Abstract
Postoperative glucose control directly affects the incidence of deep sternal wound infection and death after patients with diabetes have undergone coronary artery bypass grafting. We compared the effect upon glucose control of continuous insulin infusion with that of glucometer-guided insulin injection after coronary artery bypass.
Our prospective, randomized, controlled study involved patients with diabetes mellitus who underwent coronary artery bypass grafting in our hospital from January 2001 through January 2003. Immediately after surgery, patients were randomly assigned to receive continuous insulin infusion or conventional glucometer-guided injection to maintain blood glucose at a level between 150 and 200 mg/dL. The adequacy of postoperative blood glucose control and clinical outcome were evaluated.
Of 93 patients studied, the incidence of sternal wound infection was 3.9% among infusion patients and 4.8% among injection patients (P=0.587). There was no significant difference in mortality rates (infusion, 3.9%; injection, 2.4%; P=0.573). Satisfactory blood glucose levels were achieved in significantly more patients undergoing infusion than injection (64.7% vs 28.6%, P <0.001). In the injection group, significantly more blood glucose measurements were required to achieve control (23.4 vs 16.5, P=0.001), and good control was attained much sooner in the infusion group (21.4 vs 30.5 hr, P=0.013).
We conclude that continuous insulin infusion provides better control of postoperative blood glucose levels after coronary artery bypass grafting in patients with diabetes than does glucometer-guided insulin injection.
Key words: Blood glucose/analysis; coronary artery bypass/adverse effects; coronary disease/surgery; diabetes complications; diabetes mellitus/drug therapy; dose-response relationship, drug; infusions, intravenous; injections, subcutaneous; insulin/administration & dosage/therapeutic use; treatment outcome
Diabetes mellitus is an important risk factor for coronary artery disease. Patients with diabetes have more advanced, diffuse coronary artery stenosis and more end-organ dysfunction, including renal insuficiency and neurologic deicits.1 They often have serious cardiovascular comorbidities, such as arrhythmias and hypertension. Not infrequently, they suffer sudden cardiac death. Patients with diabetes usually have a worse outcome from acute myocardial infarction and left ventricular dysfunction than do nondiabetic patients2,3 and are more susceptible to perioperative death and shorter long-term survival after coronary artery bypass grafting (CABG).2,4 A higher incidence of postoperative complications has also been reported, including left ventricular dysfunction, sternal infection and need for revision, respiratory insuficiency, perioperative stroke, renal dysfunction, and prolonged intensive care unit (ICU) stay.5–7
Although some common postoperative complications are related to existing comorbid diseases—for instance, vasculopathy and nephropathy—the high incidences of sternal wound infection and operative death are closely related to poor postoperative blood-glucose control. The risks decrease with better control, which is commonly deined as the maintainance of blood glucose levels below 200 mg/dL.8–10 After surgery, the conventional practice in cardiac ICUs is to give glucometer-guided insulin injections every 4 to 6 hours. However, it is dificult to maintain blood glucose levels below 200 mg/dL with this protocol. Postulating that continuous insulin infusion would provide better control of postoperative blood glucose levels, we designed this prospective, randomized study to test that hypothesis. The primary endpoints were incidences of operative mortality and sternal wound infection; the secondary endpoint was the adequacy of blood-glucose control.
Patients and Methods
This study was approved by the Investigational Review Board of our hospital. Informed written consent was obtained from each patient.
From January 2001 through January 2003, we studied 100 consecutive patients with diabetes mellitus who were to undergo CABG for the 1st time. In most cases, the diagnosis of diabetes had been made before admission for surgery. Newly diagnosed diabetes was confirmed by a fasting blood glucose level of ≥200 mg/dL associated with an elevated level of hemoglobin A1c. The CABG was performed with the patients under cardiopulmonary bypass.
