Abstract
Gastrointestinal complications after open-heart surgery are rare. Many preoperative, intraoperative, and postoperative factors may predispose patients to these complications or cause them. Our patient was a 64-year-old woman who underwent aortic valve replacement due to aortic stenosis. Free intra-abdominal hemorrhage occurred on the 2nd postoperative day. During exploratory laparotomy, it was determined that the hemorrhage was from a vein near the falciform ligament of the liver and from a bleeding laceration of the splenic capsule. The complication was repaired surgically. To our knowledge, intra-abdominal hemorrhage of both liver and spleen after open-heart surgery has never been reported before, even in large patient series. We report the case and present our ideas regarding the cause of the bleeding.
Key words: Anticoagulants/adverse effects; cardiac surgical procedures/adverse effects; gastrointestinal hemorrhage/etiology; heparin, low-molecularweight/adverse effects; postoperative complications; splenic rupture; rupture, spontaneous
Intra-abdominal complications are rare (0.3%–2.0%) after open-heart surgery.1 However, the mortality rate of patients exposed to these complications is high (11%–59%).2–4 Among the conditions most associated with intra-abdominal complications after open-heart surgery are preoperative factors (impaired left ventricular function, peripheral vascular disease, old age, and female sex), intraoperative occurrences (prolonged cardiopulmonary bypass and aortic cross-clamp time, emergency surgery, and the use of an intra-aortic balloon pump), and postoperative factors (prolonged mechanical ventilation, anticoagulation, valve surgery, acute and chronic renal failure, sepsis, and mediastinitis).1 In this case, we discuss a free intra-abdominal hemorrhage as a sequela to open-heart surgery.
Case Report
In April 2004, a 64-year-old woman was hospitalized to undergo aortic valve replacement. Because of aortic stenosis, the patient had been monitored for 5 years in our cardiology clinic. During the past year, she had been anxious because of dyspnea and stridor. Upon echocardiography, her aortic stenosis was seen to have progressed; the mean systolic gradient was now 55 mmHg. Her medical history was notable for chronic obstructive lung disease of 20 years' duration and for pulmonary tuberculosis (diagnosed and treated in 1996). She had no history of trauma during the past 6 months. The patient consulted specialists in pulmonary disease, who cleared her for the aortic valve surgery. The results of her preoperative coagulation studies were normal. Because there was no evidence of a blood coagulopathy, low-molecular-weight heparin (LMWH) was not given preoperatively.
After a standard median sternotomy, cardiopulmonary bypass was performed with ascending aortic and 2-stage venous cannulation. There were no difficulties during aortocaval cannulation and cardiopulmonary bypass. Cardiac arrest was achieved with blood cardioplegic solution. After aortotomy, it was seen that the aortic valve was highly calcific. Aortic valve replacement was performed with a 23-mm mechanical prosthesis (St. Jude Medical, Inc.; St. Paul, Minn). The aortic cross-clamp time was about 60 minutes. The perioperative transesophageal echocardiogram showed good prosthetic valve function and no paravalvular leak. Two chest tubes were placed, one through the mediastinum and the other through the left pleura. The tube to the mediastinum was made of silicone and was placed below the xiphoid process.
There was no problem on the 1st postoperative day, and the patient was extubated 10 hours after the operation. Low-molecular-weight heparin (dalteparin, 10,000 IU/day) was prescribed for coagulation prophylaxis; the 1st dose was given at the 12th postoperative hour. After extubation, the patient's arterial blood oxygen saturation indicated hypoxia, so bronchodilator and corticosteroid agents were started and postural drainage was performed. The partial thromboplastin time was 58 sec on the 2nd postoperative day.
Forty-eight hours after surgery, sudden hypotension and bradycardia occurred; because of the respiratory disturbance, the patient was intubated. Cardiac arrest then occurred, but sinus rhythm was restored after a short resuscitation period. Just 2 hours before this event, routine testing had shown a hemoglobin level of approximately 10.2 mg/dL. Until that time, the mediastinal tubes had been oscillating, and there had been no significant drainage. Central venous pressure was absent (0 mmHg), and rapid volume replacement (erythrocyte suspension, 4 units; fresh frozen plasma, 6 units) did not re-verse the fall. An urgent complete blood count showed that the patient's hemoglobin level was 5.7 mg/dL.
After all these interventions, the arterial systolic blood pressure was only 60 to 70 mmHg. Transesophageal echocardiography was performed urgently for suspected cardiac tamponade or aortic dissection, but there was no sign of hemorrhage or dissection. Abdominal distention was noticed, so abdominal ultrasonography was performed and general surgeons were consulted. Ultrasonography revealed perihepatic, perisplenic–subcapsular, and peritoneal free fluid, on which basis an urgent laparotomy was performed. Upon laparotomy, 2,500 cc of hemorrhagic fluid was aspirated, and the incision was enlarged. A vein near the falciform ligament of the liver (Fig. 1) was seen to be actively bleeding, and there was a laceration on the spleen capsule. The bleeding vein was ligated and the spleen capsule repaired. The patient's hemodynamic values and mental function were normal after the operation. Unfortunately, her preoperative lung problems and the massive blood transfusion worsened her respiratory function. A tracheotomy was performed, but the patient could not be extubated, and she died 38 days after the 2nd operation due to the respiratory complications.
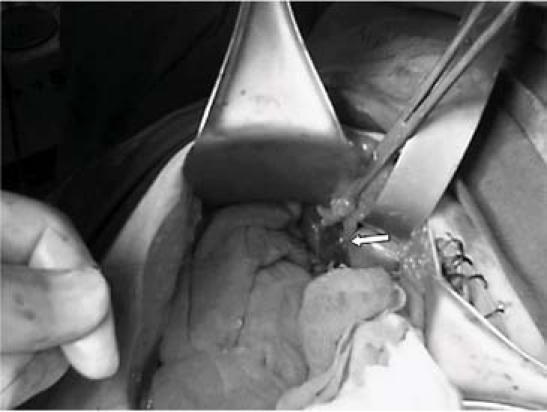
Fig. 1 Arrow shows the bleeding vein near the falciform ligament of the liver.
