Abstract
Many of the symptoms characteristic of the functional gastrointestinal disorders (FGID) are consistent with dysfunction of the motor and/or sensory apparatus of the digestive tract. Those aspects of sensorimotor dysfunction most relevant to the FGID include alterations in: gut contractile activity; myoelectrical activity; tone and compliance; and transit, as well as an enhanced sensitivity to distension, in each region of the gastrointestinal tract. Assessment of these phenomena involves a number of techniques, some well established and others requiring further validation. Using such techniques, researchers have reported a wide range of alterations in sensory and in motor function in the FGID. Importantly, however, relationships between such dysfunction and symptoms have been relatively weak, and so the clinical relevance of the former remains unclear. Moreover, the proportions of patients in the various symptom subgroups who display dysfunction, and the extent and severity of their symptoms, require better characterization. On a positive note, progress is occurring on several fronts, especially in relation to functional dyspepsia and irritable bowel syndrome, and based on the data gathered to date, a number of areas where further advances are required can be highlighted. Keywords: motility; sensation; gastrointestinal tract; functional gut disorders; functional dyspepsia; irritable bowel syndrome; visceral hyperalgesia; Rome II
Full Text
The Full Text of this article is available as a PDF (136.3 KB).
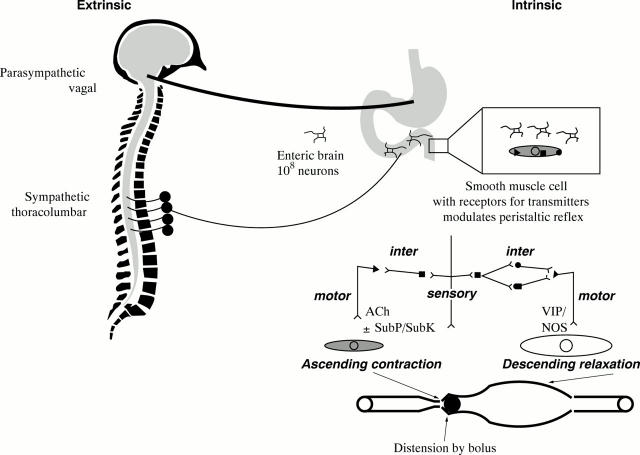
Figure 1 .
Extrinsic and intrinsic control of gastrointestinal motility. The extrinsic sympathetic and parasympathetic supply to the gut modulates the function of the enteric brain located in ganglionated plexi along the gastrointestinal tract. Transmitters released from the enteric neurons, which are the intrinsic neural control of the gut, modulate the peristaltic reflex. The major transmitters in the peristaltic reflex are shown on the right, acetylcholine (ACh) and substance P (SubP) are the predominant excitatory neurotransmitters, and vasoactive intestinal polypeptide (VIP) and nitric oxide are the predominant inhibitory neurotransmitters. SubK, substance K; NOS, nitric oxide synthase. (Reproduced with permission, Ann Rev Med 1999 (in press).)
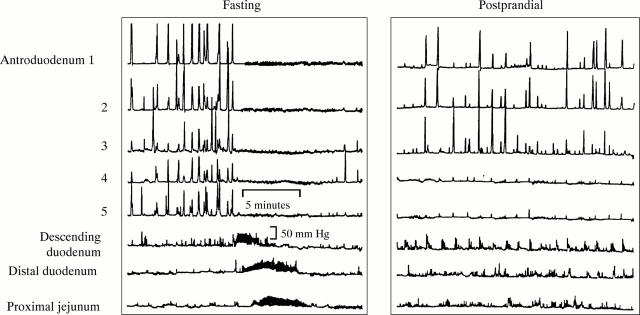
Figure 2 .
Example of fasting and postprandial motility in a healthy subject. Note the activity front (phase 3 of the migrating motor complex) during fasting (left panel) and the sustained but irregular contractile phasic pressure activity postprandially. (Reproduced with permission, Ann Rev Med 1999 (in press).)
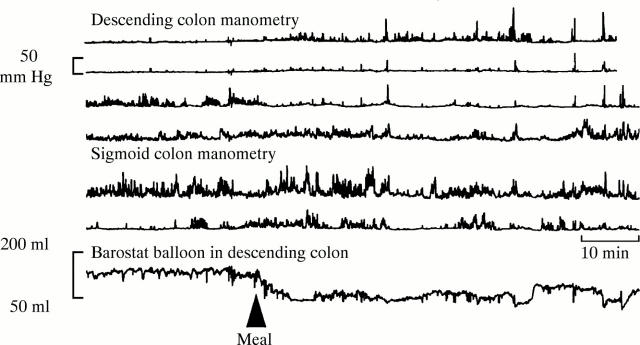
Figure 3 .
