Abstract
Objective: To evaluate whether the presence of viable myocardium, detected by low dose dobutamine echocardiography, limits the likelihood of left ventricular dilatation in patients with acute myocardial infarction.
Patients: 107 patients were studied by low dose dobutamine echocardiography at (mean (SD)) 3 (1) days after acute myocardial infarction. Cross sectional echocardiography was repeated three months later. Patients were divided in two groups based on the presence (n = 47) or absence (n = 60) of myocardial viability.
Results: Baseline characteristics were comparable between the two groups, except for infarct location. Left ventricular end diastolic volume index (EDVI) was stable in patients with viability, but end systolic volume index (ESVI) decreased significantly (p = 0.006). Patients without viability had a significant increase in both EDVI (p < 0.0001) and ESVI (p = 0.0007). Subgroup analysis in patients with small and large infarcts (peak creatine kinase ≤ 1000 v > 1000 IU/l) showed that ventricular dilatation occurred only in patients with large infarcts without viability. This resulted in larger ESVI values at three months in that group compared with patients with large infarcts plus viability (p < 0.05). Multivariate regression analysis identified myocardial viability as an independent predictor of left ventricular dilatation, along with wall motion score index on low dose dobutamine echocardiography and the number of pathological Q waves.
Conclusions: The presence of viability early after acute myocardial infarction is associated with preservation of left ventricular size, whereas the absence of viability results in ventricular dilatation, particularly in large infarcts.
Keywords: echocardiography, myocardial infarction, remodelling, stunning
Progressive left ventricular dilatation after acute myocardial infarction, a process often referred to as remodelling, is associated with a poor prognosis.1–3 Alterations in left ventricular architecture involving both infarcted and non-infarcted myocardium lead to progressive deterioration in left ventricular function.4 Several factors predict this process: anterior infarct location, infarct size, and patency of the infarct related artery are all independently associated with progressive left ventricular dilatation.4–11 It has been found that significant dilatation occurs only after transmural myocardial necrosis.12–14 The presence of viable myocardium in the outer layers of the ventricular wall may contribute to the maintenance of left ventricular size.12,15 Under normal conditions, the outer layer of the myocardium does not show much systolic thickening, in contrast to the inner layer which is the major contributor to wall thickening in systole.16 Hence wall thickening at rest may be severely diminished after necrosis of just the inner layer of the myocardium. It has been shown that stimulation by dobutamine under these circumstances results in increased thickening of the outer layers of the myocardium and increased overall wall thickening.17 We hypothesised that the presence of dobutamine responsive wall thickening after acute myocardial infarction might indicate viable myocardium in the outer layers of the ventricular wall, which could prevent left ventricular dilatation. We tested this hypothesis using low dose dobutamine echocardiography in patients with acute myocardial infarction.
METHODS
Patients
The study population comprised 107 consecutive patients with acute myocardial infarction, admitted to the coronary care units of the Free University Hospital and the Sint Lucas-Andreas Hospital. Myocardial infarction was documented by a history of typical chest pain, ST segment elevation in two contiguous leads, and a transient rise in creatine kinase exceeding twice the upper limit of normal. Patients treated with and without thrombolysis or primary coronary angioplasty and with first or recurrent infarction, and those with Q wave or non-Q wave infarction, were eligible. Patients without baseline wall motion abnormalities or with technically difficult echocardiographic studies were excluded. Other exclusion criteria were: postinfarction angina or infarction complicated by severe haemodynamic instability; sustained ventricular tachycardia or ventricular fibrillation occurring more than 24 hours after admission; and additional revascularisation procedures before inclusion. Patients were also excluded if they had mitral valve replacement before their second echocardiogram or if there was no echocardiographic follow up. All patients gave their informed consent to this prospective study, which was approved by the science and ethics committee of our institutions.
Echocardiography
Low dose dobutamine echocardiography was performed at 3 (1) days (mean (SD); range 2–5 days) after myocardial infarction, using a Hewlett-Packard Sonos 1500 or Sonos 2500 instrument (Hewlett-Packard Inc, Andover, Massachusetts, USA) with a 2.5 MHz transducer. β Blockers were withdrawn 24 hours before the test.
