Abstract
Left main coronary artery dissection occurs very rarely during selective coronary angiography, but it generally progresses to complete coronary occlusion. The traditional treatment of occlusive dissection of the unprotected left main coronary artery has been surgical. Percutaneous treatment has been sporadic and controversial. We report a case of iatrogenic occlusive dissection of the unprotected left main coronary artery during diagnostic coronary angiography, followed by successful stenting of the lesion.
Key words: Angioplasty, balloon; aneurysm, dissecting/etiology; coronary angiography/adverse effects; coronary stenosis/etiology; coronary vessels/injuries; iatrogenic disease; myocardial revascularization; stents
Acute occlusive dissection of the left main coronary artery (LMCA) occurs very rarely during diagnostic coronary angiography. However, occlusive dissection of LMCA is a dramatic condition that has a very high mortality rate if it is not treated. Traditionally, coronary artery bypass grafting (CABG) has been considered the treatment of choice for this condition.1,2 Although emergency CABG is effective, it is a time-consuming procedure. Recently, percutaneous revascularization has been preferred over CABG in order to re-establish the patency of the LMCA more rapidly.3–7 In spite of improvements in balloon angioplasty techniques, the advent of stents, and new antiplatelet regimens, published reports about successful percutaneous revascularization in cases of unprotected-LMCA stenosis are limited,8–11 and there are only a few reports of successful percutaneous revascularization in cases of acute occlusive dissection of the LMCA.3–7 We describe a case of iatrogenic occlusive dissection of the LMCA during coronary angiography and of subsequent percutaneous revascularization of the LMCA, left anterior descending (LAD), and left circumflex (LCx) coronary arteries with stenting.
Case Report
A 56-year-old man presented with a 1-year history of angina on exertion (Canadian Cardiovascular Society class II12) followed by dyspnea for a year. On admission, the patient's arterial pressure was 130/70 mmHg, and his heart rate was 84 beats/min. He underwent diagnostic left heart catheterization and coronary angiography. Ventriculography showed normal left ventricular function. The right coronary artery was normal, and no collateral vessels supplied the left system. Left coronary angiography revealed a normal arterial tree.
A few minutes after the procedure, the patient developed oppressive substernal chest pain radiating to the back, followed by dyspnea and profuse sweating, and his blood pressure level fell to 80/50 mmHg. The electrocardiogram showed ST-segment elevation on the anterior electrocardiographic leads (Fig. 1A). Coronary angiography revealed LMCA dissection that extended into the LAD and stenosis of the proximal segment of the LAD (Fig. 2A). Due to the patient's critical status, CABG would have caused a great risk of death. It was decided that angioplasty on the LMCA would save time.
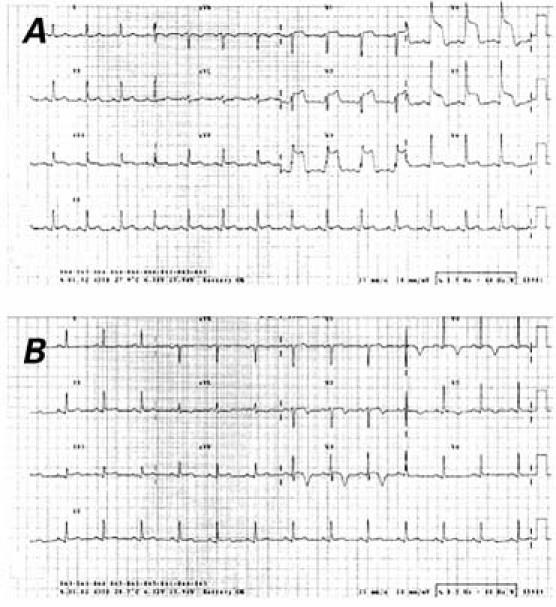
Fig. 1 Electrocardiography shows A) ST–segment elevation on the anterior electrocardiographic leads just after occlusive dissection of the left main coronary artery, and B) disappearance of the ST–segment elevation after percutaneous intervention.
