Abstract
We describe the case of a 31-year-old man who experienced an acute myocardial infarction 16 years after undergoing radiation and vinca alkaloid therapy for Hodgkin's disease. Even though coronary artery disease is a well-established complication after mediastinal radiation therapy, this adult patient had normal coronary angiographic results, with no traditional risk factors for coronary artery disease, and no hematologic or other abnormality associated with hypercoagulability.
Keywords: Key words, Antineoplastic agents/adverse effects, coronary disease/etiology, electrocardiography, heart/radiation effects, heart diseases/chemically induced/etiology, Hodgkin disease/radiotherapy, myocardial infarction/etiology, radio-therapy/adverse effects, risk assessment, risk factors
Long-term survival after Hodgkin's disease has increased considerably during the past 30 years; therefore, diagnosis and management of late complications after initial treatment of the disease are very important.1 Cardiovascular complications after mediastinal radiotherapy (with or without chemotherapy) include acute pericarditis, late constrictive pericarditis, coronary artery disease (CAD), valvular heart disease, and myocardial fibrosis.2 In particular, several studies have shown an association between mediastinal irradiation and CAD,2 whereas cardiac deaths constitute nearly 5% of all deaths in the Hodgkin's disease population.3,4
We describe the case of a patient who suffered an acute myocardial infarction (MI) 16 years after treatment for Hodgkin's disease. Notably, this adult patient had normal coronary angiographic results, no traditional risk factors for CAD, and no hematologic abnormality associated with hypercoagulability.
Case Report
In November 2003, a 31-year-old man presented at our emergency department with chest discomfort of 2 hours' duration. His medical history included Hodgkin's disease, which had been diagnosed at age 15. He had been treated with mediastinal irradiation followed by vinca alkaloid chemotherapy, and he had since remained asymptomatic, with no evidence of relapse. He was taking no medication and had no traditional risk factors for CAD. An electrocardiogram (ECG) on admission showed ST-segment elevation of 1 mm in the inferior leads (Fig. 1).
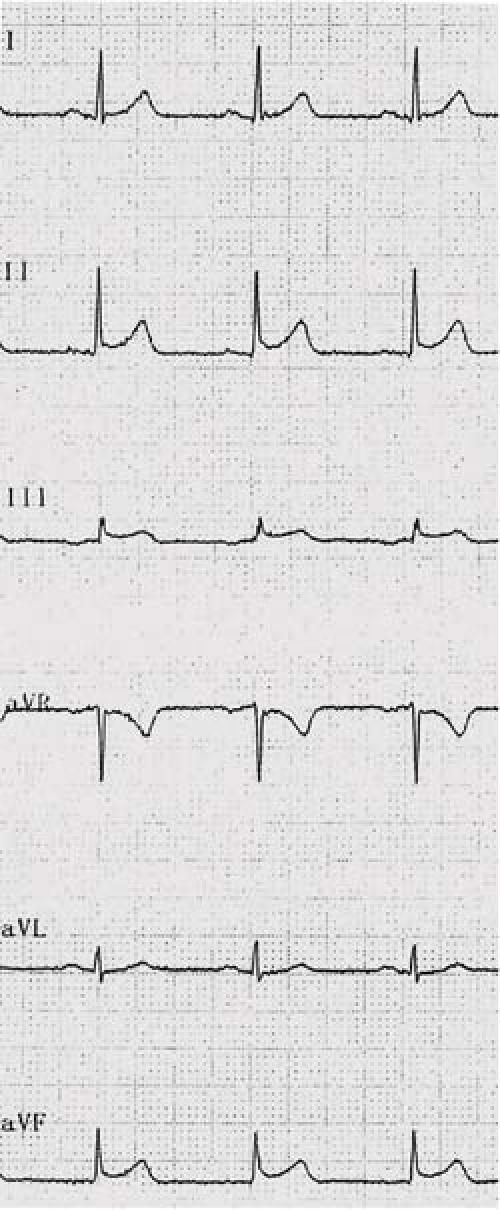
Fig. 1 Electrocardiographic recording on admission shows slight ST-segment elevation in the inferior leads.
