Abstract
Objectives
The main objectives of this study were to assess the motives, diversion sources and routes of administration associated with the nonmedical use of prescription opioids as well as to examine substance use related problems associated with the nonmedical use of prescription opioids.
Method
A self-administered, cross-sectional Web survey was conducted in 2005 at a large public Midwestern 4-year university in the U.S. using a probability-based sampling approach. The final sample included 4580 full-time undergraduate students.
Results
The three most common motives associated with the nonmedical use of prescription opioids were to relieve pain, get high, and experiment. The leading sources of prescription opioids were friends and parents although there were gender differences in reports of primary sources. More than 1 in every 10 nonmedical users reported intranasal administration. Multivariate analyses indicated nonmedical users of prescription opioids who used for motives other than to relieve pain, obtained these drugs from non-parental sources, or used these drugs via non-oral routes of administration were significantly more likely to experience substance use related problems.
Conclusions
These results indicate that nonmedical use of prescription opioids represents a considerable problem for particular subgroups of college students. While additional research is needed, the present study offers important new directions for policy and research regarding prescription opioid misuse.
Keywords: Prescription opioids, Route of administration, Motives, Diversion, College students, Substance abuse
1. Introduction
The nonmedical use of prescription opioids among college students has increased over the past decade in the U.S. (e.g., Johnston, O'Malley, Bachman, & Schulenberg, 2005a; Mohler-Kuo, Lee, & Wechsler, 2003) and previous studies indicate several potential severe consequences associated with the nonmedical use of prescription opioids (e.g., Cone et al., 2004; Jewers et al., 2005; Katz & Hays, 2004; SAMHSA, 2004; Watson et al., 2004). Despite the possible deleterious effects associated with the nonmedical use of prescription opioids, there is a paucity of studies regarding the motives, sources of diversion, and routes of administration associated with the nonmedical use of these medications among college-age youth (Compton & Volkow, 2006; Zacny et al., 2003).
Undeniably, prescription opioids are the foundation for the treatment of moderate to severe pain within young adults, but this age group also has the highest prevalence rate of nonmedical use of prescription opioids in the U.S (SAMHSA, 2005a). Previous exploratory studies have identified parents and peers as possible sources for abusable prescription drugs obtained without a prescription by adolescents and young adults (Boyd, McCabe, & Teter, 2006; McCabe, Teter, & Boyd, 2005a; Pedersen & Lavik, 1991). However, there has been relatively little epidemiological work examining how college-age youth obtain prescription opioids not prescribed to them and scant research regarding the motives underlying nonmedical use.
The main objectives of the present study were to use a probability-based sample of college students to 1) assess the motives, sources, and routes of administration associated with the nonmedical use of prescription opioids; and 2) examine several measures of drug use and drug use related problems as a function of motive, source, and route of administration associated with the nonmedical use of prescription opioids.
2. Methods
2.1. Study design
After receiving Institutional Review Board approval, this study was conducted in January and February of 2005, drawing on a total undergraduate population of 20,138 full-time students (10,339 women and 9799 men) attending a large public research university located in the U.S. A simple random sample of 5389 full-time undergraduate students was drawn from the total undergraduate population. An additional 652 Hispanic, 634 African-American and 244 Asian undergraduate students were selected using stratified random sampling to ensure adequate representation of these racial/ethnic groups. The entire sample was mailed a pre-notification letter with $2 enclosed describing the study and inviting students to self-administer a Web survey by using a URL address and unique password. Informed consent was obtained online from each participant. Non-respondents were sent up to three reminder e-mails. The Web survey was maintained on an Internet site running under the secure socket layer protocol to ensure privacy and security. By participating in the survey, students became eligible for a sweepstakes that included cash and other prizes. The final response rate was 66.2% and the completion rate was 97%. Nonresponse bias was assessed by administering a short form of the questionnaire via telephone to a randomly selected sample of 750 students who did not respond to the original Web survey, and 159 students responded. The demographic characteristics of the 159 students who responded to the telephone survey were compared with the 591 nonrespondents; there were no significant differences in terms of gender, race, age, and class year between these two groups. When the 159 students surveyed by telephone were compared to the general sample, there were no significant differences in prevalence rates of 12-month alcohol use, binge drinking, 30-day cigarette smoking, and other problem health behaviors.
2.2. Sample
The final sample consisted of 4580 undergraduate students (3639 from simple random sampling and 941 from stratified random sampling). A sample weight was created to account for the sampling design and oversampling of racial minorities and data were weighted for analyses of the overall sample to increase the representativeness of the results. The weight variable was centered (normalized) to ensure the sample size remained the same after weighting. As a result, the demographic characteristics of our sample mirrored the overall student population. The sample consisted of 50% women, 50% men, 65% White, 13% Asian, 7% African American, 5% Hispanic, and 10% from other ethnic categories. The mean age of students in the sample was 19.9 years old (S.D.=2.0). Ninety-eight percent of respondents were 18 to 24 years of age; 28% were freshmen, 24% sophomores, 23% juniors and 25% seniors.