The preoperative blood glucose level was recorded as a baseline value, and the intraoperative glucose level was controlled at around 200 mg/dL at the discretion of each anesthesiologist. After surgery and before the immediate postoperative glucose level was measured, the patients were randomly assigned to 1 of 2 groups for diabetic control. The average postoperative glucose level was calculated as the composite average of daily mean glucose levels from the period immediately after surgery through the 5th postoperative day. The mean daily glucose level was defined as the average of blood glucose levels within a 24-hour period. Sternal wound infections, both superficial and deep, were confirmed by wound culture. For each patient, we recorded
Demographic variables: age, sex, weight, and body mass index;
Medical history variables: hypertension, current method of diabetic control, congestive heart failure, renal insufficiency (including renal failure and the type of dialysis), chronic obstructive pulmonary disease, peripheral vascular disease, hyperlipidemia, previous cerebrovascular accident, current and past status as a smoker, and New York Heart Association functional class;
Preoperative cardiovascular variables: left main coronary artery disease, number of diseased vessels, unstable angina, left ventricular dimensions and ejection fraction, previous myocardial infarction, history of atrial ibrillation, cardiogenic shock, percutaneous transluminal angioplasty, preoperative need for inotropic or diuretic agents, and requirement of an intra-aortic balloon pump before undergoing CABG;
Intraoperative variables: operative status, number of anastomoses, graft types, duration of cardiopulmonary bypass, and duration of ischemia (aortic cross-clamp time in traditional CABG or total duration of vessel occlusion in off-pump procedures); and
Postoperative variables: units of blood transfused, reoperation for hemostasis, prolonged intubation, need for inotropic agents, level of cardiac enzymes, new-onset atrial ibrillation, sternal wound infection, new neurologic deicits, renal dysfunction, and death.
Study Groups
Glucometer-Guided Insulin (GGI) Group. Patients in the GGI group received subcutaneous insulin injections (Humulin® R, Eli Lilly and Company; Indianapolis, Ind) every 2 hours in an attempt to maintain blood glucose levels between 150 and 200 mg/dL. The dose of insulin was adjusted on the basis of each patient's response to the previous insulin injection.
When 2 consecutive measurements showed that the target glucose level was attained, the frequency of GGI injections was decreased to once every 4 hours. When the patients began eating, the frequency of injections was changed to 4 times per day (before every meal and at bedtime). Given continuing stability in glucose-level readings, the patient's usual preoperative glucose-control regimen was resumed 5 days after the operation.
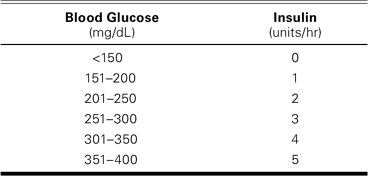
Continuous Insulin Infusion (CII) Group. The CII protocol (see Appendix) used in this group was modiied from the Portland protocol.11 Insulin was initiated and the dosage titrated according to the results of glucose testing to maintain the blood glucose between the desired target levels.
Statistical Analysis
Data were analyzed with the SPSS for Windows Release 11.5 (SPSS Inc.; Chicago, Ill) statistical software package. Continuous variables were compared by means of an unpaired Student's t-test. The mean value of daily blood glucose was compared between the 2 groups by means of Student's t-test and linear regression of repeated measurement. Categorical variables were analyzed by means of a χ2 test with Yates correction. A P value of <0.05 was considered signiicant.