The patient was transferred to the coronary care unit. His vital signs were normal. A clinical examination revealed the presence of a 4th heart sound. The symptoms persisted, and he was treated with nitroglycerin, diltiazem, aspirin, and heparin. The symptoms and the ECG abnormalities completely resolved within 1 hour. The next day, an ECG demonstrated biphasic T waves in leads V3 through V5, and the biochemical markers for myocardial damage (troponin T and creatine kinase-MB) were elevated (5 μg/mL and 62 IU/L, respectively), suggesting myocardial necrosis. His lipid profile and thyroid function values were within normal limits. Transthoracic echocardiography performed at bedside revealed mild hypokinesis of the cardiac apex, the basal segment of the interventricular septum, and the inferior wall, with a calculated ejection fraction of 0.55. A chest radiograph showed no abnormality. Results of coronary angiography performed on the 3rd day of hospitalization and of provocative tests for coronary artery spasm were also normal (Fig. 2). The patient had not experienced febrile or inflammatory disease during the previous months, and screening tests for myocarditis (autoantibodies and serological markers for infectious agents) were negative. Also negative, and notably so, were coagulation tests and molecular screening (using samples obtained before treatment) for factor V Leiden, protein C and S deficiencies, prothrombin G20210A, and methylenetetrahydrofolate reductase C677T polymorphisms.
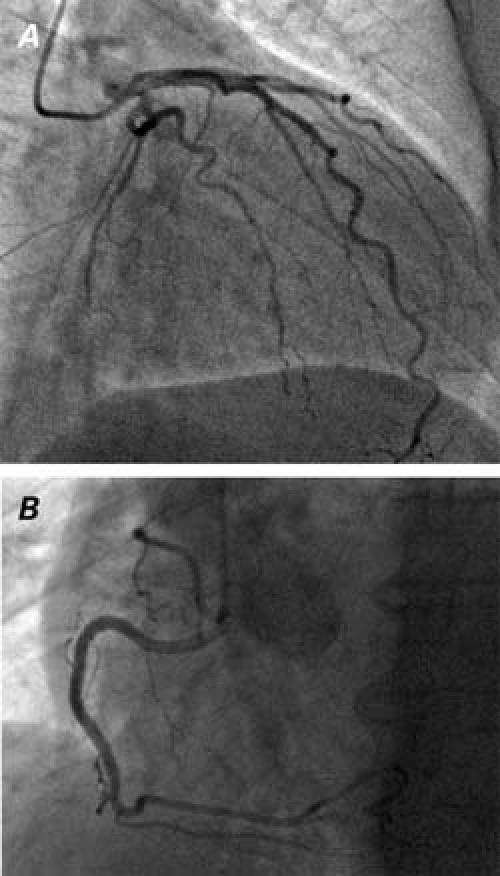
Fig. 2 Angiogram in the A) right anterior oblique caudal view shows a normal left coronary artery, and B) left anterior oblique view shows a normal right coronary artery.
The patient was discharged 7 days after admission on prescribed diltiazem and aspirin. One month later, he performed an exercise stress test successfully, with no evidence of ischemia. The patient remained completely asymptomatic 11 months later.
Discussion
Despite having normal coronary arteries 16 years after the completion of irradiation and chemotherapy for Hodgkin's disease, the patient experienced an acute MI. A vasospastic response during cardiac catheterization could not be elicited in his case; nevertheless, the most plausible underlying mechanism seems to be either transient coronary artery spasm, thrombosis with subsequent spontaneous recanalization, or both.
Advances in cancer treatment increase the likelihood that patients diagnosed with cancer will survive longer now than in the past. Therefore, cardiac damage induced by radiation and chemotherapy is appearing more often, and it is a relevant late side effect of such treatments.5
Mediastinal irradiation and chemotherapy in patients with Hodgkin's disease have been associated with the development of CAD that manifests itself over ensuing years.2,3 A retrospective study of 4,665 patients treated for Hodgkin's disease with either irradiation or chemotherapy identified 124 diagnoses of CAD, including 68 cases of acute MI.3 Long-term follow-up of 27,280 patients after irradiation therapy showed that, after 15 to 20 years, the mortality rate from Hodgkin's disease diagnosed at early and intermediate stages was surpassed by other causes of death, mostly secondary malignancies and cardiac deaths, the latter especially from MI.4
Although the exact pathogenesis of the complication of MI remains largely undetermined, it is believed to be related to endothelial damage and subsequent fibrosis.6,7 In most cases, the classic atherosclerotic process is accelerated and severe focal stenotic lesions become evident, especially in individuals with traditional risk factors for CAD.8,9 Certain cytokines and growth factors, such as TGF-β1 and IL-1β, may stimulate irradiation-induced endothelial proliferation, fibroblast proliferation, collagen deposition, and fibrosis.10 Furthermore, vinca alkaloids have been shown to exert toxic effects on the endothelium.11
To the best of our knowledge, acute MI in the presence of normal coronary arteries, after irradiation therapy for Hodgkin's disease, has been reported only once in the medical literature.12 In that report, a 19-year-old woman developed MI 27 months after radiation therapy. In addition, Scholz and colleagues13 presented a case of acute MI that developed as a result of right coronary artery thrombosis 5 days after the start of vinblastine treatment; in that instance, late coronary angiography revealed normal coronary arteries. Of note is that our patient experienced this MI complication after a far longer time interval than any other patient whose case is reported in the literature.