After baseline cross sectional echocardiography, dobutamine was given intravenously at doses of 5 and 10 μg/kg/min for five minutes at each dose. Patients underwent continuous ECG monitoring, and blood pressure was recorded at the end of each stage. Standard parasternal and apical views were recorded on half inch VHS videotape at baseline and at the end of the dobutamine infusion. Follow up cross sectional echocardiography was repeated 3 (1) months later.
The echocardiographic images were digitised and displayed side by side in quad screen format to facilitate the comparison of images. Dobutamine echocardiograms were analysed by two observers. A third observer was involved in cases of disagreement, and a majority decision was reached. Wall motion was evaluated visually, using both endocardial motion and systolic wall thickening, and was semiquantitated using a 13 segment model of the left ventricle and a four point scoring system: 1, normokinesia; 2, hypokinesia; 3, akinesia; 4, dyskinesia.18 The assessment was based both on the digitised images displayed in a quadscreen format and on a review of the images recorded on videotape. Myocardial viability was defined as an improvement in wall motion in two or more contiguous segments during dobutamine infusion. Improved wall motion was defined as hypokinetic segments that normalised, and akinetic or dyskinetic segments that became hypokinetic or normal. Wall motion score index was calculated by summing the scores for each segment and dividing by the number of segments analysed.
Left ventricular end diastolic and end systolic volumes were determined from apical two and four chamber views using the Simpson biplane formula, according to the recommendations of the American Society of Echocardiograpy.19 Tracing of the endocardial borders was performed on a digitised frame from the technically best cardiac cycle (ECHO-CMS, Medis Medical Imaging Systems, address),20 and volumes were normalised for body surface area. Ejection fraction was calculated as [end diastolic – end systolic volume]/end diastolic volume. An increase of more than 10% in end diastolic volume index (EDVI) at follow up was defined as significant left ventricular dilatation.
Statistical analysis
Baseline descriptive data are presented as mean (SD). Group differences in clinical and echocardiographic variables were assessed by unpaired Student's t test or by χ2 analysis for proportions. Changes in left ventricular volume over time were analysed by paired Student's t test. Those variables that were significantly different between patients with and without left ventricular dilatation were submitted to univariate regression analysis. Variables that showed a significant correlation with left ventricular dilatation were included in the multivariate stepwise logistic regression model to determine the independent correlates. A probability value of p < 0.05 was considered significant.
RESULTS
Patients
On the basis of the results of low dose dobutamine echocardiography, patients were divided into two groups: 47 patients with viability and 60 without. Baseline characteristics of the two groups are shown in table 1. All clinical and echocardiographic results were similar, except for infarct location: inferior infarction was more common in patients without viability (p < 0.05). Importantly, enzymatic and echocardiographic indicators of infarct size were comparable between the two groups.
Table 1.
Baseline characteristics
| Variable | Viability (n=47) | Non-viability (n=60) | p Value |
| Age (years) | 57 (11) | 61 (12) | NS |
| Male | 41 (87%) | 51 (85%) | NS |
| Female | 6 (13%) | 10 (15%) | |
| Anterior myocardial infarction | 29 (62%) | 23 (38%) | <0.05 |
| Inferior myocardial infarction | 18 (38%) | 37 (62%) | <0.05 |
| Previous myocardial infarction | 6 (13%) | 9 (15%) | NS |
| Thrombolysis | 33 (70%) | 39 (65%) | NS |
| Primary PTCA | 7 (15%) | 4 (7%) | NS |
| Number of pathological Q waves* | 1.9 (1.7) | 2.0 (1.6) | NS |
| Peak creatine kinase (IU/l) | 1661 (1282) | 1559 (1310) | NS |
| Peak MB fraction (IU/l) | 143 (94) | 153 (107) | NS |
| Drug treatment on hospital discharge | |||
| β Blockers | 36 (77%) | 49 (82%) | NS |
| ACE inhibitors | 18 (38%) | 30 (50%) | NS |
| Nitrates | 18 (38%) | 23 (38%) | NS |
| Calcium antagonists | 7 (15%) | 11 (18%) | NS |
| End diastolic volume index (ml/m2) | 63 (8) | 63 (16) | NS |
| End systolic volume index (ml/m2) | 33 (7) | 33 (15) | NS |
| Ejection fraction (%) | 49 (6 ) | 50 (9 ) | NS |
| Wall motion score index | 1 .61 (0.21) | 1.54 (0.30) | NS |
| Number of akinetic segments | 2.1 (1.4) | 2.0 (1.7) | NS |
Values are mean (SD) or n (%).