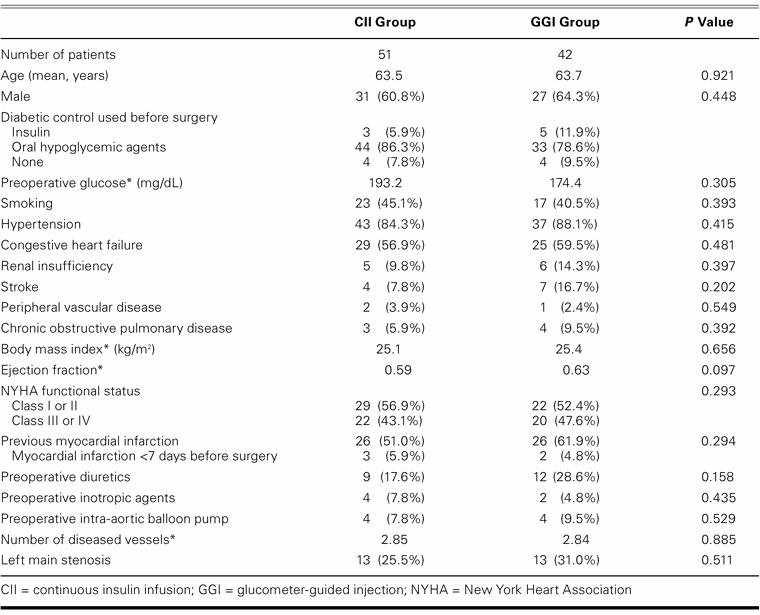
Of the 100 patients enrolled in this study, 51 were randomly assigned to the CII group and 49 to the GGI group. However, 7 patients in the GGI group dropped out of the study after surgery and were switched to the CII regimen because their personal surgeon considered their degree of blood-glucose control to be unacceptable. These 7 were excluded from our analysis. The demographic data of the 2 groups are shown in Table I. There was no signiicant difference between the groups in sex distribution, age, or prevalence of other underlying disease. In both groups, ventricular function and the number of diseased vessels were comparable. Oral hypoglycemic agents were used preoperatively by 43 of 51 CII patients (84%) and by 32 of 42 GGI patients (76%). No glucose control at all had been used by 4 patients in each group (CII, 8%; GGI, 10%) due to diabetes newly diagnosed during admission to our hospital for CABG. The mean preoperative glucose value was 193.2 mg/dL in the CII group and 174.4 mg/dL in the GGI group.
TABLE I. Demographic Data of Patients with Diabetes Who Underwent Coronary Artery Bypass Grafting
Results
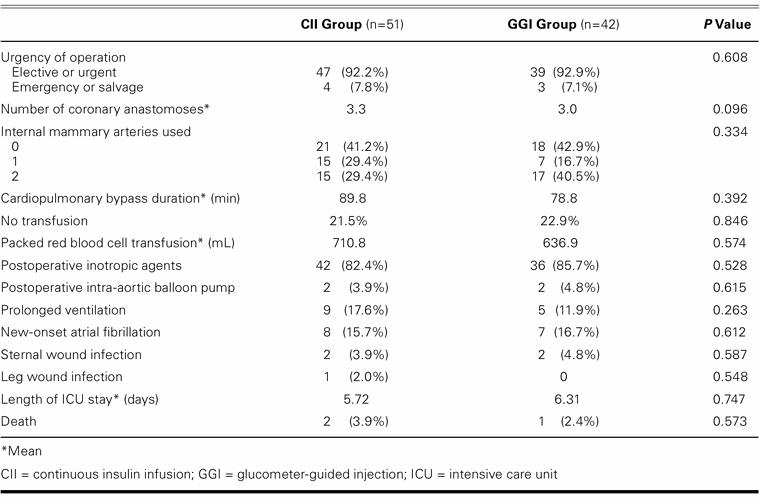
Most of the CABG operations were elective. The mean number of coronary anastomoses was 3.3 in the CII group and 3.0 in the GGI group (P=0.096). All patients underwent traditional cardiopulmonary bypass and cardioplegic cardiac arrest. The duration of bypass varied little between the 2 groups (89.8 vs 78.8 min, P=0.392). Blood transfusion was not required in 11 CII patients (22%) and in 10 GGI patients (24%) (P=0.846); for those in either group who needed blood, the amounts transfused were similar. The percentages of patients requiring postoperative inotropic agents or an intra-aortic balloon pump were similar between groups. Two patients in each group had sternal wound infections requiring débridement and closure (P=0.587). Two CII patients (3.9%) and 1 GGI patient (2.4%) died (P=0.573). The mean length of stay in the ICU was 5.7 days (median, 4 days) for the CII group and 6.3 days (median, 5 days) for the GGI group (P=0.747) (Table II).