2.3. Measures
Nonmedical use of prescription opioids was assessed with the following question: "On how many occasions in (a) your lifetime or (b) the past 12 months have you used the following types of drugs, not prescribed to you?" Pain medication (i.e., opioids such as Vicodin, OxyContin, Tylenol 3 with codeine, Percocet, Darvocet, morphine, hydrocodone, oxycodone). The response scale ranged from (1) No occasions to (7) 40 or more occasions. Respondents who reported nonmedical use of prescription opioids in the past 12 months were asked if they had used the following prescription drugs not prescribed to them in the past 12 months: (a) Codeine (e.g., Tylenol 3 with codeine), (b) Fentanyl (e.g., Actiq, Duragesic, Sublimaze), (c) Hydrocodone (e.g., Vicodin, Lortab, Lorcet), (d) Hydromorphone (e.g., Dilaudid), (e) Meperidine (e.g., Demerol), (f) Methadone, (g) Morphine, (h) Oxycodone (e.g., OxyContin, Roxicodone, Percocet, Tylox, Percodan), (i) Propoxyphene (e.g., Darvon, Darvocet), (j) Tramadol (e.g. Ultram), (k) Other (specify), (l) Don't know names of some I have used, and (m) Rather not say.
Motives for nonmedical use of prescription opioids were assessed by asking respondents who reported lifetime nonmedical use of prescription opioids the following question: "Please provide the reason(s) why you used pain medication not prescribed to you." Respondents were asked to select all that apply from a list of motives (see Table 1) based on previous research (Johnston & O'Malley, 1986; McCabe et al., 2005a).
Table 1.
Motive, source and route of administration for nonmedical use of prescription opioids
| Overall sample (n=4478) % | Lifetime nonmedical users (n=640) % | Female nonmedical users (n=321) % | Male nonmedical users (n=319) % | Gender differences χ2 (df) p-value | |
|---|---|---|---|---|---|
| Motive | |||||
| Because it relieves pain | 9.0 | 63.0 | 65.7 | 60.2 | NS |
| Because it gives me a high | 4.6 | 31.9 | 24.4 | 39.4 | 16.5 (1)*** |
| Because of experimentation | 3.8 | 26.8 | 18.4 | 35.3 | 23.0 (1)*** |
| Because it helps me sleep | 2.0 | 13.7 | 12.9 | 14.5 | NS |
| Because it helps decrease anxiety | 1.4 | 9.5 | 10.2 | 8.8 | NS |
| Because it's safer than street drugs | 0.5 | 3.6 | 1.9 | 5.2 | 5.0 (1)* |
| Because it counteracts the effects of other drugs | 0.3 | 2.2 | 1.1 | 3.4 | 4.0 (1)* |
| Because I'm addicted | 0.1 | 0.5 | 0.2 | 0.8 | NS |
| Source | |||||
| Friend not from same college | 4.8 | 33.7 | 26.1 | 41.4 | 16.4 (1)*** |
| Parent | 4.0 | 28.3 | 36.1 | 20.4 | 19.1 (1)*** |
| Friend from same college | 3.9 | 27.0 | 24.9 | 29.0 | NS |
| Roommate | 1.1 | 8.0 | 7.8 | 8.2 | NS |
| Boyfriend/girlfriend | 1.1 | 7.9 | 10.0 | 5.8 | NS |
| Acquaintance not from same college | 0.9 | 6.6 | 5.7 | 7.5 | NS |
| Sibling | 0.8 | 5.9 | 7.3 | 4.5 | NS |
| Acquaintance from same college | 0.5 | 3.8 | 2.5 | 5.1 | NS |
| Other family member | 0.5 | 3.6 | 4.0 | 3.1 | NS |
| Drug dealer | 0.5 | 3.5 | 0.9 | 6.1 | 13.1 (1)*** |
| Other | 0.4 | 3.1 | 2.5 | 3.6 | NS |
| Aunt/Uncle | 0.3 | 2.1 | 1.8 | 2.4 | NS |
| Abroad | 0.1 | 1.0 | 1.1 | 0.9 | NS |
| Internet | <0.1 | 0.2 | 0.4 | 0.0 | NS |
| Route of administration | |||||
| Orally | 13.9 | 97.2 | 97.9 | 96.4 | NS |
| Snorting | 1.9 | 13.1 | 10.5 | 15.7 | NS |
| Smoking | 0.6 | 3.9 | 3.1 | 4.8 | NS |
| Inhaling | 0.1 | 0.6 | 0.7 | 0.6 | NS |
| Injecting | 0.1 | 0.5 | 1.0 | 0.0 | NS |
p<0.05,
p<0.001.
Totals exceed 100% because response categories were "select all that apply."
Sources of prescription opioids were assessed by asking respondents who reported lifetime nonmedical use of prescription opioids the following question: "Please indicate who you obtained pain medication from that was not prescribed to you by a doctor." Respondents were asked to select all that apply from a list of sources (see Table 1) based on previous research (McCabe & Boyd, 2005; McCabe et al., 2005a).
Routes of administration were assessed by asking respondents who reported lifetime nonmedical use of prescription opioids to indicate the route(s) of administration they used for taking prescription opioids not prescribed to them by a doctor. Respondents were asked to select all that apply from a list of routes (see Table 1).
Past month use of marijuana and other drugs–including cocaine, LSD, psychedelics other than LSD, heroin, crystal methamphetamine, inhalants and ecstasy–was measured with the following question for each substance: "On how many occasions in the past 30 days have you used the following types of drugs?" The response scale for each substance was (1) no occasions to (7) 40 or more occasions. The use of any of the eight substances in the past month was summed to create an index of past month illicit drug use.