*On the ECG at hospital discharge.
ACE, angiotensin converting enzyme; PTCA, percutaneous transluminal coronary angioplasty.
Left ventricular volumes
In patients with viability, EDVI was stable throughout the study period (baseline value, 63 (8) ml/m2; follow up value, 64 (10) ml/m2; NS), while end systolic volume index (ESVI) decreased from 33 (7) ml/m2 at baseline to 30 (8)ml/m2 at three months (p = 0.006). In contrast, left ventricular volume indices increased significantly in patients without viability: EDVI from 63 (16) to 68 (20) ml/m2 (p < 0.0001), and ESVI from 33 (15) to 36 (18) ml/m2 (p = 0.0007).
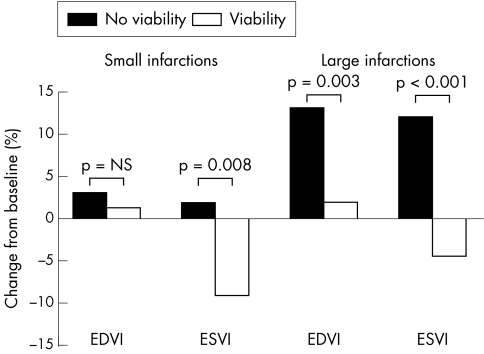
Table 2 shows the changes in left ventricular volume indices in the two groups in a subgroup of patients with small and large infarcts, based on enzymatic infarct size (peak creatine kinase ≤ 1000 IU/l and > 1000 IU/l). Baseline values were comparable between subgroups. In small infarcts, EDVI remained unchanged during the study period in both groups. ESVI decreased significantly in patients with viability but not in those without. The mean percentage change in ESVI was −9% and +2% in patients with and without viability, respectively (p = 0.008; fig 1). In large infarcts, both EDVI and ESVI remained stable in patients with viability, but increased significantly in those without. The mean percentage change in volume indices was higher in patients without viability than in those with viability (EDVI, 13% v 2%, p = 0.003; ESVI, 12% v −4%, p < 0.001; fig 1). At three months, patients without viability had larger ESVI values than patients with viability (p < 0.05; table 2).
Table 2.
Changes in left ventricular volume indices
| Small infarcts | ||||||
| Viability (n=18) | Non-viability (n=27) | |||||
| Variable | Baseline | 3 Months | p Value | Baseline | 3 months | p Value |
| EDVI (ml/m2) | 64 (8) | 64 (10) | NS | 61 (12) | 63 (16) | NS |
| ESVI (ml/m2) | 33 (7) | 30 (8) | 0.005 | 29 (11) | 30 (14) | NS |
| Large infarcts | ||||||
| Viability (n=29) | Non-viability (n=33) | |||||
| Values are mean (SD). | ||||||
| *p <0.05 by unpaired Student's t test. | ||||||
| EDVI, end diastolic volume index; ESVI, end systolic volume index. | ||||||
| EDVI (ml/m2) | 63 (8) | 64 (10) | NS | 64 (19) | 71 (22) | <0.001 |
| ESVI (ml/m2) | 33 (8) | 31 (9)* | NS | 35 (17) | 40 (20)* | 0.001 |
Figure 1.
Mean percentage change from baseline in left ventricular end diastolic and end systolic volume indices (EDVI and ESVI) in patients with and without viability, in a subgroup of patients with small (peak creatine kinase ≤ 1000 IU/l) and large (peak creatine kinase > 1000 IU/l) myocardial infarcts.
