Age adjusted hospitalisation rates for heart failure have increased considerably throughout the western world in the 1980s and early 1990s, as documented by reports from New Zealand, the USA, Sweden, Spain, Scotland, and the Netherlands.1,2 Hospitalisations account for as much as 70% of the health care budget spent on heart failure.1 Angiotensin converting enzyme (ACE) inhibition became the cornerstone of heart failure treatment in the 1990s, following demonstration of reduction in mortality and readmissions in patients with heart failure or left ventricular dysfunction enrolled in clinical trials.3 We examined trends in hospitalisations for heart failure and ACE inhibitor prescription rates in the Netherlands from 1980 to 1999.
PARTICIPANTS, METHODS, AND RESULTS
All hospital admissions, including in-hospital deaths, with a first listed discharge diagnosis of heart failure were studied, using the methods described in detail previously.2 Briefly, International classification of diseases, ninth revision (ICD-9) codes 428.x (heart failure), 402.x (hypertensive heart disease), and 429.1 (myocardial degeneration) were used to identify discharges for heart failure. Complete national data on discharges were obtained from Prismant and on Dutch population figures from Statistics Netherlands. From 1980 to 1999 the mean age of patients admitted for heart failure increased from 71.2 to 72.9 years in men and from 75.0 to 77.7 years in women. Age adjusted discharge rates were calculated by direct standardisation to the European standard population. Trends over time in discharge rates were analysed separately for men and women using Poisson regression. The model included calendar year, both linear and quadratic, and five year age groups (categorical) as explanatory variables. Nationwide information on ACE inhibition prescription was obtained from IMS Medical Index and Farminform FI-ROM/Aventis, the Netherlands.
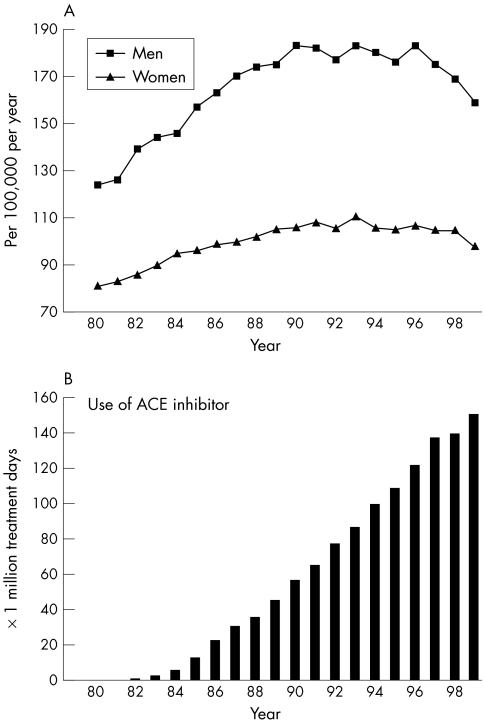
The total number of hospitalisations for heart failure increased by 72% between 1980 (14441) and 1999 (24868). The quadratic term of calendar year was highly significant and negative in sign in both men (β = −0.00267; p = 0.0001) and women (β = −0.00181; p = 0.0001), indicating that following an increase in hospitalisation rates in the beginning of the study period a peak was reached in 1992 for men and in 1993 for women (fig 1A). For men the average annual increase between 1980 and 1992 was estimated at 4.3%, followed by a small annual decrease of 1.5% in the years thereafter. For women the average annual increase between 1980 and 1993 was 2.8%, followed by an annual decrease of 1.0%. The average duration of hospitalisation declined steadily from 21.1 days in 1980 to 12.9 days in 1999. In-hospital mortality declined from 18.6% to 13.5%.
Figure 1.
(A) Age adjusted discharge rates for heart failure, the Netherlands, 1980–1999. Source: Prismant, the Netherlands. The “new” European standard population was used as a standard. (B) ACE inhibitor use (in million treatment days per year) in the Netherlands, 1980–1999. Source: Farminform FI-ROM/Aventis Pharma, the Netherlands.
Since their introduction in the 1980s, ACE inhibition prescription rates continued to increase in the 1990s, more than doubling between 1990 (56.8 million treatment days) and 1999 (151.8 million treatment days) (fig 1B). Currently, the predominant indication for ACE inhibition prescription is primary hypertension (65.0%). Heart failure and chronic ischaemic heart disease account for 9.4%. In patients with a diagnosis of heart failure diuretics (69.4%) were the most frequently prescribed drugs, followed by ACE inhibitors (30.7%) and digoxin (14.5%). In 1983, two years after introduction of the first ACE inhibitor, captopril, on the Dutch market, 81% of treated patients were on diuretics, 43% on digoxin, and none on an ACE inhibitor.
DISCUSSION
Our data indicate that, following a steady increase in the 1980s, age adjusted hospitalisation rates for heart failure peaked in the early 1990s. This trend was observed concomitantly with a sharp rise in the use of ACE inhibitors.
