).
Interpretation
Public and private hospitals behaved differently in adopting drug-eluting stents and in using PCI with drug-eluting stents as a substitute for surgical revascularization.
The use of drug-eluting stents in percutaneous coronary intervention (PCI) is shaping a new pattern of care for patients with coronary artery disease. For example, in routine clinical practice drug-eluting stents appear to be used in patients who differ from those in clinical trials, and even in patients traditionally referred for coronary artery bypass graft (CABG) surgery.1–5 Although traditional factors associated with the adoption of new technologies have certainly played an important role here, system-wide financial and organizational incentives may also be influencing the use of drug-eluting stents in PCI.
We conducted a study to examine the association between the acquisition and use of drug-eluting stents in the Italian Servizio Sanitario Nazionale (SSN), a national health care system in which both public and private health care facilities receive public financing, and hospital ownership (public v. private for-profit), hospital payment structure (diagnosis-related group [DRG]-based prospective payment system v. full-cost reimbursement) and organizational characteristics (the availability of on-site cardiac surgery facilities).
The timing of this study is particularly relevant, given the current debate on increasing the role of private facilities in publicly funded health care in the United Kingdom6 and Canada.7 It is generally assumed that new medical technologies are adopted too quickly and used too frequently in private health care systems, as a form of non-price competition.8 In contrast, the late adoption and underuse of new technologies is the traditional Achilles heel of public health care systems. However, although the costs and patient outcomes in public and private hospitals have been extensively debated,9–11 little is known about the influence of hospital ownership status on the adoption and use of new medical technologies.
Methods
The health care system in Italy is similar to the UK system, with universal access and comprehensive coverage in a publicly funded system in which care is provided by both public and private facilities.12 In Italy, the responsibility for health care delivery rests within each region with the publicly funded Aziende Sanitarie Locali (ASLs). Public hospitals are directly managed by the ASLs, excluding those that have either teaching status or provide tertiary care. Teaching hospitals and tertiary care hospitals are managed by Aziende Ospedaliere (AOs), semi-independent public enterprises that are similar to hospital trusts in the UK National Health Service. Most private hospitals within the SSN are for-profit facilities and account for 14% of the total number of hospital admissions nationally.13 Both private for-profit hospitals and public AOs are paid by ASLs on a DRG-based prospective payment scheme, with tariffs established by the region.13 Public hospitals other than AOs are directly managed by ASLs and are funded on a full-cost basis.
In Emilia-Romagna, a region of Italy with 4 million residents, cardiac care is directed through a regional hub-and-spoke model that includes both public and private facilities. Each of the 6 cardiac surgery centres (hubs) are assigned a catchment area that includes a network of cardiology departments and wards (spokes).14 A regional commission of clinicians from both public and private hospitals define the projected need for cardiac surgery and interventional cardiology for the area and develops organizational and clinical appropriateness criteria.
Of the 6 open-heart surgical facilities in Emilia-Romagna, 4 are located in private hospitals and account for 60% of the total number of cardiac surgeries performed in the region. The remaining 2 facilities are public AOs with teaching status. These 6 hospitals also have interventional cardiology centres. In addition, 7 interventional cardiology centres are located in public hospitals that are managed directly by the ASLs and that do not have open-heart surgical facilities.
When drug-eluting stents became available in April 2002, the regional commission of clinicians developed guidelines that targeted the use of drug-eluting stents to patients at high risk of restenosis.1 The development of this policy relied mostly on expert opinion; however, the policy has proven to be both clinically sound15 and cost-effective.16,17
We compared private hospitals that had open-heart surgical facilities (n = 4) and public hospitals, both with (n = 2) and without (n = 7) open-heart surgical facilities, using 3 sets of indicators: (a) the rate of drug-eluting stent use, both overall and among patients undergoing PCI for multivessel coronary artery disease; (b) the selectivity of drug-eluting stent use (e.g., the rate of drug-eluting stent use among patients deemed to be at high risk of a major adverse cardiac event according to regional guidelines); and (c) the volume of cardiac surgery, both overall and for CABG and valve surgery.