In fact, there is no empirical evidence regarding preventive strategies for late cardiac complications of irradiation and chemotherapy. When considering the aforementioned pathophysiologic considerations, it is reasonable to assume that the prophylactic use of agents that have favorable effects on the endothelium and on the atherothrombotic process (statins, aspirin, inhibitors of the renin–angiotensin system, and others)14 may prove clinically relevant, especially in patients with concomitant CAD risk factors.
In conclusion, presumptive endothelial dysfunction after irradiation and chemotherapy in survivors of Hodgkin's disease may lead to coronary artery spasm or thrombosis with subsequent spontaneous recanalization, which can cause acute MI in the presence of normal coronary arteries. Clinicians should be aware of this complication in order to make a timely and correct diagnosis, and to aggressively manage coexistent cardiovascular risk factors.
Footnotes
Address for reprints: Panagiotis Korantzopoulos, MD, Department of Cardiology, G. Hatzikosta General Hospital, 45001 Ioannina, Greece. E-mail: pan-kor@mailbox.gr
References
- 1.Abrahamsen AF, Loge JH, Hannisdal E, Nome O, Lund MB, Holte H, Kvaloy S. Late medical sequelae after therapy for supradiaphragmatic Hodgkin's disease. Acta Oncol 1999; 38:511–5. [DOI] [PubMed]
- 2.Glanzmann C, Kaufmann P, Jenni R, Hess OM, Huguenin P. Cardiac risk after mediastinal irradiation for Hodgkin's disease. Radiother Oncol 1998;46:51–62. [DOI] [PubMed]
- 3.Boivin JF, Hutchison GB, Lubin JH, Mauch P. Coronary artery disease mortality in patients treated for Hodgkin's disease. Cancer 1992;69:1241–7. [DOI] [PubMed]
- 4.Gustavsson A, Osterman B, Cavallin-Stahl E. A systematic overview of radiation therapy effects in Hodgkin's lymphoma. Acta Oncol 2003;42:589–604. [DOI] [PubMed]
- 5.Gaya AM, Ashford RF. Cardiac complications of radiation therapy. Clin Oncol (R Coll Radiol) 2005;17:153–9. [DOI] [PubMed]
- 6.Om A, Ellahham S, Vetrovec GW. Radiation-induced coronary artery disease. Am Heart J 1992;124:1598–602. [DOI] [PubMed]
- 7.Brosius FC 3rd, Waller BF, Roberts WC. Radiation heart disease. Analysis of 16 young (aged 15 to 33 years) necropsy patients who received over 3,500 rads to the heart. Am J Med 1981;70:519–30. [DOI] [PubMed]
- 8.Angelini A, Benciolini P, Thiene G. Radiation-induced coronary obstructive atherosclerosis and sudden death in a teenager. Int J Cardiol 1985;9:371–3. [DOI] [PubMed]
- 9.McEniery PT, Dorosti K, Schiavone WA, Pedrick TJ, Sheldon WC. Clinical and angiographic features of coronary artery disease after chest irradiation. Am J Cardiol 1987;60:1020–4. [DOI] [PubMed]
- 10.Basavaraju SR, Easterly CE. Pathophysiological effects of radiation on atherosclerosis development and progression, and the incidence of cardiovascular complications. Med Phys 2002;29:2391–403. [DOI] [PubMed]
- 11.Pai VB, Nahata MC. Cardiotoxicity of chemotherapeutic agents: incidence, treatment and prevention. Drug Saf 2000; 22:263–302. [DOI] [PubMed]
- 12.Yahalom J, Hasin Y, Fuks Z. Acute myocardial infarction with normal coronary arteriogram after mantle field radiation therapy for Hodgkin's disease. Cancer 1983;52:637–41. [DOI] [PubMed]
- 13.Scholz KH, Herrmann C, Tebbe U, Chemnitius JM, Helmchen U, Kreuzer H. Myocardial infarction in young patients with Hodgkin's disease–potential pathogenic role of radiotherapy, chemotherapy, and splenectomy. Clin Investig 1993; 71:57–64. [DOI] [PubMed]
- 14.Viles-Gonzalez JF, Anand SX, Valdiviezo C, Zafar MU, Hutter R, Sanz J, et al. Update in atherothrombotic disease. Mt Sinai J Med 2004;71:197–208. [PubMed]