Discussion
Although gastrointestinal and intra-abdominal complications are rare after open-heart surgery, they increase the mortality rate significantly.1 The most common gastrointestinal complications in large patient series1–3,5 were upper gastrointestinal bleeding, gastroesophagitis, colitis, enteric ischemia, perforated peptic ulcer, and lower gastrointestinal bleeding. To our knowledge, there has been no previous report of intra-abdominal free hemorrhage from the spleen or liver after open-heart surgery.
The most common causes of gastrointestinal complications after open-heart surgery, listed in our introductory remarks, fall within a wide spectrum. Our patient had some of the risk factors. However, these factors generally predispose the patient to enteric ischemia or ulceration, not to rupture of the spleen or the liver. We suspect that 2 other factors—the spontaneous hemorrhagic effect of LMWH,6,7 and perhaps the postural drainage—may have contributed to the bleeding in our patient.
The use of LMWH, which has been reported in patients undergoing open-heart surgery,8 affects coagulation extrinsically by inhibiting factors Xa and IIa. We were using LMWH in our patient for prosthetic valve protection and for prophylaxis of deep venous thrombosis. It has been reported that LMWH can cause spontaneous splenic rupture and intra-abdominal free hemorrhage.6 The efficiency and reliability of LMWH are well known and are comparable to the efficiency and reliability of unfractionated heparin,9 and reported cases of hemorrhage due to LMWH are rare. Nonetheless, there are reports of spontaneous hemorrhage, such as retroperitoneal and intra-abdominal hemorrhage, related to LMWH.10 The literature reports such bleeding episodes at a rate of up to 5.2%.10 The general surgeons' exploration found no congenital aneurysm or arteriovenous malformation in the bleeding zone; and this, we believe, supports our hypothesis in regard to the cause of bleeding.
Another (but somewhat less probable) reason for the bleeding is the blunt-trauma effect of intensive postural drainage on intra-abdominal organs such as the spleen and liver, which could contribute to postoperative intra-abdominal hemorrhage in a patient who has respiratory problems.
In conclusion, intra-abdominal hemorrhage of the spleen or liver is a possible complication of open-heart surgery. Although rare, hepatic or splenic lacerations can occur spontaneously and can contribute to postoperative hemodynamic instability after open-heart surgery. When bleeding of unknown origin occurs, a cardiac surgeon thinks first about the operative zone but should mind the possibility of intra-abdominal bleeding from the spleen or liver in patients who have received LMWH or have been exposed to postural drainage.
Footnotes
Address for reprints: Erkan Iriz, MD, Gazi Universitesi Tip Fakultesi Kalp ve Damar Cerrahisi AD, Besevler 06500 Ankara, Turkey. E-mail: erkaniriz@hotmail.com
References
- 1.D'Ancona G, Baillot R, Poirier B, Dagenais F, de Ibarra JI, Bauset R, et al. Determinants of gastrointestinal complications in cardiac surgery. Tex Heart Inst J 2003;30:280–5. [PMC free article] [PubMed]
- 2.Zacharias A, Schwann TA, Parenteau GL, Riordan CJ, Durham SJ, Engoren M, et al. Predictors of gastrointestinal complications in cardiac surgery. Tex Heart Inst J 2000;27:93–9. [PMC free article] [PubMed]
- 3.Christenson JT, Schmuziger M, Maurice J, Simonet F, Velebit V. Gastrointestinal complications after coronary artery bypass grafting. J Thorac Cardiovasc Surg 1994;108:899–906. [PubMed]
- 4.Ohri SK, Desai JB, Gaer JA, Roussak JB, Hashemi M, Smith PL, Taylor KM. Intra-abdominal complications after cardiopulmonary bypass. Ann Thorac Surg 1991;52:826–31. [DOI] [PubMed]
- 5.Yilmaz AT, Arslan M, Demirkilc U, Ozal E, Kuralay E, Bingol H, et al. Gastrointestinal complications after cardiac surgery. Eur J Cardiothorac Surg 1996;10:763–7. [DOI] [PubMed]
- 6.Taccone FS, Starc JM, Sculier JP. Splenic spontaneous rupture (SSR) and hemoperitoneum associated with low molecular weight heparin: a case report. Support Care Cancer 2003;11:336–8. [DOI] [PubMed]
- 7.Burg MD, Dallara JJ. Rupture of a previously normal spleen in association with enoxaparin: An unusual cause of shock. J Emerg Med 2001;20:349–52. [DOI] [PubMed]
- 8.Beghi C, Fragnito C, Antonelli A, Reverberi C, Ferrari P, Saccani S, Fesani F. Prevention of deep venous thrombosis by a new low molecular weight heparin (Fluxum) in cardiac surgery. Int Angiol 1993;12:383–6. [PubMed]
- 9.Simonneau G, Sors H, Charbonnier B, Page Y, Laaban JP, Azarian R, et al. A comparison of low-molecular-weight heparin with unfractionated heparin for acute pulmonary embolism. The THESEE Study Group. Tinzaparine ou Heparine Standard: Evaluations dans l'Embolie Pulmonaire. N Engl J Med 1997;337:663–9. [DOI] [PubMed]
- 10.Melde SL. Enoxaparin-induced retroperitoneal hematoma. Ann Pharmacother 2003;37:822–4. [DOI] [PubMed]


