Abstract
Cardiac herniation and torsion is a rare condition associated with a high mortality rate. We present an unusual case of sudden cardiogenic shock that was caused by torsion and herniation of the heart after an operation for a penetrating cardiac injury. The patient was successfully treated by urgent surgical intervention.
Key words: Heart injuries/diagnosis/surgery; hernia/diagnosis/surgery; iatrogenic disease; pericardium/injuries/surgery; postoperative complications/surgery; pulmonary arteries/surgery; reoperation; torsion; wounds, penetrating/complications
Lung surgery involving pericardiectomy,1 traumatic rupture of the pericardium,2 and congenital pericardial defects3 can lead to cardiac herniation, which is a rare, life-threatening complication. To our knowledge, 2 cases of iatrogenic cardiac herniation have been reported in the literature after cardiac operations; in both instances, diagnoses of the condition were made at autopsy.4,5 We describe an occurrence of iatrogenic cardiac herniation that caused torsion of the main pulmonary artery.
Case Report
In June 2005, a 16-year-old boy underwent surgery at another hospital for a penetrating intracardiac stab wound. On his 1st postoperative day, he underwent reoperation because of massive bleeding (1,500 mL) from a left thoracostomy tube. No focus for the bleeding was discovered. One hour after the reoperation, complete atrioventricular block followed a sudden onset of dyspnea, so a temporary pacemaker was implanted. Transthoracic echocardiography then revealed an obstruction of the pulmonary artery. One day after his initial surgery, the patient was referred to our clinic for open-heart surgery.
The boy was in cardiogenic shock when admitted to our emergency unit. A physical examination revealed dyspnea with a rate of 30 breaths/min, a slightly enlarged liver, and no cardiac murmurs or extra sounds. The patient had attenuated jugular venous pulse waves with a prominent x descent, and his heart rate was 40 beats/min when his temporary pacemaker was deactivated. An electrocardiogram showed widespread ST-segment depression and complete atrioventricular block. With the patient breathing 3 L/min of oxygen, arterial blood-gas analysis revealed a PO2 of 65 mmHg, a PCO2 of 27 mmHg, and a pH of 7.45.
Transthoracic echocardiography showed right atrial and right ventricular dilatation and pulmonary artery obstruction, but no ventricular septal defect. The pulmonary artery systolic pressure was 60 mmHg. Cardiac catheterization revealed a totally occluded left main pulmonary artery branch and a nearly totally occluded right main pulmonary artery branch (Fig. 1).
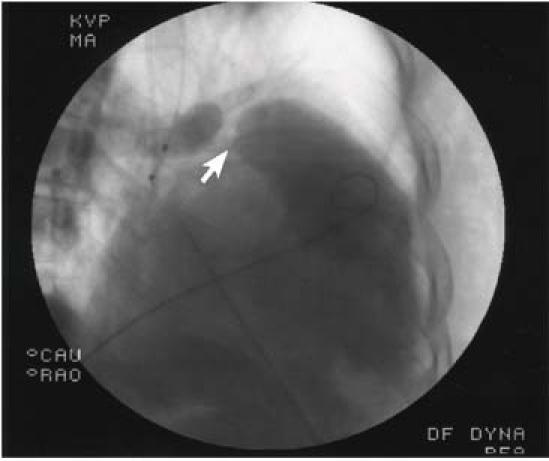
Fig. 1 Preoperative pulmonary angiogram reveals a totally occluded left main pulmonary artery branch and a nearly totally occluded right main pulmonary artery branch (arrow).
As his status worsened, the patient was taken for urgent surgery with a presumptive diagnosis of pulmonary artery embolism. With the patient under general anesthesia, a median sternotomy was performed. The right atrium and ventricle were extremely dilated and stretched. A sutured cardiac injury was visible on the left ventricular wall.
The patient went into sudden cardiac arrest, and cardiopulmonary bypass was instituted by cannulation of the aorta and right atrium during internal cardiac massage. The pericardiotomy incision extended approximately 12 to 13 cm into the left pleuropericardium; this had been left open after the previous operations. Torsion of the main pulmonary artery and herniation of the heart into the left thoracic cavity were evident (Fig. 2). After the ascending aorta was cross-clamped, a longitudinal arteriotomy was performed on the main pulmonary artery. No thrombus was found in the artery or in the main pulmonary branches.
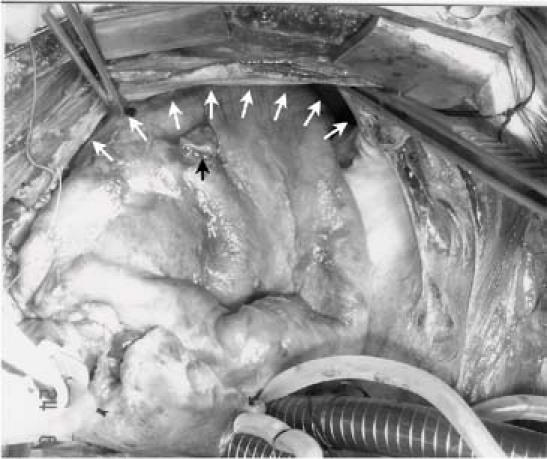
Fig. 2 Intraoperative view of the left hemithorax and the cardiac herniation that twisted the main pulmonary artery. The white arrows point to the pericardial defect in the left pleuropericardium; the black arrow indicates the sutured cardiac injury.