The Drug Abuse Screening Test (DAST-10) is a self-report instrument that can be used in clinical and non-clinical settings to screen for potential abuse of a wide variety of substances other than alcohol (Skinner, 1982). Respondents who used drugs other than alcohol in the past 12 months were asked whether they had experienced 10 drug use related problems in the past 12 months (e.g., inability to stop using drugs, simultaneous polydrug use, illegal activities to obtain drugs, blackouts as a result of drug use, medical problems as a result of drug use, withdrawal symptoms, felt bad or guilty about drug use, family complaints about drug use). Based on previous research, if a respondent indicated that they had experienced three or more drug use related problems, this was considered a "positive" screening test result denoting potential drug abuse or dependence (Cocco & Carey, 1998; French, Roebuck, McGeary, Chitwood, & McCoy, 2001; Maisto, Carey, Carey, Gordon, & Gleason, 2000; Skinner, 1982).
Binge drinking was measured using the following single item question: "Over the past 2 weeks, how many occasions have you had five or more drinks in a row (four or more for women)?" The response scale ranged from (1) none to (6) 10 or more occasions (Wechsler, Dowdall, Davenport, & Rimm, 1995).
The CAGE is a standard four-item brief screening instrument used to identify potential alcohol abuse and dependence (Ewing, 1984; Mayfield, McLeod, & Hall, 1974). Respondents who used alcohol were asked how many times in the past year they had experienced each of the four CAGE criteria (i.e., felt that you should cut down your drinking, been annoyed by people criticizing your drinking, felt guilt or remorse after drinking, had a drink first thing in the morning as an "eye opener"). Consistent with previous college-based research, if a respondent indicated that they had experienced two or more of these events, this was considered a "positive" screening test result denoting potential alcohol abuse (Heck, 1991).
2.4. Data analysis
Prevalence rates of motives, sources, and routes associated with the nonmedical use of prescription opioids were derived by dividing the number of students reporting an outcome behavior by the total number of respondents to that question. Bivariate associations between student characteristics and outcome prevalence rates were tested using chi-square analyses for dichotomous outcomes. In addition, one-way analyses of variance (ANOVA) and post hoc pairwise comparisons using Tukey's Honestly Significant Difference (HSD) test were conducted for continuous outcomes. Multiple logistic regression analyses were conducted to examine the associations between student characteristics and the dichotomous drug use outcomes after statistically controlling for demographic characteristics (e.g., gender, race, class year and living arrangement). Adjusted odds ratios (AOR) and 95% confidence intervals (95% CI) were reported. All statistical analyses were performed using SAS version 9.1.3 (SAS Institute, Cary, NC) statistical software.
3. Results
3.1. Prevalence of nonmedical use of prescription opioids
The lifetime prevalence of nonmedical use of prescription opioids was 14.3% and the past-year prevalence of nonmedical use was 7.5%. Bivariate and multivariate results indicated there were no gender differences in the lifetime or past year nonmedical use of prescription opioids. Bivariate and multivariate results indicated White students were more likely than African-American and Asian students to report lifetime or past year nonmedical use of prescription opioids. Furthermore, seniors were more likely to report lifetime or past year nonmedical use of prescription opioids when compared to freshmen and sophomores. Of the 640 undergraduate students who reported lifetime nonmedical use of prescription opioids, 54.8% used on 1 to 2 occasions, 19.8% used on 3 to 5 occasions, 9.4% used on 6 to 9 occasions and 16.0% used on 10 or more occasions. Further, 62.7% initiated before college and 37.3% initiated during college. Of the 335 past year nonmedical users, the prescription opioids most commonly used included hydrocodone (50%), codeine (38%), oxycodone (14%), and propoxyphene (10%). The past-year prevalence of the following prescription opioids among nonmedical users was 2% or less: morphine, hydromorphone, methadone, fentanyl, meperidine, and tramadol.
3.2. Motives for nonmedical use of prescription opioids
As illustrated in Table 1, respondents were most likely to report "to relieve pain" as a reason for using prescription opioids not prescribed to them by a doctor. Other prevalent motives included "gives me a high" and "experimentation". The rank order for motives for use was the same between lifetime and past year users. Approximately 40% of lifetime nonmedical users reported using prescription opioids to relieve pain only while 60% reported some other combination of motives. Among lifetime users, multiple logistic regression analyses adjusting for gender, class year, race/ethnicity, and living arrangement revealed undergraduate men were about two times more likely than women to report lifetime nonmedical use of prescription opioids to get high (AOR=2.0, 95% CI=1.4–2.9, p<0.001) and to experiment (AOR=2.3, 95% CI=1.6–3.5, p<0.001). These same gender differences in motives were also present for past year users based on bivariate and multivariate results.
As illustrated in Table 2, multiple logistic regression analysis revealed that the likelihood of binge drinking and alcohol problems (based on the CAGE) did not differ between nonmedical users of prescription opioids who reported using these drugs to relieve pain as compared to students who did not report nonmedical use of prescription opioids. In contrast, the odds of binge drinking and alcohol problems (based on the CAGE) were over two times greater among undergraduate students who used prescription opioids for motives other than to relieve pain as compared with students who did not report nonmedical use of prescription opioids.