Colonic motility measured by means of manometry and barostatically controlled balloon in a healthy subject. Note the postprandial increase in phasic pressure activity in the descending colon, and the reduction in balloon volume, signifying an increase in colonic tone.
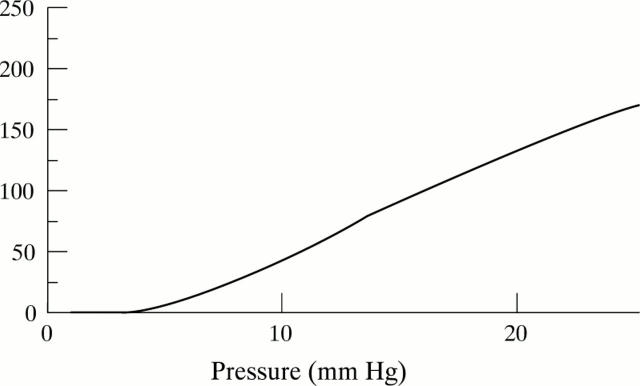
Figure 4 .
Compliance curve (dV:dP) drawn for human colon in a healthy subject.
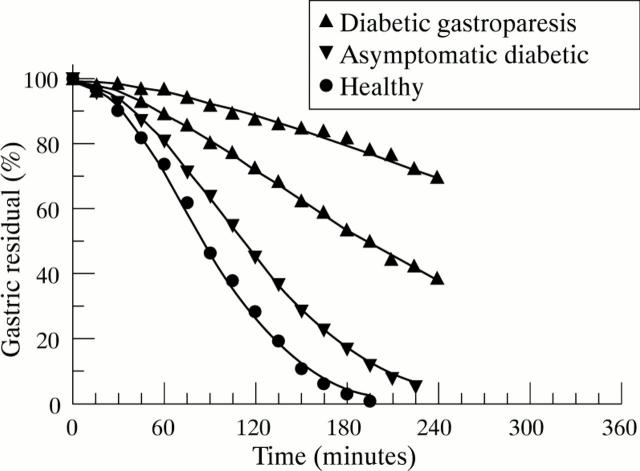
Figure 5 .
Gastric emptying of solids measured using scintigraphy: note the delay in gastric emptying t1/2 in a symptomatic diabetic patient compared with an asymptomatic patient and a healthy subject.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Accarino A. M., Azpiroz F., Malagelada J. R. Selective dysfunction of mechanosensitive intestinal afferents in irritable bowel syndrome. Gastroenterology. 1995 Mar;108(3):636–643. doi: 10.1016/0016-5085(95)90434-4. [DOI] [PubMed] [Google Scholar]
- Aggarwal A., Cutts T. F., Abell T. L., Cardoso S., Familoni B., Bremer J., Karas J. Predominant symptoms in irritable bowel syndrome correlate with specific autonomic nervous system abnormalities. Gastroenterology. 1994 Apr;106(4):945–950. doi: 10.1016/0016-5085(94)90753-6. [DOI] [PubMed] [Google Scholar]
- Awouters F., Megens A., Verlinden M., Schuurkes J., Niemegeers C., Janssen P. A. Loperamide. Survey of studies on mechanism of its antidiarrheal activity. Dig Dis Sci. 1993 Jun;38(6):977–995. doi: 10.1007/BF01295711. [DOI] [PubMed] [Google Scholar]
- Aziz Q., Thompson D. G. Brain-gut axis in health and disease. Gastroenterology. 1998 Mar;114(3):559–578. doi: 10.1016/s0016-5085(98)70540-2. [DOI] [PubMed] [Google Scholar]
- Bueno L., Fioramonti J., Delvaux M., Frexinos J. Mediators and pharmacology of visceral sensitivity: from basic to clinical investigations. Gastroenterology. 1997 May;112(5):1714–1743. doi: 10.1016/s0016-5085(97)70056-8. [DOI] [PubMed] [Google Scholar]
- Bueno L., Fioramonti J., Ruckebusch Y., Frexinos J., Coulom P. Evaluation of colonic myoelectrical activity in health and functional disorders. Gut. 1980 Jun;21(6):480–485. doi: 10.1136/gut.21.6.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camilleri M., Hasler W. L., Parkman H. P., Quigley E. M., Soffer E. Measurement of gastrointestinal motility in the GI laboratory. Gastroenterology. 1998 Sep;115(3):747–762. doi: 10.1016/s0016-5085(98)70155-6. [DOI] [PubMed] [Google Scholar]
- Camilleri M., Von der Ohe M. R. Drugs affecting serotonin receptors. Baillieres Clin Gastroenterol. 1994 Jun;8(2):301–319. doi: 10.1016/0950-3528(94)90006-x. [DOI] [PubMed] [Google Scholar]
- Clouse R. E. Antidepressants for functional gastrointestinal syndromes. Dig Dis Sci. 1994 Nov;39(11):2352–2363. doi: 10.1007/BF02087651. [DOI] [PubMed] [Google Scholar]
- Coffin B., Azpiroz F., Guarner F., Malagelada J. R. Selective gastric hypersensitivity and reflex hyporeactivity in functional dyspepsia. Gastroenterology. 1994 Nov;107(5):1345–1351. doi: 10.1016/0016-5085(94)90536-3. [DOI] [PubMed] [Google Scholar]
- Collins S. M. The immunomodulation of enteric neuromuscular function: implications for motility and inflammatory disorders. Gastroenterology. 1996 Dec;111(6):1683–1699. doi: 10.1016/s0016-5085(96)70034-3. [DOI] [PubMed] [Google Scholar]