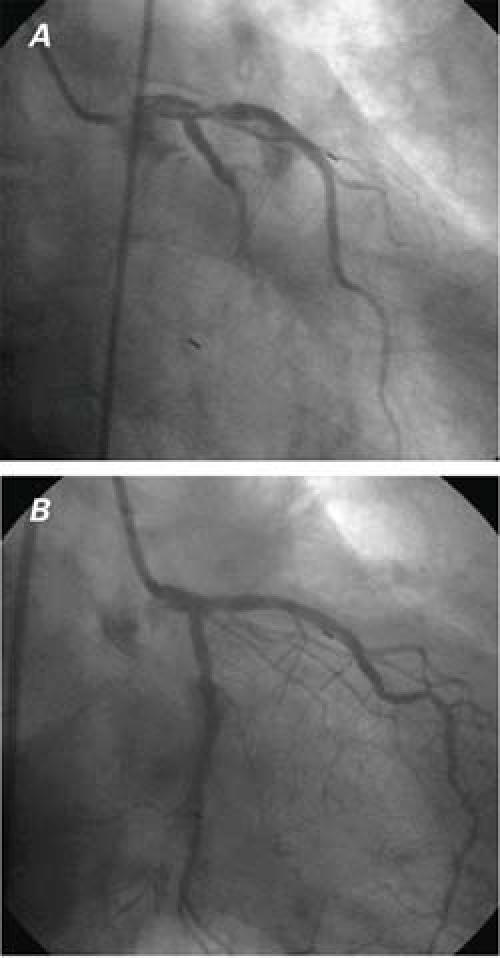
Fig. 2 Right anterior oblique view of the left coronary angiogram. A) Occlusive dissection of the left main coronary artery before percutaneous intervention. B) Normal coronary flow from the left main coronary artery to the left anterior descending and left circumflex arteries after stent implantation.
In the catheterization laboratory, the stump of the LMCA was engaged with an 8F guiding catheter (Cordis, a Johnson & Johnson company; Miami Lakes, Fla), and contrast injection revealed TIMI I (Thrombolysis in Myocardial Infarction I) flow in the LAD. A soft-tip guidewire (Neo's Soft, Asahi Intecc Co.; Nagoya, Japan) was chosen and carefully advanced into the LAD to avoid penetrating subintimal tissue. Coronary angiography ensured that the guidewire was in the true lumen of the LAD. A 20-mm × 2.0-mm Maverick® balloon (Boston Scientific/Scimed; Nanterre Cedex, France) was then placed across the LMCA to the proximal LAD and inflated to 12 atm. After inflation, some antegrade flow was restored in the LMCA to the LAD. Then, the LMCA-to-LAD dissection was stented with an 18-mm × 4-mm Ephesos stent (Nemed Ltd.; Istanbul, Turkey) to 12 atm. The final result was a normal-looking LMCA, LAD, and LCx with restoration of TIMI III flow with no residual stenosis (Fig. 2B).
After percutaneous intervention, the patient's chest pain resolved and the blood pressure rose to normal. The ST-segment elevation on the anterior electrocardiographic leads had also disappeared (Fig. 1B). However, the peak troponin I concentration was 8.5 ng/mL. Heparin was given as a bolus of 10,000 U during the procedure, followed by continuous infusion for 3 days to maintain an activated clotting time of 360 seconds. The patient received clopidogrel (loading dose, 300 mg; followed by 75 mg daily) and aspirin (300 mg daily) after the procedure. After an uneventful period, the patient was discharged on postprocedural day 6 as asymptomatic and was maintained on clopidogrel (75 mg daily) and aspirin (300 mg daily). At 6 months of follow-up, he was symptom-free, and results of exercise testing were negative. The patient refused further angiography, and, on the basis of the 6-month results, we did not insist on performing the procedure. No major cardiac events have occurred during the follow-up period.
Discussion
Coronary angiography is a routine diagnostic procedure in current clinical practice. Life-threatening complications, such as dissection of the LMCA, can arise during coronary angiography in a small number of patients.3–7 The exact mechanism of LMCA dissection is unclear. However, such dissection in our patient could have resulted from vigorous hand-injection of contrast medium, subintimal passage of the guidewire, or inappropriate handling of the guidewire catheter.