Table 2.
Substance use and substance-related problems as a function of motive of nonmedical use of prescription opioids
| Motive | Binge drinking in the past 2 weeks
|
CAGE (+ screen) in the past year a |
Marijuana and other illicit drug use in the past month b |
DAST-10 (+ screen) in the past year c |
||||
|---|---|---|---|---|---|---|---|---|
| % | AOR d (95% CI) | % | AOR d (95% CI) | % | AOR d (95% CI) | % | AOR d (95% CI) | |
| No nonmedical use (n=3859) | 50.2 | Ref | 18.4 | Ref | 16.1 | Ref | 5.7 | Ref |
| Relieve pain only (n=252) | 55.6 | 1.2 (0.89–1.60) | 23.4 | 1.3 (0.97–1.88) | 21.5 | 1.4 (1.00–2.02)* | 8.3 | 1.5 (0.86–2.46) |
| Other motives (n=380) | 79.0 | 3.4 (2.60–4.50)*** | 34.5 | 2.2 (1.71–2.82)*** | 59.8 | 7.7 (5.96–9.83)*** | 48.0 | 15.1 (11.46–19.84)*** |
Ref=Reference group for each model was respondents who did not report nonmedical use of prescription opioids.
p<0.05,
p<0.001.
A cutpoint score of two or more was used for the CAGE.
Consisted of any use of the following drugs in the past month: marijuana, cocaine, LSD, other psychedelics, ecstasy, inhalants, heroin or crystal methamphetamines.
A cutpoint score of three or more was used for the DAST-10.
Adjusted odds ratios (AOR) are adjusted for gender, race/ethnicity, class year and living arrangement (odds ratios for these variables are not shown).
As illustrated in Table 2, the likelihood of illicit drug use in the past month was slightly higher for nonmedical users of prescription opioids who reported using prescription opioids to relieve pain as compared to students who did not report nonmedical use of prescription opioids. However, nonmedical users of prescription opioids who used these drugs to relieve pain as their sole motive did not differ from students who did not report nonmedical use of prescription opioids in the odds of experiencing three or more drug use related problems in the past year. In contrast, nonmedical users of prescription opioids who reported motives other than to relieve pain had seven times the odds of using illicit drugs in the past month (AOR=7.7, 95% CI=6.0–9.8, p<0.001) and fifteen times the odds of experiencing three or more drug use related problems in the past year (AOR=15.1, 95% CI=11.5–19.9; p<0.001) as compared to students who did not report nonmedical use of prescription opioids.
To further examine drug use related problems as a function of motive of nonmedical use of prescription opioids, a one-way ANOVAwas conducted. Results indicated a main effect of motive, F(2, 4466)=585.8, p<0.001, and post-hoc tests revealed the mean DAST-10 scores among students who did not report nonmedical use of prescription opioids and individuals who used prescription opioids to relieve pain only were significantly lower than mean DAST-10 scores of nonmedical users who reported motives other than to relieve pain (see Fig. 1).
Fig. 1.
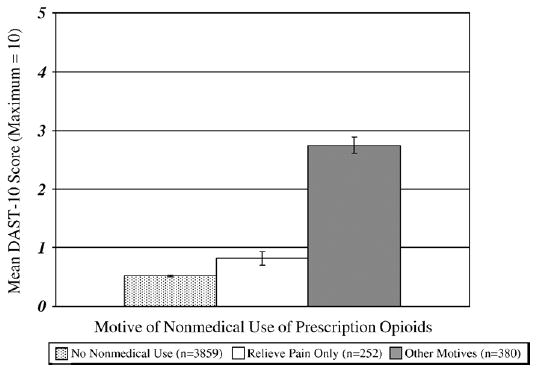
Mean DAST-10 scores as a function of motive of nonmedical use of prescription opioids. Error bars represent ± 1 S.E. ANOVA showed a main effect of motive, F(2, 4466)=585.8, p<0.001. Post-hoc Tukey HSD tests indicated the mean DAST-10 scores among non-users and nonmedical users to relieve pain only were significantly lower than mean DAST-10 scores of nonmedical users who reported motives other than to relieve pain (p<0.05).
3.3. Sources of prescription opioids for nonmedical use
Among the 640 lifetime nonmedical users, 74.8% reported one source for obtaining the drug not prescribed to them, 16.2% indicated two sources, and 9.0% reported three or more sources. As illustrated in Table 1, the leading sources of prescription opioids reported by nonmedical users were friends and parents. Other less prevalent sources included roommates, boyfriend or girlfriend, acquaintances, siblings, other family members, and drug dealers. Notably, the source with the lowest prevalence was obtaining prescription opioids via the Internet (0.2%). There were some important gender differences in the sources of prescription opioids among nonmedical users. Most notably, parents served as the leading single source of prescription opioids for women while friends not from the same university represented the leading single source for undergraduate men. The same rank order and gender differences held true for past year nonmedical users.