To account for potential confounding variables, we used logistic regression analysis to estimate the likelihood (expressed as an odds ratio [OR] and adjusted for case mix) of receiving a drug-eluting stent (dependent variable). Covariates included in the model were selected by univariate analysis exploring the association between the use of drug-eluting stents, patient characteristics (age, sex, diabetes mellitus, hypertension, smoking status, hypercholesterolemia, previous revascularization, clinical indication, multivessel disease, high-risk lesions) and the calendar year. Covariates with a statistically significant (p < 0.05) association were included in the logistic model, with fit assessed by means of the Hosmer–Lemeshow test.18 A few of the variables had missing values, although this was less than 5% of the total number of values for each variable. Thus, all of the patients were retained in the multivariable analysis.
Information was drawn from the Regional PCI Registry (REAL),1,15 which reports the clinical characteristics of patients undergoing PCI and the type of stent, if used. The registry covers 95% of all PCI procedures; it is routinely tested for completeness, but not reliability, of information and meets the standard quality criteria for clinical databases.19
The monthly number of cardiac surgeries and PCI (with or without stenting) procedures performed from January 1998 to December 2004 was retrieved from the regional database of hospital admissions. This period included 84 months of data: 52 months before and 32 months after drug-eluting stents became available. All procedures were represented in the database.
The analyses were based on segmented time-series regression models applied to the monthly number of procedures, adjusted for seasonality, which allowed estimation of the slope coefficient for the phases before and after drug-eluting stents became available.20 A statistically significant difference in slope coefficients between the 2 phases indicates a long-term effect of drug-eluting stent availability. The immediate effect of drug-eluting stent availability on the number of procedures performed was assessed as a statistically significant change in the level of surgery activity, expressed as the difference between the estimated first point after drug-eluting stents became available and the extrapolated first point after drug-eluting stent availability, if the pre–drug-eluting stent line was continued into the post–drug-eluting stent phase.20 The Durbin–Watson test21 suggested a low degree of autocorrelation of the data (varying from 1.8 to 2.2).
Results
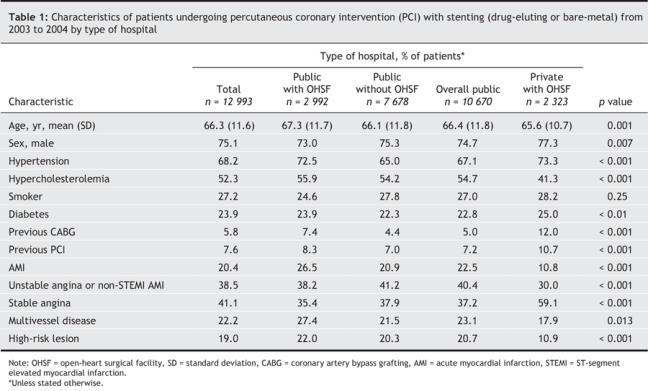
The general characteristics of patients undergoing primary PCI with stenting from 2003 to 2004 (following the availability of drug-eluting stents) are described in Table 1. Patients in the public hospitals were statistically older and more likely than patients at the private hospitals to undergo PCI for indications such as acute myocardial infraction and unstable angina. Patients with stable angina were more prevalent in the private hospitals than in the public hospitals. Patients with multivessel disease who underwent PCI with stenting were significantly more prevalent in the public centres, both with and without open-heart surgical facilities than in the private centres (Table 1). The proportion of patients with high-risk lesions (as defined by regional guidelines) was higher in the public than in the private hospitals.
Table 1
Rate of drug-eluting stent adoption
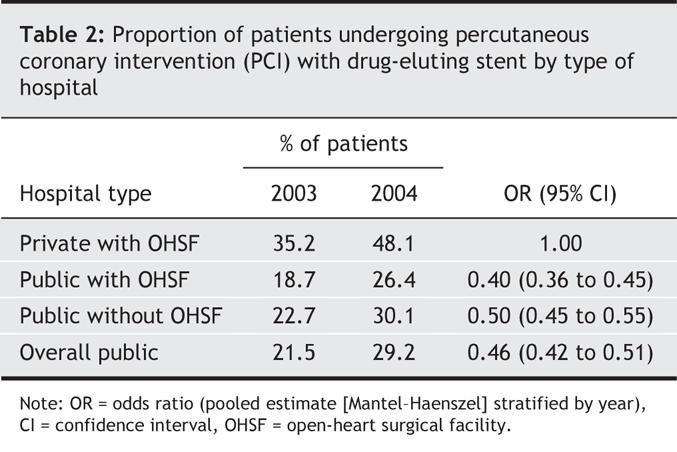
The proportion of patients who received a drug-eluting stent was higher in the private (42.1%) than in the public hospitals (25.6% overall, varying from 22.8% to 26.7% in those with and without open-heart surgical facilities respectively). This pattern was consistent in both study years, and the proportion of patients treated who received drug-eluting stents increased over time at all types of hospitals (Table 2).