If the dissection is small and there is no reduction in distal coronary flow, the natural course of iatrogenic coronary artery dissections in anatomical sites other than the LMCA is very good. Left main coronary artery dissection generally progresses to complete coronary occlusion.13,14 Left main coronary artery occlusion is the most severe form of coronary artery disease. It is a dramatic condition that has a very high mortality rate; however, early successful myocardial revascularization seems to improve survival. Traditionally, CABG has been the treatment of choice for patients with LMCA stenosis, a condition that until recently was regarded as an absolute contraindication for percutaneous intervention.1,2,15,16 Although emergency CABG is effective, it is a time-consuming procedure that entails the risk of irreversible, extensive myocardial damage. Percutaneous intervention of LMCA stenosis has emerged as a new alternative treatment, and it has been developed and improved over the past several years. At first, disappointing long-term results from the use of percutaneous angioplasty for unprotected LMCA stenosis15,17,18 led to the abandonment of such angioplasty. Later, several authors reported encouraging results after the stenting of unprotected LMCA lesions in selected patients.19–22 The combination of improvements in percutaneous transluminal coronary angioplasty techniques, the advent of stents, and the use of glycoprotein IIb/IIIa inhibitors have increased the reports of successful percutaneous intervention in unprotected LMCA stenosis. However, because catheter-induced occlusive dissection of the unprotected LMCA is quite rare, there are only a few reports of cases in which iatrogenic occlusive dissection of the LMCA has been successfully revascularized percutaneously.3–7
In our patient, initially, there was no notable stenosis of the LAD, and LAD stenosis developed after LMCA dissection during diagnostic coronary angiography. Percutaneous revascularization was preferred to CABG in order to re-establish the patency of the LMCA, LAD, and LCx more rapidly. Left main coronary artery stenting enabled prompt restoration of the coronary blood flow before extensive myocardial necrosis developed. In fact, the release of serum cardiac markers was minimal after the rescue procedure, and left ventricular function was normal.
At present, stent implantation is mandatory in the percutaneous treatment of LMCA dissection, because it achieves better flow while reducing the ischemia time due to balloon inflation. Many reports show that, in selected cases of protected or unprotected LMCA stenosis, coronary stenting yields good results, decreasing morbidity, mortality, and length of hospital stay.3–11,19–22
Conclusion
Our case confirms the effectiveness of rescue stenting of the unprotected LMCA for the treatment of life-threatening occlusive dissection, by promptly re-establishing coronary blood flow to the myocardium.
Footnotes
Address for reprints: Talantbek Batyraliev, MD, Sani Konukoglu Tip Merkezi, Ali Fuat Cebesoy Bulvari, 27090 Gaziantep, Turkey. Email: talantbekb@yahoo.com
References
- 1.Connors JP, Thanavaro S, Shaw RC, Sandza JG, Ludbrook PA, Krone RJ. Urgent myocardial revascularization for dissection of the left main coronary artery: a complication of coronary angiography. J Thorac Cardiovasc Surg 1982;84: 349–52. [PubMed]
- 2.Slack JD, Pinkerton CA, VanTassel JW, Orr CM. Left main coronary artery dissection during percutaneous transluminal coronary angioplasty. Cathet Cardiovasc Diagn 1986;12: 255–60. [DOI] [PubMed]
- 3.Grenadier E, Roguin A, Nikolsky E, Zdorovyak A, Cohen S. Acute left main dissection with complete obliteration of flow followed by emergency stenting without predilatation. Int J Cardiovasc Intervent 2000;3:245. [DOI] [PubMed]
- 4.Mulvihill NT, Boccalatte M, Fajadet J, Marco J. Catheter-induced left main dissection: a treatment dilemma. Catheter Cardiovasc Interv 2003;59:214–6. [DOI] [PubMed]
- 5.Al-Saif SM, Liu MW, Al-Mubarak N, Agrawal S, Dean LS. Percutaneous treatment of catheter-induced dissection of the left main coronary artery and adjacent aortic wall: a case report. Catheter Cardiovasc Interv 2000;49:86–90. [DOI] [PubMed]