Approximately 40.9% of nonmedical users reported peer only sources (e.g., friend/acquaintance from same university, friend/acquaintance not from same university, boyfriend/girlfriend or roommate), 19.7% of nonmedical users reported parent only sources and 39.5% reported some other combination of sources. As illustrated in Table 3, alcohol and other drug use behaviors did not differ between nonmedical users who obtained prescription opioids from their parents and students who did not report nonmedical use of prescription opioids. In contrast, the odds of binge drinking, alcohol problems (based on the CAGE), illicit drug use, and drug use related problems (based on the DAST-10) were significantly greater among nonmedical users who obtained prescription opioids from peer only sources and other non-parental sources as compared to students who did not report nonmedical use of prescription opioids.
Table 3.
Substance use and substance-related problems as a function of source of nonmedical prescription opioids
| Source | Binge drinking in the past 2 weeks
|
CAGE (+ screen) in the past year a |
Marijuana and other illicit drug use in the past month b |
DAST-10 (+ screen) in the past year c |
||||
|---|---|---|---|---|---|---|---|---|
| % | AOR d (95% CI) | % | AOR d (95% CI) | % | AOR d (95% CI) | % | AOR d (95% CI) | |
| No nonmedical use (n=3859) | 50.2 | Ref | 18.3 | Ref | 16.1 | Ref | 5.7 | Ref |
| Parent only (n=126) | 45.2 | 0.7 (0.46–1.06) | 16.7 | 0.8 (0.51–1.39) | 17.5 | 1.0 (0.63–1.72) | 7.9 | 1.3 (0.65–2.68) |
| Peer only (n=259) | 82.6 | 4.4 (3.12–6.32)*** | 34.7 | 2.3 (1.67–3.05)*** | 52.7 | 5.7 (4.23–7.59)*** | 38.5 | 9.9 (7.20–13.68)*** |
| Other sources (n=253) | 68.7 | 2.1 (1.58–2.87)*** | 32.1 | 2.1 (1.55–2.83)*** | 51.2 | 5.6 (4.20–7.53)*** | 39.7 | 11.3 (8.18–15.54)*** |
Ref=Reference group for each model was respondents who did not report nonmedical use of prescription opioids.
p<0.001.
A cutpoint score of two or more was used for the CAGE.
Consisted of any use of the following drugs in the past month: marijuana, cocaine, LSD, other psychedelics, ecstasy, inhalants, heroin or crystal methamphetamines.
A cutpoint score of three or more was used for the DAST-10.
Adjusted odds ratios (AOR) are adjusted for gender, race/ethnicity, class year and living arrangement (odds ratios for these variables are not shown).
ANOVA showed a main effect for source, F(3, 4473)=314.8, p<0.001, and post-hoc tests indicated the mean DAST-10 scores among nonmedical users who obtained prescription opioids from peers only and other sources were significantly higher than non-users and nonmedical users who obtained prescription opioids from their parents only (see Fig. 2). In addition, based on chi-square analyses, motives differed as a function of source. For example, students who obtained prescription opioids from their parents were significantly less likely than their peers who obtained prescription opioids from other sources to use these drugs to get high (8.7% vs. 37.5%, χ2 =38.3, df=1, p<0.001) or for experimentation (4.8% vs. 32.2%, χ2 =37.7, df=1, p<0.001).
Fig. 2.
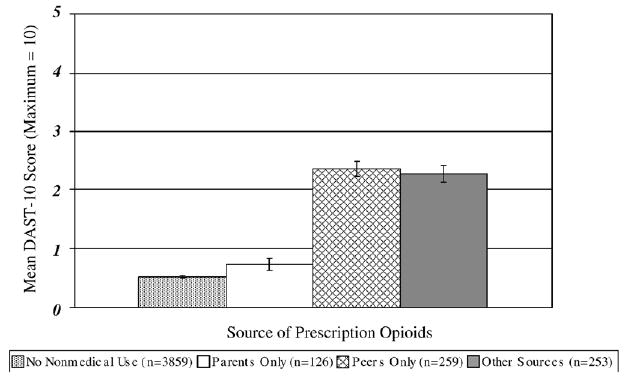
Mean DAST-10 scores as a function of source of nonmedical prescription opioids. Error bars represent ± 1 S.E. ANOVA showed a main effect for source, F(3, 4473)=314.8, p<0.001. Post-hoc tests indicated the mean DAST-10 scores among nonmedical users who obtained prescription opioids from peers only and other sources were significantly higher than non-users and nonmedical users who obtained prescription opioids from their parents only (p<0.05).
3.4. Route of administration for nonmedical use of prescription opioids
As illustrated in Table 1, the two leading routes of administration were oral (97%) and intranasal (13%); intranasal administration of prescription opioids varied as a function of source and motive for nonmedical use. For example, no students (0%) who obtained prescription opioids from their parents reported intranasal administration of prescription opioids as compared to intranasal use by 16.3% of students who obtained these drugs from non-parental sources (χ2 =32.4, df=1, p<0.001). In addition, less than 1% of the individuals who used prescription opioids only to relieve pain reported intranasal administration, whereas almost 80% of the intranasal administration group was comprised of individuals who used prescription opioids to get high.
