Intracardiac migration of an inferior vena cava (IVC) filter is an extremely rare complication. Only a few cases have been reported in the world medical literature.1–5 The filter is usually entrapped in the tricuspid valve, which results in insufficiency of the valve.1–5 In uncomplicated cases, the filter can be removed via the percutaneous transvenous approach.3,4 However, the entrapped filter may cause ventricular arrhythmia1 or paradoxical embolization5 that results in profound hemodynamic disturbance. Herein, we report a case of acute massive pulmonary embolization with hemodynamic collapse that required an emergency operation.
Clinical Summary
In November 2005, a 56-year-old man (weight, 75 kg) was admitted to our hospital with severe shortness of breath, abdominal pain, and tachycardia. He had experienced an episode of deep venous thrombosis 16 years before, which had been treated with warfarin for 6 months, but he had remained in good health since then. Our laboratory findings included microcytic anemia (hemoglobin, 92 g/L) and fibrinolysis (dimerized plasmin fragment D, 4.6 mg/L). A computed tomographic scan showed thrombi in the segmental pulmonary arteries and in the popliteal veins bilaterally, and a thickened right colon with regional lymphadenopathy. Results of a colonoscopy confirmed a moderately differentiated adenocarcinoma of the colon, stage T3 N2 M0, Dukes stage C; surgery was scheduled for 3 weeks later. The patient's IVC was 2.5 cm in diameter when a Simon nitinol IVC filter (Bard Peripheral Vascular, Inc.; Tempe, Ariz) was placed in mid-November. The patient was discharged with a prescription for 80 mg of subcutaneously injected enoxaparin twice daily.
The enoxaparin was discontinued on the night before surgery. A right hemicolectomy was performed; afterwards, the patient received 5,000 units of subcutaneous heparin twice daily as an anticoagulant. Four days later, he collapsed while walking around the ward. He did not require chest compression and was resuscitated promptly. A central venous line was placed. Although the patient's condition was stabilized, he remained hypotensive, tachycardic, and short of breath despite appropriate oxygen supplementation.
Urgent transthoracic echocardiography revealed severe distention of the right ventricle (Fig. 1A) and an echogenic mass in the tricuspid valve (Fig. 1B). The patient underwent emergency surgery with cardiopulmonary bypass on the beating heart. The right atrium was opened first, and the IVC filter—lodged in the tricuspid valve—was removed (Fig. 2A). A large thrombus in the shape of the IVC bifurcation (Fig. 2B) was removed from the pulmonary artery. A new IVC filter (OptEase®, Cordis Corporation, a Johnson & Johnson company; Miami Lakes, Fla) was placed immediately after surgery.
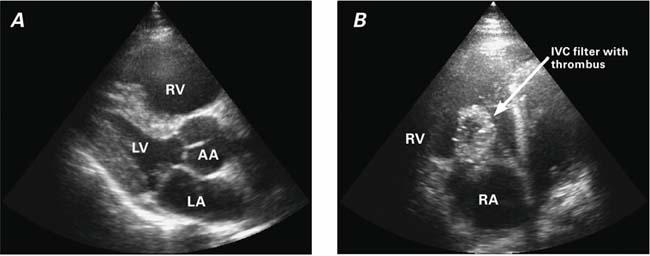
Fig. 1 Transthoracic echocardiography shows A) right ventricular distention and B) a mass in the tricuspid valve.
AA = ascending aorta; IVC = inferior vena cava; LA = left atrium; LV = left ventricle; RA = right atrium; RV = right ventricle
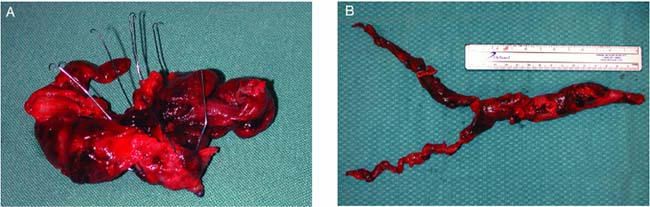
Fig. 2 The filter was removed (A), as was a thrombus (B), which was formed in the shape of the inferior vena caval bifurcation.
The patient was given warfarin (international normalized ratio, 2–2.5) as an anticoagulant, and he was discharged from the hospital in early December 2005. At the 10-month follow-up examination, he was doing well.
Comment
Migration of an IVC filter to the heart is a rare event that can result in massive pulmonary embolism. We believe that insufficient anticoagulation before our patient's general surgical procedure contributed to the accumulation of thrombi at the IVC filter. Subsequent dislodgment of the filter produced a life-threatening pulmonary embolism. Immediate intervention by the cardiothoracic surgical team saved this patient's life.
Two important issues can be emphasized. First, IVC filters can become overloaded with emboli unless adequate anticoagulation is instituted promptly and is continued for at least 6 months after placement of the IVC filter. Second, because a dislodged IVC filter can result in acute massive thromboembolism that necessitates urgent open-heart surgery, we strongly recommend that any high-risk surgical or medical intervention in patients who have an IVC filter be performed in a hospital where cardiothoracic surgery is available.
Footnotes
Address for reprints: Igor E. Konstantinov, MD, PhD, Department of Cardiothoracic Surgery, Sir Charles Gairdner Hospital, Nedlands, Perth, WA 6009, Australi. E-mail: igorkonst@hotmail.com
References
- 1.Izutani H, Lalude O, Gill IS, Biblo LA. Migration of an inferior vena cava filter to the right ventricle and literature review. Can J Cardiol 2004;20:233–5. [PubMed]
- 2.James KV, Sobolewski AP, Lohr JM, Welling RE. Tricuspid insufficiency after intracardiac migration of a Greenfield filter: case report and review of the literature. J Vasc Surg 1996;24: 494–8. [DOI] [PubMed]
- 3.Queiroz R, Waldman DL. Transvenous retrieval of a Greenfield filter lodged in the tricuspid valve. Cathet Cardiovasc Diagn 1998;44:310–2. [DOI] [PubMed]
- 4.Arjomand H, Surabhi S, Wolf NM. Right ventricular foreign body: percutaneous transvenous retrieval of a Greenfield filter from the right ventricle–a case report. Angiology 2003; 54:109–13. [DOI] [PubMed]
- 5.Porcellini M, Stassano P, Musumeci A, Bracale G. Intracardiac migration of nitinol TrapEase vena cava filter and paradoxical embolism. Eur J Cardiothorac Surg 2002;22:460–1. [DOI] [PubMed]