Table 2
After adjustment for clinical characteristics, patients treated in public hospitals, with or without open-heart surgical facilities, consistently had a lower probability of receiving drug-eluting stents than did patients admitted to the private hospitals (Table 3).
Table 3
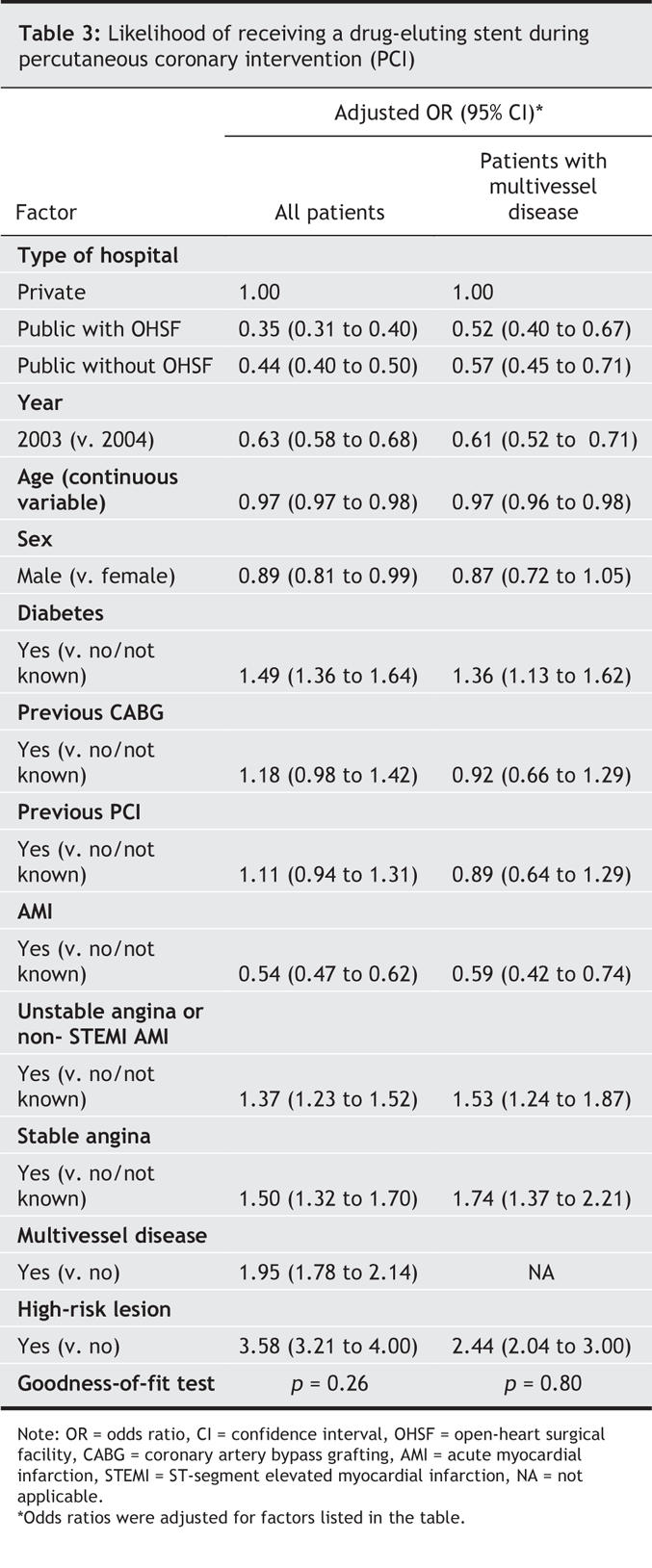
The proportion of patients with multivessel disease who received drug-eluting stents was 52.1% in private hospitals, compared with 37.5% in public hospitals with, and 40.1% in public hospitals without, open-heart surgical facilities.
Compliance with the regional guidelines was 20.8% in private hospitals versus 33.3% and 34.1% for public hospitals with and without open-heart surgical facilities respectively. Public hospitals with open-heart surgical facilities were more likely than private hospitals to use drug-eluting stents in patients with high-risk lesions (OR 1.30, 95% CI 1.03 to 1.64). The same held true for public hospitals without open-heart surgical facilities (OR 2.64, 95% CI 2.21 to 3.15).