ANOVA indicated a main effect of route of administration, F(3, 4473)=355.8, p<0.001, and post-hoc tests confirmed the mean DAST-10 scores among individuals who reported intranasal and other non-oral routes of administration were significantly higher than the mean DAST-10 scores of non-users and nonmedical users who reported oral administration only (see Fig. 3). Furthermore, approximately 6% of non-users and 26% of nonmedical users who reported oral administration only reported experiencing three or more drug related problems in the past year based on the DAST-10 screening instrument as compared to 67% of intranasal users and 80% of those who reported other routes of administration (χ2 =661.8, df=3, p<0.001). Among lifetime users (n=640), multiple logistic regression analyses adjusting for gender, class year, race/ethnicity, and living arrangement revealed nonmedical users of prescription opioids who reported intranasal administration (AOR=5.8, 95% CI=3.2–10.5, p<0.001) and other non-oral routes administration (AOR=10.1, 95% CI=4.0–25.3, p<0.001) had considerably increased odds of experiencing three or more drug use related problems in the past year as compared to nonmedical users who reported oral administration only.
Fig. 3.
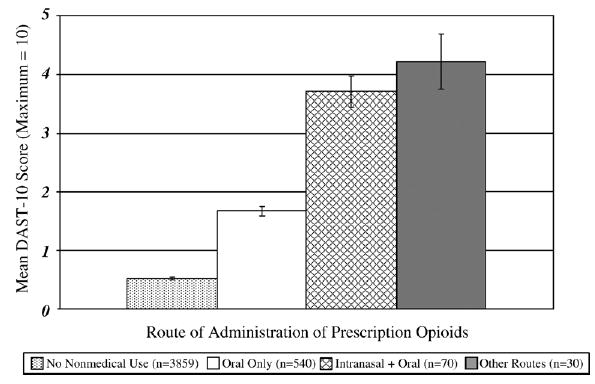
Mean DAST-10 scores as a function of route of administration of nonmedical prescription opioids. Error bars represent ± 1 S.E. Intranasal+oral (n=70) excluded other non-oral routes. Other routes (n=30) included smoking, injecting, and/or inhaling but did not exclude oral or intranasal. ANOVA showed a main effect of route of administration, F(3, 4473)=355.8, p<0.001. Post-hoc tests indicated the mean DAST-10 score among individuals who reported intranasal and other routes of administration was significantly higher than mean DAST-10 scores of non-users and nonmedical users who reported oral only route of administration (p<0.05).
4. Discussion
Findings from this research are similar to other national studies; in the United States, hydrocodone, codeine, oxycodone and propoxyphene are the prescription opioids most likely to be used nonmedically (Johnston et al., 2005a, 2005b; SAMHSA, 2005a). The present study found that the single leading reason provided by college youth for nonmedical use of prescription opioids was to relieve pain and for those endorsing this motivation as the sole reason for use, there was no increase in risk of other substance abuse problems. However, nonmedical users of prescription opioids who reported motives other than pain relief had 15 times the odds of experiencing three or more drug use related problems based on the DAST-10 than students who did not report nonmedical use of prescription opioids. These findings suggest that health professionals working with college youth should inquire about motives since there is substantially greater risk for substance abuse associated with motives other than to relieve pain.
The findings of the present study provided evidence that a substantial proportion of collegiate nonmedical users of prescription opioids obtain these drugs from peers and these nonmedical users are at increased risk for alcohol and other drug use related problems. The present study also found that nonmedical users who obtained these drugs from parents were not at the same increased risk for alcohol and other drug use related problems as students who obtained these drugs from non-parental sources. Although students who obtained prescription opioids from parents did not have higher rates of other substance use behaviors, there are risks associated with using diverted prescription pain medication. College students who use prescription opioids provided by parents or other non-physician sources do not receive important prescribing information such as dosage, contraindications or drug interactions. Furthermore, prescription opioids carry the risk of causing both physical dependence and withdrawal symptoms upon discontinuation, which should be discussed with any individual using these medications. In the future, health education efforts should inform parents about the potential dangers associated with providing prescription medications to their children; clearly parents should obtain appropriate medical care to treat their children's pain.
Although recent investigations have demonstrated the feasibility of purchasing prescription drugs online without a prescription (Califano, 2004; Forman, 2003), the present investigation along with another college-based study do not suggest that college youth are obtaining prescription opioids directly from the internet (McCabe & Boyd, 2005). Indeed, the present study found only 1 out of 640 lifetime nonmedical users reported obtaining prescription opioids via the Internet. The lack of direct online purchases in the present study could be a result of these college youth having easy access to less expensive sources such as peers and family members. Future work should continue to examine the role of the Internet as a possible source of obtaining prescription opioids by nonmedical users.
The findings of the present study have important implications for prevention and intervention efforts. For instance, more than 1 in every 10 lifetime nonmedical users reported intranasal administration. Furthermore, approximately 67% of intranasal users and 80% of other non-oral users reported experiencing three or more drug use related problems in the past year. The use of prescription opioids via intranasal and other non-oral routes of administration are extremely dangerous drug use behaviors that have been linked to a number of adverse physical consequences (Jewers et al., 2005; Watson et al., 2004; Yewell, Haydon, Archer, & Manaligod, 2002). Additionally, the rate of delivery of drug to the brain directly correlates to the abuse potential of the drug and intranasal along with other non-oral routes of administration are expected to deliver drug to the brain at a much faster rate than oral administration (Kollins, 2003; Roset et al., 2001). These factors (i.e., route and rate) have important implications for the addictive potential of various drugs, and hence intranasal and other non-oral routes of administration of prescription drugs should be assessed and monitored closely by college administrators and health professionals involved in providing substance abuse services to college students. Individuals who are identified as using prescription opioids intranasally or via other non-oral routes of administration should be informed about the potential severe consequences of such use and referred for a comprehensive substance abuse assessment.