Left ventricular dilatation
Significant left ventricular dilatation occurred in 23 (21%) of the 107 patients. Clinical and echocardiographic data on patients with and without left ventricular dilatation are summarised in table 3. Patients with dilatation had a larger enzymatic infarct size, more pathological Q waves, and angiotensin converting enzyme (ACE) inhibitors were more often prescribed in this group. Patients with dilatation also had more compromised left ventricular systolic function, both at rest and during low dose dobutamine echocardiography, and less often showed myocardial viability. Both wall motion score indices and the number of akinetic segments were significantly lower on low dose dobutamine echocardiography than at rest in patients without ventricular dilatation (p < 0.0001), but not in patients with dilatation (NS). All those variables were found to be predictive of ventricular dilatation on univariate analysis, while wall motion score index on low dose dobutamine echocardiography was the single best predictor (p < 0.0001; table 4). When multivariate stepwise logistic regression analysis was performed (including all significant baseline variables in the model), only three variables emerged as independent predictors of subsequent ventricular dilatation: myocardial viability, wall motion score index at low dose dobutamine echocardiography, and the number of pathological Q waves (table 4).
Table 3.
Characteristics of patients with and without left ventricular dilatation
| Variable | No dilatation (n=84) | Dilatation (n=23) | p Value |
| Age (years) | 58 (12) | 62 (11) | NS |
| Male | 70 (83%) | 22 (96%) | NS |
| Female | 14 (17%) | 1 (4%) | |
| Anterior myocardial infarction | 39 (46%) | 13 (57%) | NS |
| Inferior myocardial infarction | 45 (54%) | 10 (43%) | NS |
| Previous myocardial infarction | 12 (14%) | 3 (13%) | NS |
| Thrombolytic treatment | 55 (65%) | 17 (74%) | NS |
| Primary PTCA | 10 (12%) | 1 (4%) | NS |
| Number of pathological Q waves* | 1.6 (1.5) | 3.2 (1.7) | <0.0001 |
| Peak creatine kinase (IU/l) | 1372 (1016) | 2449 (1788) | <0.0005 |
| Peak MB fraction (IU/l) | 132 (90) | 209 (118) | <0.001 |
| Drug treatment on hospital discharge | |||
| ACE inhibitors | 33 (39) | 15 (65) | <0.05 |
| Resting echocardiography | |||
| End diastolic volume index (ml/m2) | 62 (3) | 66 (16) | NS |
| End systolic volume index (ml/m2) | 31 (11) | 38 (14) | <0.05 |
| Ejection fraction (%) | 51 (7) | 43 (8) | <0.0005 |
| Wall motion score index | 1.52 (0.24) | 1.75 (0.28) | <0.0005 |
| Number of akinetic segments | 1.8 (1.5) | 2.9 (1.5) | <0.005 |
| Low dose dobutamine echocardiography | |||
| Wall motion score index | 1.43 (0.22) | 1.72 (0.29) | <0.0001 |
| Number of akinetic segments | 1.4 (1.4) | 2.8 (1.5) | <0.0001 |
| Myocardial viability | 43 (51%) | 4 (17%) | <0.01 |
Values are mean (SD) or n (%).
*On the ECG at hospital discharge.
ACE, angiotensin converting enzyme; PTCA, percutaneous transluminal coronary angioplasty.
Table 4.
Logistic regression analysis: predictors of left ventricular dilatation
| Univariate | Multivariate | |||
| Variable | Wald χ2 | p Value | Wald χ2 | p Value |
| Number of pathological Q waves* | 13.12 | 0.0003 | 5.6 | 0.018 |
| Peak creatine kinase (IU/l) | 9.57 | 0.0020 | – | NS |
| Peak MB fraction (IU/l) | 8.69 | 0.0032 | – | NS |
| ACE inhibitors at hospital discharge | 4.69 | 0.0304 | – | NS |
| Resting echo | ||||
| End diastolic volume index (ml/m2) | – | NS | – | |
| End systolic volume index (ml/m2) | 4.52 | 0.0335 | – | NS |
| Ejection fraction (%) | 12.93 | 0.0003 | – | NS |
| Wall motion score index | 12.18 | 0.0005 | – | NS |
| Number of akinetic segments | 8.05 | 0.0046 | – | NS |
| Low dose dobutamine echocardiography | ||||
| Wall motion score index | 16.65 | 0.0000 | 6.2 | 0.013 |
| Number of akinetic segments | 12.27 | 0.0005 | – | NS |
| Myocardial viability | 7.36 | 0.0067 | 5.2 | 0.023 |
*On the ECG at hospital discharge.