Impact of drug-eluting stent availability on PCI and cardiac surgery volume
The number of cardiac surgical procedures performed in public hospitals decreased 5.1% after drug-eluting stents became available in 2002: the mean number of procedures per year was 1322 during 2003–2004, compared with 1394 during 1998–2002. There was a 21.4% reduction in the number of isolated CABG surgeries performed (783 during 1998–2002 v. 615 during 2003–2004), which was more than compensated for by the increase in valve surgery, both isolated (7.1%) and those associated with CABG (15.2%).
In private hospitals, the mean number of surgical interventions performed per year remained stable (2018 during 1998–2002 v. 2007 during 2003–2004). The number of isolated CABG surgeries decreased in both public and private hospitals; however, the level of reduction of isolated CABG surgeries was lower in private hospitals than in public hospitals (16.2%), and this was associated with an increase in the number of valve surgeries, both isolated (31.3%) and associated with CABG (12.1%).
Time-series regression analyses showed that drug-eluting stent availability was associated with a statistically significant reduction in the overall number of cardiac procedures performed per year in public hospitals (coefficient –20.1, 95% CI –23.2 to –17.1), while the degree of reduction was much smaller in private hospitals (coefficient –1.8, 95% CI –6.4 to –2.8) (Table 4). This pattern is explained by the higher level of reduction in isolated CABG surgeries in public hospitals than in private hospitals (coefficient –16.1 v. –6.2 respectively), whereas CABG procedures associated with valve surgery decreased in public hospitals and increased in private ones (Table 4).
Table 4
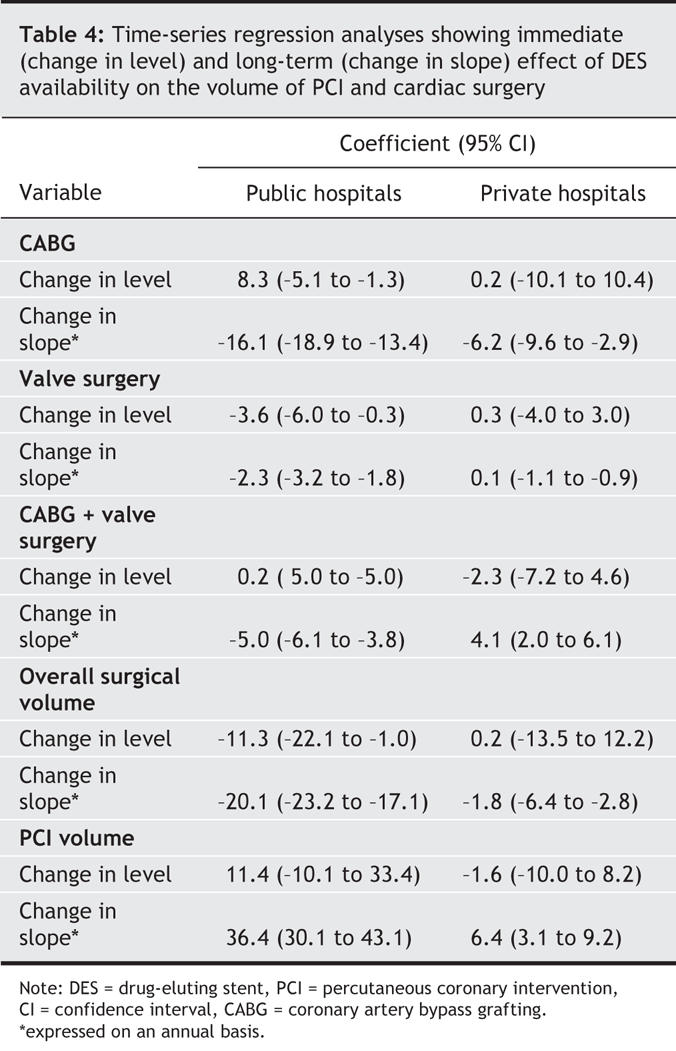
Drug-eluting stent availability was also associated with a substantial increase in the number of PCI procedures in public hospitals (coefficient 36.4, 95% CI 30.1 to 43.1), whereas the corresponding increase in private hospitals was much lower (coefficient 6.44, 95% CI 3.1 to 9.2) (Table 4).