The majority of undergraduate students in the present study initiated nonmedical use of prescription opioids before they entered college. This finding, along with research showing high rates of nonmedical use of prescription opioids observed among secondary school students (Boyd et al., 2006; Johnston, O'Malley, Bachman, & Schulenberg, 2005b), indicate that prevention and intervention efforts should begin well before college. Such efforts, aimed at high school and undergraduate students should take into account differential risks, including risks associated with route of administration, motive to use, and source of the prescription drugs. Such preventative efforts should also consider gender differences in behaviors associated with nonmedical use of prescription opioids. For example, although there were no gender differences in the prevalence of nonmedical use of prescription opioids, undergraduate men were considerably more likely than women to use prescription opioids to get high and to experiment.
There are some limitations that should be taken into account while considering the implications of the results. First, the findings of the present study may not generalize to other adolescent and young adult populations because our sample was drawn from one university. While the present sample resembles the demographic characteristics of 4-year U.S. colleges and universities nationally, previous research has found that rates of nonmedical use of prescription opioids vary across different types of U.S. colleges and universities (McCabe, Teter, Boyd, Knight, & Wechsler, 2005b) as well as between young adults attending college versus those not attending college (Johnston et al., 2005a; SAMHSA, 2005b). Future investigations should examine multiple colleges and universities as well as young adults not attending college to assess the generality of the present findings. Second, there remains the possibility that students could have underestimated or overestimated the prevalence of nonmedical use of opioid analgesics. While we can never fully eliminate the misinterpretation of question wording, we tried to minimize its impact through the following strategies: 1) including the term "opioid" in the question stem, 2) including both generic and brand names of relevant and commonly prescribed drugs as examples of opioids and 3) asking students a follow-up question to specify the pain medication not prescribed to them to confirm they had used a prescription opioid. Furthermore, prevalence rates of nonmedical use of prescription opioids in this study were comparable to other national studies of U.S. college students (Johnston et al., 2005a; McCabe, Teter, Boyd, Knight, et al., 2005b). Finally, although nonresponse may have introduced potential bias in the present study, we assessed its potential impact by administering a short form of the questionnaire via a brief telephone survey to a randomly selected sample of students who did not respond to the original Web survey and found no evidence for nonresponse bias.
This study provides new directions for policy and research regarding prescription opioid abuse. The results suggest that self-treatment with opioid analgesics must be considered in future policy and research efforts. Future research should examine why college-age young adults did not obtain their own prescription; after all, if nearly 1 in 10 students use prescription pain medications to relieve pain–nonmedically–one could conclude that young adults are not being adequately treated for their pain. Additionally, special consideration needs to be given to nonmedical users of prescription opioids with motives other than pain relief, nonmedical users who obtain prescription opioids from non-parental sources, and nonmedical users who report non-oral routes of administration because these individuals appear to be at increased risk for substance abuse behaviors. Finally, an understanding and clarification as to which students are most at risk when reporting the nonmedical use of prescription opioids can considerably aid clinicians in both screening and intervention efforts.
Acknowledgments
This study and development of this manuscript was supported by a research grant R03 DA 018239 (PI: Sean Esteban McCabe) from the National Institute on Drug Abuse, National Institutes of Health.
Footnotes
Preliminary results were presented at the Society for Research Prevention Annual Meeting, 2005 and the American Society of Criminology Annual Meeting, 2005.
References
- Boyd CJ, McCabe SE, Teter CJ. Medical and nonmedical use of prescription pain medication by youth in a Detroit-area public school district. Drug and Alcohol Dependence. 2006;81:37–45. doi: 10.1016/j.drugalcdep.2005.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Califano J. You've got Drugs!" Prescription drug pushers on the Internet. A CASA white paper. New York, Columbia University: The National Center on Addiction and Substance Abuse; 2004. [Google Scholar]
- Cocco KM, Carey KB. Psychometric properties of the Drug Abuse Screening Test in psychiatric outpatients. Psychological Assessment. 1998;10:408–414. [Google Scholar]
- Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: Concerns and strategies. Drug and Alcohol Dependence. 2006;81:103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Cone EJ, Fant RV, Rohay JM, Caplan YH, Ballina M, Reder RF, et al. Oxycodone involvement in drug abuse deaths: II. Evidence for toxic multiple drug–drug interactions. Journal of Analytical Toxicology. 2004;28:616–624. doi: 10.1093/jat/28.7.616. [DOI] [PubMed] [Google Scholar]