- Cook I. J., van Eeden A., Collins S. M. Patients with irritable bowel syndrome have greater pain tolerance than normal subjects. Gastroenterology. 1987 Oct;93(4):727–733. doi: 10.1016/0016-5085(87)90434-3. [DOI] [PubMed] [Google Scholar]
- Delvaux M., Louvel D., Lagier E., Scherrer B., Abitbol J. L., Frexinos J. The kappa agonist fedotozine relieves hypersensitivity to colonic distention in patients with irritable bowel syndrome. Gastroenterology. 1999 Jan;116(1):38–45. doi: 10.1016/s0016-5085(99)70226-x. [DOI] [PubMed] [Google Scholar]
- Drossman D. A., Whitehead W. E., Camilleri M. Irritable bowel syndrome: a technical review for practice guideline development. Gastroenterology. 1997 Jun;112(6):2120–2137. doi: 10.1053/gast.1997.v112.agast972120. [DOI] [PubMed] [Google Scholar]
- Dykhuizen R. S., Masson J., McKnight G., Mowat A. N., Smith C. C., Smith L. M., Benjamin N. Plasma nitrate concentration in infective gastroenteritis and inflammatory bowel disease. Gut. 1996 Sep;39(3):393–395. doi: 10.1136/gut.39.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans P. R., Bennett E. J., Bak Y. T., Tennant C. C., Kellow J. E. Jejunal sensorimotor dysfunction in irritable bowel syndrome: clinical and psychosocial features. Gastroenterology. 1996 Feb;110(2):393–404. doi: 10.1053/gast.1996.v110.pm8566585. [DOI] [PubMed] [Google Scholar]
- Farrugia G., Camilleri M., Whitehead W. E. Therapeutic strategies for motility disorders. Medications, nutrition, biofeedback, and hypnotherapy. Gastroenterol Clin North Am. 1996 Mar;25(1):225–246. doi: 10.1016/s0889-8553(05)70373-3. [DOI] [PubMed] [Google Scholar]
- Fock K. M., Khoo T. K., Chia K. S., Sim C. S. Helicobacter pylori infection and gastric emptying of indigestible solids in patients with dysmotility-like dyspepsia. Scand J Gastroenterol. 1997 Jul;32(7):676–680. doi: 10.3109/00365529708996517. [DOI] [PubMed] [Google Scholar]
- Frexinos J., Bueno L., Fioramonti J. Diurnal changes in myoelectric spiking activity of the human colon. Gastroenterology. 1985 May;88(5 Pt 1):1104–1110. doi: 10.1016/s0016-5085(85)80067-6. [DOI] [PubMed] [Google Scholar]
- Greydanus M. P., Vassallo M., Camilleri M., Nelson D. K., Hanson R. B., Thomforde G. M. Neurohormonal factors in functional dyspepsia: insights on pathophysiological mechanisms. Gastroenterology. 1991 May;100(5 Pt 1):1311–1318. [PubMed] [Google Scholar]
- Holtmann G., Talley N. J., Goebell H. Association between H. pylori, duodenal mechanosensory thresholds, and small intestinal motility in chronic unexplained dyspepsia. Dig Dis Sci. 1996 Jul;41(7):1285–1291. doi: 10.1007/BF02088548. [DOI] [PubMed] [Google Scholar]
- Hveem K., Jones K. L., Chatterton B. E., Horowitz M. Scintigraphic measurement of gastric emptying and ultrasonographic assessment of antral area: relation to appetite. Gut. 1996 Jun;38(6):816–821. doi: 10.1136/gut.38.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellow J. E., Phillips S. F., Miller L. J., Zinsmeister A. R. Dysmotility of the small intestine in irritable bowel syndrome. Gut. 1988 Sep;29(9):1236–1243. doi: 10.1136/gut.29.9.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingham J. G., Dawson A. M. Origin of chronic right upper quadrant pain. Gut. 1985 Aug;26(8):783–788. doi: 10.1136/gut.26.8.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malagelada J. R. Functional dyspepsia. Insights on mechanisms and management strategies. Gastroenterol Clin North Am. 1996 Mar;25(1):103–112. doi: 10.1016/s0889-8553(05)70367-8. [DOI] [PubMed] [Google Scholar]