There are several possible explanations for the end to the increase in hospitalisation rates: a decrease in the incidence of heart failure, changes in admission policy and coding practice, and improved treatment and management of heart failure patients—for example, by means of dedicated heart failure clinics.
A decrease in the incidence of heart failure appears unlikely, given the current transition from acute to chronic forms of cardiovascular disease.1 The growing awareness of heart failure among physicians would probably lead to an increase rather than a decrease in hospitalisations. In addition, the coding system did not change over the study period and a survey in the Netherlands indicated that 80% of the patients discharged with ICD code 428 (heart failure) fulfilled the Framingham criteria for heart failure.2
Major advances have been made in the treatment of heart failure, notably the demonstration in the late 1980s that ACE inhibitors are effective. ACE inhibition reduces mortality (odds ratio (OR) 0.80, 95% confidence interval (CI) 0.74 to 0.87) and readmissions (OR 0.67, 95% CI 0.61 to 0.74) in patients with heart failure or left ventricular dysfunction,3 and reduces cardiovascular events (OR 0.78, 95% CI 0.70 to 0.86), including heart failure, in patients with an increased cardiovascular risk profile.4 ACE inhibition to treat hypertension is likely to prevent heart failure, or at least postpone its onset.5 More recently the benefits of β blockers, angiotensin II receptor blockers, and spironolactone are being acknowledged. As the translation of observed benefits in clinical trials to larger groups of patients takes time, a substantial effect on hospitalisation rates of the latter three classes of drugs during our study period is doubtful. Proper management of patients having heart failure may prevent up to 40% of hospital admissions for heart failure.6 The increasing difficulties encountered in admitting patients to hospital in the Netherlands—for example, because of shortages in nursing staff—may have contributed to the decline in hospitalisations and a shift towards home based care for heart failure patients.
In the face of the predicted increase in age adjusted prevalence of heart failure in the near future,1 the observed decline in hospitalisations may come as a surprise. Hospitalisations for heart failure, however, do not necessarily reflect the incidence and prevalence of heart failure in the community, as they relate only to the more severe stages of the syndrome warranting in-hospital evaluation and treatment. Other limitations inherent to hospital registration based studies for heart failure, such as non-uniform case ascertainment and changes in assessment and classification of heart failure over time, have recently been addressed,7 and do apply to our study. In addition, direct linkage of ACE inhibitor use to individual patients to assess the impact on hospitalisations for heart failure was not possible, as these data are not available in the Netherlands.
The stabilisation of heart failure hospitalisation rates, the decrease in length of stay, and the decrease in in-hospital case fatality rates are strikingly similar to recent findings from Scotland during the same period,8 suggesting that the observation that hospitalisation rates for heart failure have reached their peak represents more than a chance finding.
In conclusion, age adjusted hospitalisation rates for heart failure have peaked in the early 1990s. Although the specific contributions of different mechanisms to the observed trend remain speculative, our findings support the view that part of it can be attributed to improvements in treatment of the syndrome, notably with ACE inhibition. By further optimisation of the management of heart failure patients a large number of hospitalisations can be prevented, potentially resulting in an appreciable cost reduction.
Abbreviations
ACE, angiotensin converting enzyme;
ICD, International classification of diseases
Footnotes
Funding: This study was supported by a grant from the Netherlands Heart Foundation.
Competing interests: none.
REFERENCES
- 1.Cowie MR, Mosterd A, Wood DA, et al. The epidemiology of heart failure. Eur Heart J 1997;18:208–25. [DOI] [PubMed] [Google Scholar]
- 2.Reitsma JB, Mosterd A, de Craen AJ, et al. Increase in hospital admission rates for heart failure in the Netherlands, 1980-1993. Heart 1996;76:388–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flather MD, Yusuf S, Køber L, et al. Long-term ACE-inhibitor therapy in patients with heart failure or left-ventricular dysfunction: a systematic overview of data from individual patients. Lancet 2000;355:1575–81. [DOI] [PubMed] [Google Scholar]
- 4.Yusuf S, Sleight P, Pogue J, et al. Effect of an angiotensin-converting enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The heart outcomes prevention evaluation study investigators. N Engl J Med 2000;342:145–53. [DOI] [PubMed] [Google Scholar]
- 5.Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood pressure lowering treatment trialists' collaboration. Lancet 2000;356:1955–64. [DOI] [PubMed] [Google Scholar]
- 6.Michalsen A, Konig G, Thimme W. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart 1998;80:437–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zannad F. Have we jugulated the epidemic of heart failure? One swallow does not make a summer. Eur Heart J 2001;22:188–90. [DOI] [PubMed] [Google Scholar]
- 8.Stewart S, MacIntyre K, MacLeod MM, et al. Trends in hospitalization for heart failure in Scotland, 1990-1996. An epidemic that has reached its peak? Eur Heart J 2001;22:209–17. [DOI] [PubMed] [Google Scholar]