Interpretation
Drug-eluting stents were used more frequently in private hospitals than in public hospitals, both overall and in the subset of patients with multivessel disease, regardless of the availability of open-heart surgical facilities. Public hospitals used drug-eluting stents sparingly and more selectively in patients with high-risk lesions, as defined by the regional guidelines. Drug-eluting stents seemed to be used as a substitute for CABG surgery in public, but not in private, hospitals.
In private hospitals, the total number of cardiac surgery cases remained stable, because the small reduction in the number of CABG procedures was compensated for by an increase in valve surgery, either alone or in combination with CABG. Public hospitals with open-heart surgical facilities used PCI with stenting in patients with multivessel disease more extensively and had a significantly higher level of reduction in the number of CABG and total cardiac surgeries compared with private hospitals.
One limitation of our study is that the inference of the use of drug-eluting stents as a substitute for, or as a complement to, CABG surgery is drawn indirectly from a cross-sectional assessment of the use of the former, combined with a time-series analysis on the trend of volumes of the latter. One might argue that the different pattern of drug-eluting stent use in public and private hospitals could have been affected by factors not accounted for in our analysis, such as patient choice or the health professionals' skills. However, the use of drug-eluting stents does not require additional skills, and 1.7% of patients requested the use of a drug-eluting stent.22
Completeness and accuracy of the data in the regional PCI registry could be another potential source of concern.19 Routine monitoring shows that the REAL database includes 95% of patients undergoing PCI at regional hospitals, and the proportion of missing variables is low. Although we have not tested the reliability of the information in REAL, there is no reason to anticipate that the data collected at private and public hospitals would systematically differ.
Research implications
We found that both the type of hospital payment structure and ownership status influenced drug-eluting stent adoption and its use as a substitute for CABG surgery. Most of the public hospitals in our study do not have open-heart surgical facilities, are directly managed by ASLs and are funded on a full-cost basis. ASLs experience a financial loss when their hospitals, both private and AOs, do not substitute CABG surgery with PCI and drug-eluting stents, because the hospital must pay a DRG-based tariff for CABG surgery. For these directly managed hospitals, therefore, economic incentives favour substituting CABG with PCI and stenting. This both supports the hospital's reputation and allows it to remain self-sufficient. AOs and private for-profit hospitals have in-house open-heart surgical facilities and are paid prospectively on a per case basis. CABG is seen as revenue-enhancing surgery, and both AOs and private hospitals face direct incentives to increase its use, provided that the tariffs are higher than the per case operating costs.23 In a similar context, the critical role of organizational factors has been convincingly shown to favour CABG over PCI, particularly for patients who are “at the margin” of the 2 techniques,24,25 such as those with multivessel disease.
A major difference between AOs and private hospitals is their incentive for recovering the cost of their investment in open-heart surgical facilities. Cardiac surgery is a profitable service that requires relatively high capital investments26 that could be made redundant by the advent of the new technology (PCI plus drug-eluting stents). Recovering the initial investment requires maintaining a high volume of CABG surgery or of other combined surgical services, such as valvuloplasty, which makes use of the same production factors. This might explain the lower number of patients with multivessel disease who were referred to private centres for PCI and the relatively stable number of cardiac surgeries performed in private hospitals. Although public AOs are, in theory, exposed to the same incentives, they may adopt different behaviours because their capital costs are perceived to be low, since they are funded by the region and there is no incentive for a yearly return on assets in use. In addition, the reputation of hospitals and health professionals might also influence cardiac surgeons to abandon CABG for more sophisticated forms of cardiac surgery, such as pediatric cardiac surgery and heart transplant, which are not performed in private hospitals.
Policy implications
In our study, drug-eluting stent availability was associated with a reduction in the total cardiac surgery volume. This level of reduction, however, depends on the relative proportion of public and private hospitals. Since cardiac surgery volume is associated with patient outcomes,27–30 the use of PCI with drug-eluting stents in place of CABG, and hence a reduction in surgery volume, could have a negative impact on surgeons' clinical competence.