- Mayer E. A., Gebhart G. F. Basic and clinical aspects of visceral hyperalgesia. Gastroenterology. 1994 Jul;107(1):271–293. doi: 10.1016/0016-5085(94)90086-8. [DOI] [PubMed] [Google Scholar]
- McLaughlin J. T., Troncon L. E., Barlow J., Heggie L. J., Thompson D. G. Evidence for a lipid specific effect in nutrient induced human proximal gastric relaxation. Gut. 1998 Aug;43(2):248–251. doi: 10.1136/gut.43.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mearin F., Cucala M., Azpiroz F., Malagelada J. R. The origin of symptoms on the brain-gut axis in functional dyspepsia. Gastroenterology. 1991 Oct;101(4):999–1006. doi: 10.1016/0016-5085(91)90726-2. [DOI] [PubMed] [Google Scholar]
- Mertz H., Fass R., Kodner A., Yan-Go F., Fullerton S., Mayer E. A. Effect of amitriptyline on symptoms, sleep, and visceral perception in patients with functional dyspepsia. Am J Gastroenterol. 1998 Feb;93(2):160–165. doi: 10.1111/j.1572-0241.1998.00160.x. [DOI] [PubMed] [Google Scholar]
- Moriarty K. J., Dawson A. M. Functional abdominal pain: further evidence that whole gut is affected. Br Med J (Clin Res Ed) 1982 Jun 5;284(6330):1670–1672. doi: 10.1136/bmj.284.6330.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narducci F., Bassotti G., Gaburri M., Morelli A. Twenty four hour manometric recording of colonic motor activity in healthy man. Gut. 1987 Jan;28(1):17–25. doi: 10.1136/gut.28.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owyang C. Octreotide in gastrointestinal motility disorders. Gut. 1994;35(3 Suppl):S11–S14. doi: 10.1136/gut.35.3_suppl.s11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace F., Coremans G., Dapoigny M., Müller-Lissner S. A., Smout A., Stockbruegger R. W., Whorwell P. J. Therapy of irritable bowel syndrome--an overview. Digestion. 1995;56(5):433–442. doi: 10.1159/000201272. [DOI] [PubMed] [Google Scholar]
- Peeters T. L. Erythromycin and other macrolides as prokinetic agents. Gastroenterology. 1993 Dec;105(6):1886–1899. doi: 10.1016/0016-5085(93)91089-z. [DOI] [PubMed] [Google Scholar]
- Poynard T., Naveau S., Mory B., Chaput J. C. Meta-analysis of smooth muscle relaxants in the treatment of irritable bowel syndrome. Aliment Pharmacol Ther. 1994 Oct;8(5):499–510. doi: 10.1111/j.1365-2036.1994.tb00322.x. [DOI] [PubMed] [Google Scholar]
- Quigley E. M. Gastric and small intestinal motility in health and disease. Gastroenterol Clin North Am. 1996 Mar;25(1):113–145. doi: 10.1016/s0889-8553(05)70368-x. [DOI] [PubMed] [Google Scholar]
- Sarna S. K. Physiology and pathophysiology of colonic motor activity (1). Dig Dis Sci. 1991 Jun;36(6):827–862. doi: 10.1007/BF01311244. [DOI] [PubMed] [Google Scholar]
- Scarinci I. C., McDonald-Haile J., Bradley L. A., Richter J. E. Altered pain perception and psychosocial features among women with gastrointestinal disorders and history of abuse: a preliminary model. Am J Med. 1994 Aug;97(2):108–118. doi: 10.1016/0002-9343(94)90020-5. [DOI] [PubMed] [Google Scholar]
- Serra J., Azpiroz F., Malagelada J. R. Intestinal gas dynamics and tolerance in humans. Gastroenterology. 1998 Sep;115(3):542–550. doi: 10.1016/s0016-5085(98)70133-7. [DOI] [PubMed] [Google Scholar]