TABLE II. Operative Data and Postoperative Complications
Intravenous glucose infusion was discontinued in all patients on the 2nd postoperative day. The daily glucose levels for both groups are shown in Table III. The mean levels were signiicantly higher than baseline levels in the GGI group throughout the postoperative course. In contrast, in the CII group, only on the day of operation was the glucose level signiicantly higher than the baseline value. The mean level on the day of operation was 248.5 mg/dL (CII) versus 233.7 mg/dL (GGI) (P=0.214). On the 1st and 2nd postoperative days, the mean value for the CII group was signiicantly lower than that for the GGI group. Although the levels in the CII group on the subsequent 3 days were lower than those in the GGI group, the differences were not statistically signiicant.
TABLE III. Preoperative and Postoperative Daily Levels of Blood Glucose
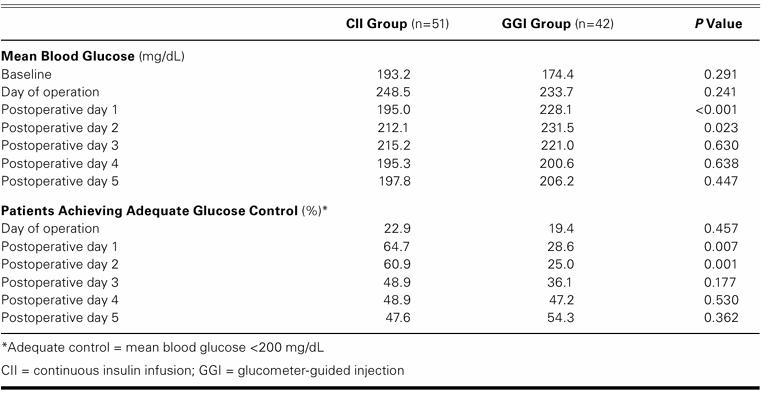
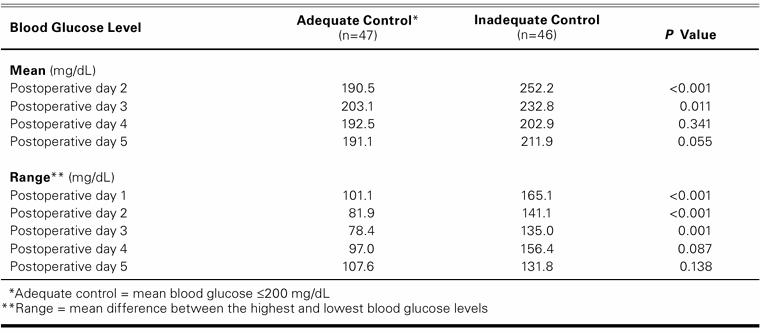
The difference between the curves of daily mean blood-glucose values in each group was signiicant (P=0.045) by the linear regression model. The achievement of glucose control in both groups is shown in Figure 1 In the CII group, blood glucose levels of less than 200 mg/dL were attained in 33 of 51 patients (65%), compared with only 12 of 42 patients (29%) in the GGI group (P <0.001). The morning glucose levels were significantly lower in the CII group (200.2 mg/dL vs 231.4 mg/dL, P=0.046). A blood-glucose reading of less than 200 mg/dL on the 1st postoperative day was associated with better control during subsequent days (Table IV), and the range of glucose change was narrower. The amount of insulin used during the first 2 postoperative days was 152.0 units (CII) versus 106.4 units (GGI) (P=0.062). Blood-glucose tests during the same period were performed 23.4 times in the CII group and 16.5 times in the GGI group (P=0.001). The time required to attain desirable glucose control was signiicantly shorter in the CII group (21.4 vs 30.5 hr, P=0.013).
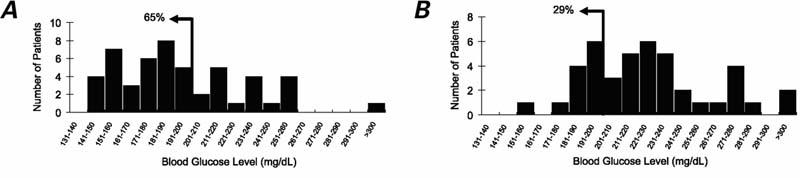
Fig. 1 Distribution curves of mean glucose levels on the 1st postoperative day in the A) CII and B) GGI groups. The arrow represents the desired goal of 200 mg/dL. Adequate blood glucose control was attained in 65% of the patients in the CII group but in only 29% of the patients in the GGI group (P=0.001).