DISCUSSION
Myocardial viability and left ventricular dilatation
At rest, most of the left ventricular wall thickening reflects thickening of the inner layer of the myocardium. The middle layer contributes only moderately to overall wall thickening, while the outer third contributes only minimally.16 Thus necrosis predominantly affecting the inner layer may lead to significantly diminished wall thickening at rest. Liebermann and colleagues showed complete loss of systolic wall thickening in dogs with infarction involving more than 20% of the wall thickness, whereas infarcted segments where the transmural extent was less than 20% showed reduced systolic thickening compared with non-infarcted segments.21 Although the middle and outer layers of the myocardium thicken little at rest, they thicken more with catecholamine stimulation and thus contribute to overall wall thickening during dobutamine infusion.17 Thus the presence of dobutamine responsive wall thickening may indicate the presence of viable myocardium in the middle and outer layers of the ventricular wall. Hochman and Bulkley showed in an experimental study that even a small rim of viable epicardial myocardium may be sufficient to prevent or lessen infarct expansion.12 While infarct expansion was common in transmural infarcts, it did not occur in non-transmural infarcts or in infarcts that had only small areas of transmurality with a rim of preserved epicardium surrounding most of the infarct. In addition, Pirolo and colleagues have shown in a large necropsy study that the degree of transmurality was an important predictor of infarct expansion.13 Thus infarct expansion and left ventricular remodelling may occur less in the presence of viable myocardium. Indeed, our study showed preservation of left ventricular volumes in patients with myocardial viability, whereas those without viable myocardium had a significant increase in EDVI and ESVI. Multivariate analysis of our data even showed that the absence of myocardial viability is an independent predictor of ventricular dilatation.
Our data are in line with previous studies. Bolognese and associates found that the extent of infarct zone viability was the most powerful independent predictor of left ventricular dilatation in 93 patients with their first acute myocardial infarct treated by coronary angioplasty.22 Dionisopoulos and colleagues studied 30 patients with Q wave myocardial infarction.23 Although not shown in their results and figures, they concluded that myocardial viability was a strong predictor of left ventricular dilatation.23
Other predictors of ventricular dilatation
Infarct size has been found to be one of the most important determinants of infarct expansion and ventricular remodelling.4–13,24,25 One important difference between our study and that of Bolognese and associates 22 is that in our study infarct size was more significantly related to ventricular dilatation than to myocardial viability. More specifically, left ventricular dilatation did not occur in the subgroup of patients with small infarcts, irrespective of the presence or absence of viability. This is in line with the concept that left ventricular dilatation occurs only after a certain threshold of myocardial damage. Hochman and Bulkley showed in an experimental study that only infarcts involving more than 17% of the left ventricle had infarct expansion.12 In the study of Bolognese and associates, however, ejection fraction and wall motion score index were not predictive of left ventricular dilatation, while peak creatine kinase was less strongly predictive than myocardial viability.22
We showed that wall motion score index on low dose dobutamine echocardiography was more significantly related to ventricular dilatation than was wall motion score index at rest. This is not surprising as wall motion abnormalities at rest may be the result of myocardial necrosis or temporary failure of mechanical function owing to transient ischaemia (referred to as myocardial stunning).26,27 In the latter case there may be contractile reserve which can be demonstrated by dobutamine infusion.28–33 Thus the extent of wall motion abnormalities on low dose dobutamine echocardiography represents the extent of myocardial necrosis (true infarct size) better than the wall motion abnormalities at rest.
Another independent predictor of ventricular dilatation in our study was the number of pathological Q waves. The presence of Q waves on the ECG is often used as a clinical indicator of transmurality, although this criterion is neither sensitive nor specific.34 Previous studies have shown that Q wave infarction is associated with greater transmurality and more remodelling than non-Q wave infarction.11,35,36 Recently, Irimpen and colleagues found in a clinical study of 45 patients that an increase in end diastolic volume index did not occur after non-Q wave infarction.36 After adjustment for infarct size in multivariate analysis, Q wave infarction still added significantly to the prediction of dilatation in that study. In our study, the number of pathological Q waves was more significantly related to ventricular dilatation than was Q wave infarction as such. Thus a large number of Q waves probably reflects both greater transmurality and greater infarct size.