Our results show that hospital ownership status and payment structure have a strong impact on the adoption and use of drug-eluting stents. In private for-profit hospitals, PCI with drug-eluting stents could have been a “disruptive technology” (a technology that, despite possibly outperforming the existing technology, is not adopted because of the high capitalization costs invested in the older technology); however, valve surgery compensated for CABG and made room for the rapid adoption of drug-eluting stents.31
In addition, our findings raise the issue of whether performing cost-effectiveness analyses that focus solely on comparing alternative technologies, without considering the broader system-wide incentives, is relevant.32 For example, at current prices, the actual cost-effectiveness of drug-eluting stent use mainly depends on whether it is targeted to patients at high risk of an adverse cardiac event that may be prevented by the use of the new device.33,34 Our findings suggest that private centres may use drug-eluting stents less selectively in high-risk patients, which may jeopardize the cost-effectiveness of this innovation.
Conclusion
The case of drug-eluting stent adoption and use illustrates that the clinical environment is a complex system, in which the introduction of a new element in one sector (e.g., drug-eluting stents for PCI) has a “ripple effect” on several other seemingly unrelated sectors (e.g., valve surgery). The size and direction of these “ripples” is influenced by health care system and hospital characteristics, such as ownership status and payment structure, and by the relative proportion of public and private providers in the system.
@ See related articles, pages 195 and 199
Acknowledgments
We acknowledge the contribution of clinicians participating in the REAL registry. This study was supported by Agenzia Sanitaria Regionale of Emilia-Romagna.
Footnotes
Published at www.cmaj.ca on Dec. 19, 2006. Revised on Dec. 28, 2006.
This article has been peer reviewed.
Contributors: Roberto Grilli conceived the study design, drafted the first version of the manuscript and wrote the final version. Paolo Guastaroba conducted the statistical analyses and contributed to the writing of the first draft. Francesco Taroni conceived the study design, revised and significantly improved the first draft of the manuscript and with RG wrote the final version. All of the authors contributed to the interpretation of data and approved the final version of the manuscript.
Competing interests: None declared.
Correspondence to: Dr. Roberto Grilli, Agenzia Sanitaria Regionale, Viale Aldo Moro, 21, 40127 Bologna, Italy; fax +39-051-6397049; rgrilli@regione.emilia-romagna.it
REFERENCES
- 1.Grilli R, Taroni F. Managing the introduction of expensive medical procedures: use of a registry. J Health Serv Res Policy 2006;11:89-93. [DOI] [PubMed]
- 2.Chu WW, Waksman R. Contemporary use of drug-eluting stents. Curr Treat Options Cardiovasc Med 2005;7:35-46. [DOI] [PubMed]
- 3.Maynard C, Lowy E, Wagner T, et al. Utilization of drug-eluting stents in the Veterans Health Administration. Am J Cardiol 2005;96:218-20. [DOI] [PubMed]
- 4.Swanson N, Gershlick AH. Drug eluting stents in interventional cardiology — current evidence and emerging uses. Curr Drug Targets Cardiovasc Haematol Disord 2005;5:313-21. [DOI] [PubMed]
- 5.Thompson CA, Kaplan AV, Jayne JE, et al. Impact and temporal trends of percutaneous coronary intervention in the drug-eluting stent versus bare metal stent eras. Am J Cardiol 2005;96:668-72. [DOI] [PubMed]
- 6.Dash P. New providers in UK health care. BMJ 2004;328:340-2. [DOI] [PMC free article] [PubMed]
- 7.McIntosh T. Don't panic: the hitchhiker's guide to Chaoulli, wait times and the politics of private insurance. Canadian Policy Research Networks; 2006 Feb 24. Available: www.cprn.com/en/doc.cfm?doc=1394# (accessed 2006 Oct 31).
- 8.Institute of Medicine. Assessing medical technologies. Washington: National Academy Press; 1985.