TABLE IV. Adequacy of Blood Glucose Control on Postoperative Day 1 in Relation to Control on Subsequent Days
Discussion
Ours is the 1st prospective, randomized, controlled study to demonstrate signiicantly better blood-glucose control in patients with diabetes by using CII after CABG. Patients treated with CII had a lower mean glucose level and were more likely to achieve the glycemic target than those treated with GGI.
The prevalence of diabetes mellitus in patients undergoing CABG ranges from 15% to 36.7%, with 2 series suggesting that the percentage has increased since 2000.4,6,9,12,13 The reasons for this increase are unclear. In our hospital, approximately half of the patients referred for CABG have a history of diabetes or are newly diagnosed. These patients often experience a more complicated postoperative course and have a higher incidence of postoperative death,4,6,12 sternal wound infection,6,12,14,15 respiratory dysfunction,6 renal dysfunction,6,14,16 neurologic deicit,4 and longer ICU stay.6,16 Associations between hyperglycemia and disordered fatty acid metabolism, and between hyperglycemia and compromised glycolysis in the myocardium, are also reported.17 The detrimental effect of free fatty acids on the ischemic myocardium has been reported to result from increased oxygen consumption, inhibited glucose utilization, decreased myocardial contractility, a predisposition to arrhythmias, and an increase in oxygen free radicals.18 Adequate glycemic control by administration of insulin implies improved glucose uptake by the myocardium, which should provide an energy supply that is more favorable for recovery from intraoperative myocardial ischemia. In addition, insulin stimulates pyruvate dehydrogenase activity and improves aerobic metabolism in postischemic myocardium.19,20 Clinically, perioperative hyperglycemia is associated with increased operative mortality rates,8 deep sternal infection,11 prolonged length of stay in the ICU, and greater consumption of hospital resources.21
The importance of glucose control on the 1st postoperative day has been reported previously. In a retrospective review conducted by McAlister and coworkers,10 an increase of 1 mmol/L (or 18 mg/dL) of glucose on the 1st postoperative day was associated with a 17% increase in the risk of adverse outcomes. Furnary and colleagues11 found a signiicant impact on the risk of postoperative deep sternal infection. Accordingly, reducing glucose levels on the 1st postoperative day may improve the outcomes of patients with diabetes undergoing CABG. In 2003, Furnary's group8 reported that insulin infusion signiicantly reduced mortality rates in these patients. The glucose levels on the day of surgery and the irst 2 days after CABG were signiicant independent predictors of operation-related death, further emphasizing the importance of glucose control in the immediate postoperative period.
With continuous infusion of insulin, we achieved faster achievement of adequate glucose control and a greater ability to maintain postoperative glucose levels near baseline values. Although our CII patients underwent glucose measurements more frequently and required more insulin than did our GGI patients, their overall consumption of hospital resources was not higher, because the closer monitoring of continuous infusions was likely offset by shortened lengths of stay in the ICU and the hospital.
The absence of significant differences in glucose levels in our 2 study groups after the 2nd postoperative day may have been related to an early return to oral feeding, which most patients began during the 1st or 2nd postoperative day. However, the actual food intake varied substantially among the patients, and we were unable to control for this variable. To prevent profound hypoglycemia between meals, we gave intermittent insulin injections instead of a continuous infusion once patients began eating. This limitation of our study appears to hold true for most other such studies, since most have been able to correlate unfavorable outcomes with hyperglycemia only on the 1st postoperative day.10,11
One limitation of our study was the small number of cases, which may explain why we were unable to show a benefit either in better survival or in a reduced incidence of sternal infections. Adverse outcomes and the length of ICU stay were similar in both groups. According to the incidence of death among our patients, an estimated 2,842 patients would be needed in each group to provide a P value of 0.05 with a 90% confidence interval. We did not deem it reasonable to enroll so many patients for study before applying the CII concept.