Finally, it has been reported that infarct expansion is more common in patients with anterior infarction.4 Our study had a seemingly paradoxical finding: the group without viability and thus with expansion had predominantly inferior infarcts, while the group with viability and thus without expansion was predominantly composed of anterior infarcts. Subgroup analysis, however, showed that the incidence of left ventricular dilatation in patients with viability was similar in those with anterior and inferior infarcts (7% and 11%, respectively). In those without viability, left ventricular dilatation occurred in 11 patients with anterior infarction (48%) compared with eight patients with inferior infarction (22%, p < 0.05).
Study limitations
One of the limitations of our study was the uncontrolled medical management after myocardial infarction. Patients received drug treatment according to individual need, which remained the responsibility of the attending physician. Hence ACE inhibitors were more often given to patients with large infarcts. As left ventricular dilatation only occurred in those with large infarcts, this produced the paradoxical finding that ACE inhibitors were univariate predictors of left ventricular dilatation. It is not surprising that patients with large infarcts may show an increase in left ventricular volume despite ACE inhibitor treatment. Although ACE inhibition after myocardial infarction limits subsequent ventricular dilatation,37–39 the CATS (captopril and thrombolysis) trial showed that dilatation was not prevented by captopril in the subgroup of patients with a large infarct.39
Furthermore, additional revascularisation procedures before follow up echocardiography could not be standardised. There was a trend towards a larger number of revascularisation procedures in patients with viability (28% v 17%) and in patients without ventricular dilatation (24% v 13%), but these differences were not significant. When analysis was restricted to the 84 patients without revascularisation before the second echocardiogram, there was no essential change in the results. On multivariate regression analysis, wall motion score index at low dose dobutamine echocardiography, myocardial viability, and the number of pathological Q waves remained the independent predictors of ventricular dilatation.
Finally, coronary angiography was not performed routinely in this study. Only 58 (54%) of the 107 patients underwent this procedure, at the discretion of the cardiologist. Both multivessel disease and an occluded infarct related artery were more common in patients with ventricular dilatation than in those without (62% v 42% and 38% v 27%, respectively). The small number of patients, however, limits the detection of differences owing to insufficient statistical power.
Conclusions
Our study shows that the presence of viability early after acute myocardial infarction is associated with preservation of left ventricular size, whereas absence of viability results in ventricular dilatation, particularly in large infarcts. This finding is likely to be of prognostic importance, as mortality increases with increased left ventricular volumes. Carlos and colleagues showed that both large echocardiographic infarct size at low dose dobutamine echocardiography and non-viability were independent predictors of an adverse outcome.40 The same variables were independent predictors of left ventricular dilatation in our present study. Thus large infarct size, absence of viability, left ventricular dilatation, and adverse prognosis are strongly interrelated. Future clinical studies are needed to establish the relative contributions of the absence of viability and ventricular dilatation to adverse prognosis after acute myocardial infarction.
Acknowledgments
We appreciate the great support provided by our technicians Irma Bekkering, Sylvia Bruinzeel, Anja Folkers, and Beatrix Willemsen.
REFERENCES
- 1.White HD, Norris RM, Brown MA, et al. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation 1987;76:44–51. [DOI] [PubMed] [Google Scholar]
- 2.Visser CA, Kan G, Meltzer RS, et al. Incidence, timing and prognostic value of left ventricular aneurysm formation after myocardial infarction: a prospective serial echocardiographic study in 158 patients. Am J Cardiol 1986;57:729–32. [DOI] [PubMed] [Google Scholar]