- Silverman D. H., Munakata J. A., Ennes H., Mandelkern M. A., Hoh C. K., Mayer E. A. Regional cerebral activity in normal and pathological perception of visceral pain. Gastroenterology. 1997 Jan;112(1):64–72. doi: 10.1016/s0016-5085(97)70220-8. [DOI] [PubMed] [Google Scholar]
- Stanghellini V., Tosetti C., Paternico A., Barbara G., Morselli-Labate A. M., Monetti N., Marengo M., Corinaldesi R. Risk indicators of delayed gastric emptying of solids in patients with functional dyspepsia. Gastroenterology. 1996 Apr;110(4):1036–1042. doi: 10.1053/gast.1996.v110.pm8612991. [DOI] [PubMed] [Google Scholar]
- Steadman C. J., Phillips S. F., Camilleri M., Haddad A. C., Hanson R. B. Variation of muscle tone in the human colon. Gastroenterology. 1991 Aug;101(2):373–381. doi: 10.1016/0016-5085(91)90014-c. [DOI] [PubMed] [Google Scholar]
- Swarbrick E. T., Hegarty J. E., Bat L., Williams C. B., Dawson A. M. Site of pain from the irritable bowel. Lancet. 1980 Aug 30;2(8192):443–446. doi: 10.1016/s0140-6736(80)91885-1. [DOI] [PubMed] [Google Scholar]
- Tack J., Piessevaux H., Coulie B., Caenepeel P., Janssens J. Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology. 1998 Dec;115(6):1346–1352. doi: 10.1016/s0016-5085(98)70012-5. [DOI] [PubMed] [Google Scholar]
- Tanum L., Malt U. F. A new pharmacologic treatment of functional gastrointestinal disorder. A double-blind placebo-controlled study with mianserin. Scand J Gastroenterol. 1996 Apr;31(4):318–325. doi: 10.3109/00365529609006404. [DOI] [PubMed] [Google Scholar]
- Valori R. M., Kumar D., Wingate D. L. Effects of different types of stress and of "prokinetic" drugs on the control of the fasting motor complex in humans. Gastroenterology. 1986 Jun;90(6):1890–1900. doi: 10.1016/0016-5085(86)90258-1. [DOI] [PubMed] [Google Scholar]
- Whitehead W. E., Delvaux M. Standardization of barostat procedures for testing smooth muscle tone and sensory thresholds in the gastrointestinal tract. The Working Team of Glaxo-Wellcome Research, UK. Dig Dis Sci. 1997 Feb;42(2):223–241. doi: 10.1023/a:1018885028501. [DOI] [PubMed] [Google Scholar]
- Whitehead W. E., Holtkotter B., Enck P., Hoelzl R., Holmes K. D., Anthony J., Shabsin H. S., Schuster M. M. Tolerance for rectosigmoid distention in irritable bowel syndrome. Gastroenterology. 1990 May;98(5 Pt 1):1187–1192. doi: 10.1016/0016-5085(90)90332-u. [DOI] [PubMed] [Google Scholar]
- Whitehead W. E., Palsson O. S. Is rectal pain sensitivity a biological marker for irritable bowel syndrome: psychological influences on pain perception. Gastroenterology. 1998 Nov;115(5):1263–1271. doi: 10.1016/s0016-5085(98)70099-x. [DOI] [PubMed] [Google Scholar]
- Wilmer A., Van Cutsem E., Andrioli A., Tack J., Coremans G., Janssens J. Ambulatory gastrojejunal manometry in severe motility-like dyspepsia: lack of correlation between dysmotility, symptoms, and gastric emptying. Gut. 1998 Feb;42(2):235–242. doi: 10.1136/gut.42.2.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiseman L. R., Faulds D. Cisapride. An updated review of its pharmacology and therapeutic efficacy as a prokinetic agent in gastrointestinal motility disorders. Drugs. 1994 Jan;47(1):116–152. doi: 10.2165/00003495-199447010-00008. [DOI] [PubMed] [Google Scholar]