As a consequence of the study's not being blinded, 7 patients on the GGI protocol were dropped from the treatment protocol because of their physicians' concerns about their high blood-glucose levels. When our secondary goal of better glucose control was reached, we stopped the trial and began using the CII protocol routinely. Although our patients on the CII protocol experienced better control than did those in the GGI group, we were able to reach the target level in only about two thirds of the CII group. Van den Berghe and colleagues22 recommended that the goal of blood-glucose control for patients in the surgical ICU should be no higher than 110 mg/dL. Clearly, we were unable to achieve control that tight with our regimen. How-ever, only 13% of van den Berghe's patients had diabetes, and the researchers measured glucose only in the mornings—a practice insufficient to show that adequate glucose control was maintained in the patients. During the past several decades, Furnary's group8 adjusted the target glucose downward to a level of 100 to 150 mg/dL. They also expanded the application of continuous insulin infusion, initiating it in the operating room and continuing it until the morning of the 3rd postoperative day.8
We conclude that continuous insulin infusion provides better control of postoperative blood-glucose levels in patients with diabetes after CABG than does conventional intermittent injection of insulin. We recommend continuous infusion as the standard treatment for such patients.
Appendix
Insulin for infusion was prepared by diluting 50 units in 50 mL saline.
-
Blood-glucose levels were checked immediately after each patient's arrival in the postoperative intensive care unit. The insulin infusion was started as follows:
-
The frequency of glucose testing was as follows:
Glucose was measured every hour until the target level of 150 to 200 mg/dL was attained in 2 consecutive tests, after which glucose was measured every 2 hours.
If the desired glucose level was maintained for 2 consecutive tests every 2 hours, the frequency of testing was changed to once every 4 hours.
The continuous insulin infusion protocol was stopped and the preoperative glucose-control regimen was resumed when a patient was able to tolerate regular feeding. Glucose measurements were then performed 4 times daily, and glucose levels were controlled as necessary by subcutaneous insulin injections.
-
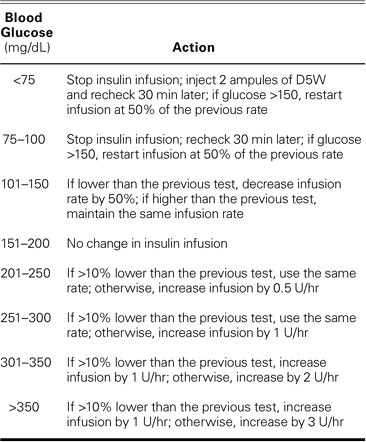
Titration of the insulin infusion:
The intravenous fluids, infused at 1 mL/kg/hr immediately after surgery, included 10 MEq of potassium in each bottle of D5W.
Footnotes
Address for reprints: Jiun-Yi Li, MD, Department of Surgery, Mackay Memorial Hospital, No. 92, Sec. 2, Chung-Shan N. Rd., Taipei 104, Taiwan, ROC. E-mail: JYL5891@ms2.mmh.org.tw
References
- 1.Jessen ME. Glucose control during cardiac surgery: How sweet it is. J Thorac Cardiovasc Surg 2003;125:985–7. [DOI] [PubMed]
- 2.McNally PG, Lawrence IG, Panerai RB, Weston PJ, Thurston H. Sudden death in type 1 diabetes. Diabetes Obes Metab 1999;1:151–8. [DOI] [PubMed]
- 3.Smith JW, Marcus FI, Serokman R. Prognosis of patients with diabetes mellitus after acute myocardial infarction. Am J Cardiol 1984;54:718–21. [DOI] [PubMed]
- 4.Thourani VH, Weintraub WS, Stein B, Gebhart SS, Craver JM, Jones EL, Guyton RA. Influence of diabetes mellitus on early and late outcome after coronary artery bypass grafting. Ann Thorac Surg 1999;67:1045–52. [DOI] [PubMed]