- 3.Pfeffer MA, Pfeffer JM. Ventricular enlargement and reduced survival after myocardial infarction. Circulation 1987;75(suppl IV):93–7. [PubMed] [Google Scholar]
- 4.Gaudron P, Eilles C, Kugler I, et al. Progressive left ventricular dysfunction and remodeling after myocardial infarction: potential mechanisms and early predictors. Circulation 1993;21:683–91. [DOI] [PubMed] [Google Scholar]
- 5.Bonaduce D, Petretta M, Morgano G, et al. Left ventricular remodeling in the year after myocardial infarction: an echocardiographic, hemodynamic, and radionuclide angiographic study. Coron Artery Dis 1994;5:155–62. [DOI] [PubMed] [Google Scholar]
- 6.Abernethy M, Sharpe N, Smith H, et al. Echocardiographic prediction of left ventricular volume after myocardial infarction. J Am Coll Cardiol 1991;17:1527–32. [DOI] [PubMed] [Google Scholar]
- 7.Assmann PE, Aengevaeren WR, Tijssen JGP, et al. Early identification of patients at risk for significant left ventricular dilation one year after myocardial infarction. J Am Soc Echocardiogr 1995;8:175–84. [DOI] [PubMed] [Google Scholar]
- 8.Chareonthaitawee P, Christian TF, Hirose K, et al. Relation of initial infarct size to extent of left ventricular remodeling in the year after acute myocardial infarction. J Am Coll Cardiol 1995;25:567–73. [DOI] [PubMed] [Google Scholar]
- 9.Peels KH, Visser CA, Dambrink JHE, et al, on behalf of the CATS Investigators Group. Left ventricular wall motion score as an early predictor of left ventricular dilation and mortality after first anterior infarction treated with thrombolysis. Am J Cardiol 1996;77:1149–54. [DOI] [PubMed] [Google Scholar]
- 10.Nijland F, Kamp O, Verheugt FWA, et al. Long-term implications of reocclusion on left ventricular size and function after successful thrombolysis for first anterior myocardial infarction. Circulation 1997;95:111–17. [DOI] [PubMed] [Google Scholar]
- 11.Modena MG, Rossi R, Sgura FA, et al. Early predictors of late dilatation and remodeling after thrombolyzed anterior transmural infarction. Clin Cardiol 1997;20:28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hochman JS, Bulkley BH. Expansion of acute myocardial infarction: an experimental study. Circulation 1982;65:1446–50. [DOI] [PubMed] [Google Scholar]
- 13.Pirolo JS, Hutchins GM, Moore GW. Infarct expansion: pathologic analysis of 204 patients with a single myocardial infarct. J Am Coll Cardiol 1986;7:349–54. [DOI] [PubMed] [Google Scholar]
- 14.Jugdutt BI, Khan MI. Impact of increased infarct transmurality on remodeling and function during healing after anterior myocardial infarction in the dog. Can J Physiol Pharmacol 1992;70:949–58. [DOI] [PubMed] [Google Scholar]
- 15.Touchstone DA, Beller GA, Nygaard TW, et al. Effects of successful intravenous reperfusion therapy on regional myocardial function and geometry in humans: a tomographic assessment using two-dimensional echocardiography. J Am Coll Cardiol 1989;13:1506–13. [DOI] [PubMed] [Google Scholar]
- 16.Myers JH, Stirling MC, Choy M, et al. Direct measurement of inner and outer wall thickening dynamics with epicardial echocardiography. Circulation 1986;74:164–72. [DOI] [PubMed] [Google Scholar]
- 17.Sklenar J, Villanueva FS, Glasheen WP, et al. Dobutamine echocardiography for determining the extent of myocardial salvage after reperfusion: an experimental evaluation. Circulation 1994;90:1503–12. [DOI] [PubMed] [Google Scholar]
- 18.Kan G, Visser CA, Koolen JJ, et al. Short and long term predictive value of admission wall motion score in acute myocardial infarction: a cross sectional echocardiographic study of 345 patients. Br Heart J 1986;56:422–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schiller N, Shah PM, Crawford M, et al. Recommendations for quantification of the left ventricle by two-dimensional echocardiography: American Society of Echocardiography subcommittee on standards. J Am Soc Echocardiogr 1989;2:358–68. [DOI] [PubMed] [Google Scholar]
- 20.Bosch JH, Savalle LH, van Burken G, et al. Evaluation of a semiautomatic contour detection approach in sequences of short-axis two-dimensional echocardiographic images. J Am Soc Echocardiogr 1995;8:810–21. [DOI] [PubMed] [Google Scholar]