- Ewing JA. Detecting alcoholism: The CAGE questionnaire. JAMA. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- Forman RF. Availability of opioids on the internet. JAMA. 2003;290:889. doi: 10.1001/jama.290.7.889. [DOI] [PubMed] [Google Scholar]
- French MT, Roebuck MC, McGeary KA, Chitwood DD, McCoy CB. Using the drug abuse screening test (DAST-10) to analyze health services utilization and cost for substance users in a community-based setting. Substance Use and Misuse. 2001;36:927–946. doi: 10.1081/ja-100104096. [DOI] [PubMed] [Google Scholar]
- Heck EJ. Developing a screening questionnaire for problem drinking in college students. Journal of American College Health. 1991;39:227–231. doi: 10.1080/07448481.1991.9936239. [DOI] [PubMed] [Google Scholar]
- Jewers WM, Rawal YB, Allen CM, Kalmar JR, Fox E, Chacon GE, et al. Palatal perforation associated with intranasal prescription narcotic abuse. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, Endodontology. 2005;99:594–597. doi: 10.1016/j.tripleo.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM. Why do the nation's students use drugs and alcohol? Self-reported reasons from nine national surveys. Journal of Drug Issues. 1986;16:29–66. [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. College students and adults ages 19–45. II. Bethesda, MD: National Institute on Drug Abuse (NIH Publication 05–5728); 2005a. Monitoring the future National survey results on drug use, 1975–2004. [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Secondary school students. I. Bethesda, MD: National Institute on Drug Abuse (NIH Publication 05–5727); 2005b. Monitoring the future national survey results on drug use, 1975–2004. [Google Scholar]
- Katz DA, Hays LR. Adolescent OxyContin abuse. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:231–234. doi: 10.1097/00004583-200402000-00020. [DOI] [PubMed] [Google Scholar]
- Kollins SH. Comparing the abuse potential of methylphenidate versus other stimulants: A review of available evidence and relevance to the ADHD patient. Journal of Clinical Psychiatry. 2003;64:14–18. [PubMed] [Google Scholar]
- Maisto SA, Carey MP, Carey KB, Gordon CM, Gleason JR. Use of the AUDIT and the DAST-10 to identify alcohol and drug use disorders among adults with a severe and persistent mental illness. Psychological Assessment. 2000;12:186–192. doi: 10.1037//1040-3590.12.2.186. [DOI] [PubMed] [Google Scholar]
- Mayfield D, McLeod G, Hall P. The CAGE questionnaire: Validation of a new alcoholism screening instrument. American Journal of Psychiatry. 1974;131:1121–1123. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ. Sources of prescription drugs for illicit use. Addictive Behaviors. 2005;30:1342–1350. doi: 10.1016/j.addbeh.2005.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. Illicit use of prescription pain medication among college students. Drug and Alcohol Dependence. 2005a;77:37–47. doi: 10.1016/j.drugalcdep.2004.07.005. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ, Knight JR, Wechsler H. Nonmedical use of prescription opioids among U.S. college students: Prevalence and correlates from a national survey. Addictive Behaviors. 2005b;30:789–805. doi: 10.1016/j.addbeh.2004.08.024. [DOI] [PubMed] [Google Scholar]
- Mohler-Kuo M, Lee JE, Wechsler H. Trends in marijuana and other illicit drug use among college students: Results from 4 Harvard School of Public Health College Alcohol Study surveys: 1993–2001. Journal of American College Health. 2003;52:17–24. doi: 10.1080/07448480309595719. [DOI] [PubMed] [Google Scholar]
- Pedersen W, Lavik NJ. Adolescents and benzodiazepines: Prescribed use, self-medication and intoxication. Acta Psychiatrica Scandinavica. 1991;84:94–98. doi: 10.1111/j.1600-0447.1991.tb01427.x. [DOI] [PubMed] [Google Scholar]
- Roset PN, Farre M, de la Torre R, Mas M, Menoyo E, et al. Modulation of rate of onset and intensity of drug effects reduces abuse potential in healthy males. Drug and Alcohol Dependence. 2001;64:285–298. doi: 10.1016/s0376-8716(01)00127-2. [DOI] [PubMed] [Google Scholar]
- Skinner H. The Drug Abuse Screening Test. Addictive Behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The DAWN Report: Oxycodone, hydrocodone, and polydrug use, 2002. Available at: http://oas.samhsa.gov/2k4/oxycodone/oxycodone.cfm. Accessed August. 2004;10:2004. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The NSDUH Report: Nonmedical use of prescription pain relievers. Available at: http://oas.samhsa.gov/2k4/pain/pain.pdf. Accessed August. 2005a;10:2005. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The NSDUH Report: College Enrollment Status and Past Year Nonmedical Drug Use among Young Adults: 2002, 2003, and 2004. 2005b. [Accessed October 25, 2005]. Available at: http://oas.samhsa.gov/2k5/College/college.pdf. [Google Scholar]
- Watson WA, Litovitz TL, Klein-Schwartz W, Rodgers GC, Youniss J, Reid N, et al. 2003 annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. American Journal of Emergency Medicine. 2004;22:335–404. doi: 10.1016/j.ajem.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Dowdall GW, Davenport A, Rimm EB. A gender-specific measure of binge drinking among college students. American Journal of Public Health. 1995;85:982–985. doi: 10.2105/ajph.85.7.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yewell J, Haydon R, Archer S, Manaligod JM. Complications of intranasal prescription narcotic abuse. Annals of Otology, Rhinology & Laryngology. 2002;111:174–177. doi: 10.1177/000348940211100212. [DOI] [PubMed] [Google Scholar]
- Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on Problems of Drug Dependence taskforce on prescription opioid non-medical use and abuse: Position statement. Drug and Alcohol Dependence. 2003;69:215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]