- 5.Sugioka J, Ozawa S, Inagaki M, Fukuzawa S, Daimon M, Kushida S, Tateno K. Influence of diabetes mellitus on left ventricular function in patients undergoing coronary artery bypass grafting. J Cardiol 2000;36:9–16. [PubMed]
- 6.Bucerius J, Gummert JF, Walther T, Doll N, Falk V, Onnasch JF, et al. Impact of diabetes mellitus on cardiac surgery outcome [published erratum appears in Thorac Cardiovasc Surg 2003;51:113]. Thorac Cardiovasc Surg 2003;51:11–6. [DOI] [PubMed]
- 7.Seki S, Yoshida H, Momoki Y, Ooba O, Teramoto S, Komoto Y. Impaired pulmonary oxygenation of diabetic origin in patients undergoing coronary artery bypass grafting. Cardiovasc Surg 1993;1:72–8. [PubMed]
- 8.Furnary AP, Gao G, Grunkemeier GL, Wu Y, Zerr KJ, Bookin SO, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg 2003;125:1007–21. [DOI] [PubMed]
- 9.Zerr KJ, Furnary AP, Grunkemeier GL, Bookin S, Kanhere V, Starr A. Glucose control lowers the risk of wound infection in diabetics after open heart operations. Ann Thorac Surg 1997;63:356–61. [DOI] [PubMed]
- 10.McAlister FA, Man J, Bistritz L, Amad H, Tandon P. Diabetes and coronary artery bypass surgery: an examination of perioperative glycemic control and outcomes. Diabetes Care 2003;26:1518–24. [DOI] [PubMed]
- 11.Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg 1999;67:352–62. [DOI] [PubMed]
- 12.Guvener M, Pasaoglu I, Demircin M, Oc M. Perioperative hyperglycemia is a strong correlate of postoperative infection in type II diabetic patients after coronary artery bypass grafting. Endocr J 2002;49:531–7. [DOI] [PubMed]
- 13.Lindvall B, Brorsson B, Herlitz J, Albertsson P, Werko L. Comparison of diabetic and non-diabetic patients referred for coronary angiography. Int J Cardiol 1999;70:33–42. [DOI] [PubMed]
- 14.Whang W, Bigger JT Jr. Diabetes and outcomes of coronary artery bypass graft surgery in patients with severe left ventricular dysfunction: results from The CABG Patch Trial database. The CABG Patch Trial Investigators and Coordinators [published erratum appears in J Am Coll Cardiol 2001;37:2012]. J Am Coll Cardiol 2000;36:1166–72. [DOI] [PubMed]
- 15.Hirotani T, Kameda T, Kumamoto T, Shirota S, Yamano M. Effects of coronary artery bypass grafting using internal mammary arteries for diabetic patients. J Am Coll Cardiol 1999;34:532–8. [DOI] [PubMed]
- 16.Morricone L, Ranucci M, Denti S, Cazzaniga A, Isgro G, Enrini R, Caviezel F. Diabetes and complications after cardiac surgery: comparison with a non-diabetic population. Acta Diabetol 1999;36:77–84. [DOI] [PubMed]
- 17.Herlitz J, Malmberg K. How to improve the cardiac prognosis for diabetes. Diabetes Care 1999;22 Suppl 2:B89–96. [PubMed]
- 18.Opie LH. Effects of regional ischemia on metabolism of glucose and fatty acids. Relative rates of aerobic and anaerobic energy production during myocardial infarction and comparison with effects of anoxia. Circ Res 1976;38(5 Suppl 1):I52–74. [PubMed]
- 19.Rao V, Merante F, Weisel RD, Shirai T, Ikonomidis JS, Cohen G, et al. Insulin stimulates pyruvate dehydrogenase and protects human ventricular cardiomyocytes from simulated ischemia. J Thorac Cardiovasc Surg 1998;116:485–94. [DOI] [PubMed]
- 20.Lazar HL, Chipkin S, Philippides G, Bao Y, Apstein C. Glucose-insulin-potassium solutions improve outcomes in diabetics who have coronary artery operations. Ann Thorac Surg 2000;70:145–50. [DOI] [PubMed]
- 21.Estrada CA, Young JA, Nifong LW, Chitwood WR Jr. Outcomes and perioperative hyperglycemia in patients with or without diabetes mellitus undergoing coronary artery bypass grafting. Ann Thorac Surg 2003;75:1392–9. [DOI] [PubMed]
- 22.van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001;345:1359–67. [DOI] [PubMed]