- 6.Awadalla H, Salloum JG, Smalling RW, Sdringola S. Catheter-induced dissection of the left main coronary artery with and without extension to the aortic root: a report of two cases and a review of the literature. J Interv Cardiol 2004;17:253–7. [DOI] [PubMed]
- 7.Garcia-Robles JA, Garcia E, Rico M, Esteban E, Perez de Prado A, Delcan JL. Emergency coronary stenting for acute occlusive dissection of the left main coronary artery. Cathet Cardiovasc Diagn 1993;30:227–9. [DOI] [PubMed]
- 8.Nageh T, Thomas MR, Wainwright RJ. Safety and eficacy of unprotected left main coronary artery stenting. Circulation 2002;105:e85. [DOI] [PubMed]
- 9.Brueren BR, Ernst JM, Suttorp MJ, ten Berg JM, Rensing BJ, Mast EG, et al. Long term follow up after elective percutaneous coronary intervention for unprotected non-bifurcational left main stenosis: is it time to change the guidelines? Heart 2003;89:1336–9. [DOI] [PMC free article] [PubMed]
- 10.Tan WA, Tamai H, Park SJ, Plokker HW, Nobuyoshi M, Suzuki T, et al. Long-term clinical outcomes after unprotected left main trunk percutaneous revascularization in 279 patients. Circulation 2001;104:1609–14. [DOI] [PubMed]
- 11.Karam C, Fajadet J, Cassagneau B, Laurent JP, Jordan C, Laborde JC, Marco J. Results of stenting of unprotected left main coronary artery stenosis in patients at high surgical risk. Am J Cardiol 1998;82:975–8. [DOI] [PubMed]
- 12.Goldman L, Hashimoto B, Cook EF, Loscalzo A. Comparative reproducibility and validity of systems for assessing cardiovascular functional class: advantages of a new specific activity scale. Circulation 1981;64:1227–34. [DOI] [PubMed]
- 13.Kennedy JW, Baxley WA, Bunnel IL, Gensini GG, Messer JV, Mudd JG, et al. Mortality related to cardiac catheterization and angiography. Cathet Cardiovasc Diagn 1982;8:323–40. [DOI] [PubMed]
- 14.Zelinger AB, Shulruff S, Pouget JM. Signiicant left main stenosis following asymptomatic dissection during coronary arteriography. Chest 1983;83:568–9. [DOI] [PubMed]
- 15.Takaro T, Peduzzi P, Detre KM, Hultgren HN, Murphy ML, van der Bel-Kahn J, et al. Survival in subgroups of patients with left main coronary artery disease. Veterans Administration Cooperative Study of Surgery for Coronary Arterial Occlusive Disease. Circulation 1982;66:14–22. [DOI] [PubMed]
- 16.Chaitman BR, Fisher LD, Bourassa MG, Davis K, Rogers WJ, Maynard C, et al. Effect of coronary bypass surgery on survival patterns in subsets of patients with left main coronary artery disease. Report of the Collaborative Study in Coronary Artery Surgery (CASS). Am J Cardiol 1981;48:765–77. [DOI] [PubMed]
- 17.Ellis SG, Tamai H, Nobuyoshi M, Kosuga K, Colombo A, Holmes DR, et al. Contemporary percutaneous treatment of unprotected left main coronary stenoses: initial results from a multicenter registry analysis 1994–1996. Circulation 1997; 96:3867–72. [DOI] [PubMed]
- 18.O'Keefe JH Jr, Hartzler GO, Rutherford BD, McConahay DR, Johnson WL, Giorgi LV, Ligon RW. Left main coronary angioplasty: early and late results of 127 acute and elective procedures. Am J Cardiol 1989;64:144–7. [DOI] [PubMed]
- 19.Park SJ, Hong MK, Lee CW, Kim JJ, Song JK, Kang DH, et al. Elective stenting of unprotected left main coronary artery stenosis: effect of debulking before stenting and intravascular ultrasound guidance. J Am Coll Cardiol 2001;38:1054–60. [DOI] [PubMed]
- 20.Keeley EC, Aliabadi D, O'Neill WW, Safian RD. Immediate and long-term results of elective and emergent percutaneous interventions on protected and unprotected severely narrowed left main coronary arteries. Am J Cardiol 1999;83:242–6, A5. [DOI] [PubMed]
- 21.Wong P, Wong V, Tse KK, Chan W, Ko P, Wong CM, et al. A prospective study of elective stenting in unprotected left main coronary disease. Catheter Cardiovasc Interv 1999;46:153–9. [DOI] [PubMed]
- 22.Randomised placebo-controlled and balloon-angioplasty-controlled trial to assess safety of coronary stenting with use of platelet glycoprotein-IIb/IIIa blockade. The EPISTENT Investigators. Evaluation of Platelet IIb/IIIa Inhibitor for Stenting. Lancet 1998;352:87–92. [DOI] [PubMed]