- 21.Lieberman AN, Weiss JL, Jugdutt BI, et al. Two-dimensional echocardiography and infarct size: relationship of regional wall motion and thinning to the extent of myocardial infarction in the dog. Circulation 1981;63:739–46. [DOI] [PubMed] [Google Scholar]
- 22.Bolognese L, Cerisano G, Buonamici P, et al. Influence of infarct-zone viability on left ventricular remodeling after acute myocardial infarction. Circulation 1997;96:3353–9. [DOI] [PubMed] [Google Scholar]
- 23.Dionisopoulos P, Smart SC, Sagar KB. Dobutamine stress echocardiography predicts left ventricular remodeling after acute myocardial infarction. J Am Soc Echocardiogr 1999;12:777–84. [DOI] [PubMed] [Google Scholar]
- 24.Lamas GA, Pfeffer MA. Increased left ventricular volume following myocardial infarction in man. Am Heart J 1986;111:30–5. [DOI] [PubMed] [Google Scholar]
- 25.McKay RG, Pfeffer MA, Pasternak RC, et al. Left ventricular remodeling after myocardial infarction: a corollary to infarct expansion. Circulation 1986;74:693–702. [DOI] [PubMed] [Google Scholar]
- 26.Braunwald E, Kloner RA. The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation 1982;66:1146–9. [DOI] [PubMed] [Google Scholar]
- 27.Bolli R. Myocardial stunning in man. Circulation 1992;86:1671–91. [DOI] [PubMed] [Google Scholar]
- 28.Bolli R, Zhu W, Myers ML, et al. Beta-adrenergic stimulation reverses postischemic myocardial dysfunction without producing subsequent functional deterioration. Am J Cardiol 1985;56:964–8. [DOI] [PubMed] [Google Scholar]
- 29.Mercier JC, Lando U, Kammatsuse K, et al. Divergent effects of inotropic stimulation on the ischemic and severely depressed reperfused myocardium. Circulation 1982;66:397–400. [DOI] [PubMed] [Google Scholar]
- 30.Ellis SG, Wynne J, Braunwald E, et al. Response of reperfusion-salvaged, stunned myocardium to inotropic stimulation. Am Heart J 1984;107:13–19. [DOI] [PubMed] [Google Scholar]
- 31.Pierard LA, DeLandsheere CM, Berthe C, et al. Identification of viable myocardium by echocardiography during dobutamine infusion in patients with myocardial infarction after thrombolytic therapy: Comparison with positron emission tomography. J Am Coll Cardiol 1990;15:1021–31. [DOI] [PubMed] [Google Scholar]
- 32.Barilla F, Gheorghiade M, Alam M, et al. Low-dose dobutamine in patients with acute myocardial infarction identifies viable but not contractile myocardium and predicts the magnitude of improvement in wall motion abnormalities in response to coronary revascularization. Am Heart J 1991;122:1522–31. [DOI] [PubMed] [Google Scholar]
- 33.Smart SC, Sawada S, Ryan T, et al. Low-dose dobutamine echocardiography detects reversible dysfunction after thrombolytic therapy of acute myocardial infarction. Circulation 1993;88:405–15. [DOI] [PubMed] [Google Scholar]
- 34.Klein LW, Helfant RH. The Q-wave and non-Q wave myocardial infarction: differences and similarities. Prog Cardiovasc Dis 1986;29:205–20. [DOI] [PubMed] [Google Scholar]
- 35.Jugdutt BI, Tang SB, Khan MI, et al. Functional impact of remodeling during healing after non-Q wave versus Q wave anterior myocardial infarction in the dog. J Am Coll Cardiol 1992;20:722–31. [DOI] [PubMed] [Google Scholar]
- 36.Irimpen AM, Tenaglia AN, Shin DJ, et al. Lack of ventricular remodeling in non-Q wave myocardial infarction. Am Heart J 1996;131:466–71. [DOI] [PubMed] [Google Scholar]
- 37.Pfeffer MA, Lamas GA, Vaughan DE, et al. Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction. N Engl J Med 1988;319:80–6. [DOI] [PubMed] [Google Scholar]
- 38.St John Sutton M, for the SAVE investigators. Quantitative two-dimensional echocardiographic measurements are major predictors of adverse cardiovascular events after acute myocardial infarction. The protective effect of captopril. Circulation 1994;89:68–75. [DOI] [PubMed] [Google Scholar]
- 39.Kingma JH, van Gilst WH, Peels KH, et al, for the CATS Investigators. Acute intervention with captopril during thrombolysis in patients with first anterior myocardial infarction. Eur Heart J 1994;15:898–907. [DOI] [PubMed] [Google Scholar]
- 40.Carlos ME, Smart SC, Wynsen JC, et al. Dobutamine stress echocardiography for risk stratification after myocardial infarction. Circulation 1997;95:1402–10. [DOI] [PubMed] [Google Scholar]