- 9.Sloan FA, Trodgon JG, Curtis LH, et al. Does the ownership of the admitting hospital make a difference? Outcomes and process of care of Medicare beneficiaries admitted with acute myocardial infarction. Med Care 2003;41:1193-205. [DOI] [PubMed]
- 10.Devereaux PJ, Schunemann HJ, Ravindran N, et al. Comparison of mortality between private for-profit and private not-for-profit hemodialysis centres. A systematic review and meta-analysis. JAMA 2002;288:2449-57. [DOI] [PubMed]
- 11.Devereaux PJ, Choi PT, Lacchetti C, et al. A systematic review and meta-analysis of studies comparing mortality rates of private for-profit and private not-for-profit hospitals. CMAJ 2002;166:1399-406. [PMC free article] [PubMed]
- 12.France G, Taroni F. The evolution of health policy making in Italy. J Health Polit Policy Law 2005;30:169-87. [DOI] [PubMed]
- 13.France G, Taroni F, Donatini A. The Italian health-care system. Health Econ 2005;14:S187-202. [DOI] [PubMed]
- 14.Nobilio L, Fortuna D, Vizioli M, et al. Impact of regionalisation of cardiac surgery in Emilia-Romagna, Italy. J Epidemiol Community Health 2004;58:97-102. [DOI] [PMC free article] [PubMed]
- 15.Marzocchi A, Piovaccari G, Manari A, et al. Comparison of effectiveness of sirolimus-eluting stents vs bare metal stents for percutaneous coronary intervention in patient at high risk for coronary restenosis or clinical adverse events. Am J Cardiol 2005;95:1409-14. [DOI] [PubMed]
- 16.Brophy JM, Erickson LJ. Cost-effectiveness of drug-eluting coronary stents in Quebec, Canada. Int J Technol Assess Health Care 2005;21:326-33. [DOI] [PubMed]
- 17.Shrive FM, Manns BJ, Galbraith PD, et al; APPROACH Investigators. Economic evaluation of sirolimus-eluting stents. CMAJ 2005;172:345-51. [DOI] [PMC free article] [PubMed]
- 18.Hosmer DW, Lemeshow S. Applied logistic regression. New York: John Wiley & Sons; 1989.
- 19.Black N, Payne M. Directory of clinical databases: improving and promoting their use. Qual Saf Health Care 2003;12:348-52. [DOI] [PMC free article] [PubMed]
- 20.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27:299-309. [DOI] [PubMed]
- 21.Draper N, Smith H. Applied regression analysis. New York: Wiley; 1981.
- 22.Guastaroba P, Fiorini M, Grilli R. Valutazione dell'impatto clinico ed economico della strategia di adozione degli stent a rilascio di farmaco per gli interventi di angioplastica coronarica [Report no 91]. Bologna (Italy): Agenzia Sanitaria Regionale; 2004.
- 23.Medical Technology and Costs of the Medicare Program Advisory Panel. Diagnosis-related groups (DRGs) and the medicare program: implications for medical technology. A technical memorandum. Washington: US Congress, Office of Technology Assessment; 1983. Available: http://govinfo.library.unt.edu/ota/Ota_4/DATA/1983/8306.PDF (accessed 2006 Oct 31).
- 24.Huckman RS. The utilization of competing technologies within the firm: evidence from cardiac procedures. Manage Sci 2003;49:599-617.
- 25.Huckman RS, Pisano GP. Turf battles in coronary revascularization. N Engl J Med 2005; 352:857-9. [DOI] [PubMed]
- 26.Horwitz JR. Does corporate ownership matter? Service provision in the hospital industry [NBER Working Paper no 11376]. Cambridge (MA): National Bureau of Econ omic Research; 2005.
- 27.Ferguson B, Rice N, Sykes D, et al. Hospital volume and health care outcomes, costs and patient access. Eff Health Care 1996;2(8). Available: www.york.ac.uk/inst/crd/ehc28.pdf (accessed 2006 Oct 31).
- 28.Gandjour A, Bannenberg A, Lauterbach KW. Threshold volumes associated with higher survival in health care. A systematic review. Med Care 2003;41:1129-41. [DOI] [PubMed]
- 29.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 2002;137:511-20. [DOI] [PubMed]
- 30.Sowden A, Aletras V, Place M, et al. Volume of clinical activity in hospitals and healthcare outcomes, costs, and patient access. Qual Health Care 1997;6:109-14. [DOI] [PMC free article] [PubMed]
- 31.Christensen CH. The innovator's dilemma: when new technologies cause great firms to fail. Boston: Harvard Business School Press; 1997.
- 32.Greenberg D, Bakhai A, Cohen DJ. Can we afford to eliminate restenosis? Can we afford not to? J Am Coll Cardiol 2004;43:513-8. [DOI] [PubMed]
- 33.Bagust A, Grayson AD, Palmer ND, et al. Cost effectiveness of drug eluting coronary artery stenting in a UK setting: cost-utility study. Heart 2006;92:68-74. [DOI] [PMC free article] [PubMed]
- 34.Kaiser C, Brunner-La Rocca HP, Buser PT, et al. Incremental cost-effectiveness of drug eluting stents compared with a third-generation bare-metal stent in a real-world setting: randomised Basel Stent Kosten Effectivitats Trial (BASKET). Lancet 2005;366:921-9. [DOI] [PubMed]