The pericardial defect in the left pleuropericardium was closed by direct suturing without a patch. The heart spontaneously resumed sinus rhythm after the aorta was declamped. Cardiopulmonary bypass was discontinued without any hemodynamic instability, and the right atrial and ventricular dilatation then disappeared.
The patient had an uneventful postoperative recovery. Follow-up pulmonary angiography showed a normal pulmonary arterial system (Fig. 3). The patient was discharged on the 5th postoperative day. Fourteen months later, echocardiography showed normal cardiac function.
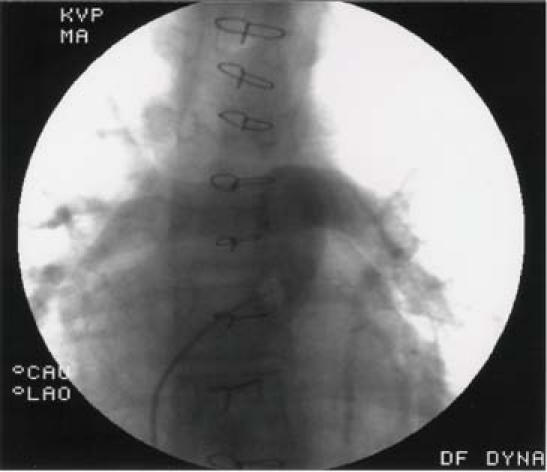
Fig. 3 Postoperative pulmonary angiogram shows normal pulmonary arteries.
Comments
Although herniation of the heart through a pericardial defect is unusual, it should be suspected in certain circumstances. When herniation occurs, sudden cardiogenic shock with signs and symptoms including arrhythmia, myocardial ischemia, and hypotension may develop in a previously stable patient.6
Cardiac herniation after lung surgery that has involved partial pericardiectomy or after blunt traumatic rupture of the pericardium is well described in the literature. The mortality rate from such complications is between 30% and 64%.7,8 Timely diagnosis is very important, and cardiac herniation can be fatal if treatment is delayed.
A high degree of suspicion is required to diagnose cardiac herniation, but surgeons are often unfamiliar with the clinical and radiologic findings. Diagnostic tools include computed tomography, chest radiography, and transthoracic and transesophageal echocardiography,2 although no single imaging technique is entirely reliable. Despite the suggestive clinical, echocardiographic, and angiographic findings, we did not diagnose our patient's condition preoperatively.
On the basis of our experience with our patient, we conclude that iatrogenic cardiac herniation and torsion can occur after cardiac operations in which a lateral pericardiotomy incision has been left open. Cardiac herniation can be treated simply and effectively through primary repair of the pericardial defect with direct suturing or with use of an autologous or synthetic patch. To prevent both cardiac herniation and tamponade by allowing drainage to the pleural cavity, the pleuropericardium should be closed with single sutures spaced 1.5 to 2 cm from each other.
Footnotes
Address for reprints: Gokhan Onem, MD, Department of Cardiovascular Surgery, Pamukkale University Medical Faculty, Kinikli Kampusu, 20070, Denizli, Turkey. E-mail: gonem@pamukkale.edu.tr
References
- 1.Buniva P, Alufi A, Rescigno G, Rademacher J, Nazari S. Cardiac herniation and torsion after partial pericardiectomy during right pneumonectomy. Tex Heart Inst J 2001;28:73. [PMC free article] [PubMed]
- 2.Matsuda S, Hatta T, Kurisu S, Ohyabu H, Koyama T, Kita Y. Traumatic cardiac herniation diagnosed by echocardiography and chest CT scanning: report of a case. Surg Today 1999;29:1221–4. [DOI] [PubMed]
- 3.Funken JC, d'Udekem d'Acoz Y, Noirhomme P. Congenital pericardial defect. Cardiovasc Surg 2002;10:618–9. [DOI] [PubMed]
- 4.Glass JD, McQuillen EN, Hardin NJ. Iatrogenic cardiac herniation: post mortem case. J Trauma 1984;24:632–3. [PubMed]
- 5.Ohshima H, Takeuchi H, Yamaguchi T, Takanashi R, Tsunoda K. Late cardiac strangulation due to an iatrogenic pericardial defect. Chest 1993;104:977–8. [DOI] [PubMed]
- 6.Montero CA, Gimferrer JM, Fita G, Serra M, Catalan M, Canalis E. Unexpected postoperative course after right pneumonectomy. Chest 2000;117:1184–5. [DOI] [PubMed]
- 7.Galindo Gallego M, Lopez-Cambra MJ, Fernandez-Acenero MJ, Alvarez Perez TL, Tadeo Ruiz G, Vazquez Santos P, Ortega Lopez M. Traumatic rupture of the pericardium. Case report and literature review. J Cardiovasc Surg (Torino) 1996;37:187–91. [PubMed]
- 8.Shimizu J, Ishida Y, Hirano Y, Tatsuzawa Y, Kawaura Y, Nozawa A, et al. Cardiac herniation following intrapericardial pneumonectomy with partial pericardiectomy for advanced lung cancer. Ann Thorac Cardiovasc Surg 2003;9:68–72. [PubMed]


