Abstract
Objective: To assess the impact of coronary revascularisation on the health related quality of life (HRQOL) of patients with chronic stable angina compared with data from “community” norms four years following revascularisation.
Design: Prospective survey and review of medical records.
Setting: Seven of the eight public Swedish heart centres that performed coronary artery interventions.
Subjects: 827 patients aged 55–79 years with chronic stable angina who underwent coronary artery revascularisation in 1994 or 1995 and completed the four year HRQOL survey.
Main outcome measures: Five components of the Swedish quality of life survey.
Results: Compared with age and sex adjusted population norms, patients at baseline had significantly lower mean scores on all five functioning and wellbeing scales (p < 0.001). Four years after revascularisation, the mean levels of functioning and wellbeing were similar to those in the normative population (p > 0.05) except for quality of sleep (p < 0.001). The improvements were the same across age groups and for men and women. However, 36% of men and 55% of women were not completely free from angina by four years (p < 0.001). Men without angina after four years had better HRQOL than their community norms (p < 0.001) on all dimensions except quality of sleep (p > 0.05). Women without angina had less pain (p < 0.01) and better general health perception (p < 0.05) but similar physical functioning, quality of sleep, and emotional wellbeing compared with their community counterparts. Both men and women who had suffered at least one anginal attack during the preceding four weeks had significantly worse HRQOL by four years than their community norms (p < 0.01).
Conclusions: By four years following revascularisation, three fifths of patients with chronic stable angina were free of angina and their HRQOL was the same as or better than that of the general Swedish population. However, fewer than half of all women and two thirds of men who underwent revascularisation were angina-free after four years. Among patients with new or persistent angina, the HRQOL was worse than that in community norms.
Keywords: coronary artery bypass graft surgery, percutaneous transluminal coronary angioplasty, coronary artery revascularisation, quality of life, outcomes
Randomised controlled trials have shown that coronary artery bypass graft (CABG) surgery improves survival for patients with severe coronary artery disease. Patients with less severe disease often elect to undergo coronary revascularisation to reduce their angina and to improve their quality of life. An important question for these patients, and for their physicians, is how effective will coronary intervention be in improving their quality of life?
The quality of life of patients with coronary artery disease may be assessed with a variety of validated instruments. Some of these instruments, such as the Seattle angina questionnaire1 and the physical activity score,2 are specific for coronary disease. Others, such as the medical outcomes study short form 36,3 the Nottingham health profile (NHP),4 and the Swedish quality of life survey (SWED-QUAL),5 provide a more generic assessment and allow comparisons with normal populations.
Although there have been several reports on the quality of life of patients following coronary revascularisation,6–12 there have been few reports comparing the outcomes in these patients with population norms and, when they have been done, they often represent very select populations.13–15 Brown and colleagues16 compared the functioning and wellbeing of myocardial infarction survivors with normative data and found that patients under age 65 years had lower scores and those over age 65 had similar scores compared with community norms.
As part of the SECOR/SBU (Swedish coronary revascularisation-Swedish Council on Technology Assessment) study, a prospective study to assess the appropriateness of the use of coronary revascularisation, we examined the quality of life of a population based cohort of Swedish patients who underwent revascularisation through a four year follow up. We examined whether the functioning and wellbeing of patients with chronic stable angina improved to a level similar to that of the general Swedish population.
METHODS
Patients
The SECOR/SBU study design and data collection have been reported previously.17 In brief, we screened 4398 patients who underwent coronary angiography in seven of the eight public Swedish heart centres in 1994 and 1995. Patients were excluded if they declined to participate or deferred intervention (n = 62), had a previous CABG (n = 291), had undergone percutaneous transluminal coronary angioplasty (PTCA) within the previous six months (n = 184), were referred for evaluation of congestive heart failure, arrhythmia, or possible cardiac transplantation (n = 62), had valvar heart disease and were considered candidates for valve surgery (n = 528), had emergency coronary angiography (n = 187), were referred for further evaluation (n = 44), were non-Swedish residents (n = 72), had incomplete medical data (n = 113), or were enrolled in other research projects (n = 88). Of the remaining 2767 patients we also excluded those with unstable angina or those who had within 21 days had a myocardial infarction (n = 650), asymptomatic patients (n = 89), and chronically ill stable patients referred for medical treatment (n = 543). For comparison with the population norms we also excluded patients who were younger than 55 years or older than 79 at the time of study entry (n = 343). The remaining 1142 patients with chronic stable angina were asked to participate in this observational study and to complete standardised questionnaires regarding their symptoms, functioning, and wellbeing before coronary angiography and six months, 21 months, and four years following revascularisation. This report focuses on a comparison between baseline and four year results. Among the 1013 patients (88.7%) who answered the baseline questionnaire, 757 had undergone CABG and 256 had undergone PTCA. For this report, we combined the patients who received CABG and PTCA into a single group since we previously found that by four years following revascularisation there were no differences in health related quality of life (HRQOL) between patients who underwent these procedures.10
Patients who died were identified by computerised linkage to the Swedish national population register. Patients who underwent further interventions within the first two years of follow up were identified by computerised linkage to the Swedish national discharge register. The regional ethics committee at the Karolinska Hospital, Stockholm, approved the study.
Normative population
We assessed functioning and wellbeing in a random cross sectional sample of the Swedish population aged 55–79 years drawn in 1995 from the Swedish general population address register kept by Statistics Sweden. Three strata of equal size for the age groups 55–64, 65–74, and 75–84 years were used for the data collection, and we used 884 respondents to compare with the SECOR/SBU patient group.
Data collection: medical records
We collected each patient's relevant clinical and laboratory information using a standardised form. Data collection started when patients were referred for coronary angiography by their cardiologist. The cardiologist entered the patient's clinical and sociodemographic characteristics. Further information such as the severity of the coronary artery disease was collected by the study team following coronary angiography. All terms were explicitly defined and have been previously published.17,18 Data were reviewed for completeness and accuracy before being entered into a computerised database.
Data collection: patient questionnaires
Patients assessed the frequency of their anginal symptoms on a six point Likert scale ranging from none to four or more times a day during the preceding four weeks. Frequent angina was defined as angina three or more times a week during the preceding four weeks. The patients' health related functioning and wellbeing were assessed with five components of the SWED-QUAL5: (a) physical functioning, a seven item scale that assesses ability to perform physical activities; (b) relief from pain, a six item scale that measures relief from physical discomfort; (c) quality of sleep, a six item scale that addresses problems with sleep initiation, maintenance, and adequacy and with somnolence; (d) emotional wellbeing, a 12 item scale that assesses positive and negative affect; and (e) a single item question assessing the patient's general health perception. The scores on each scale ranged from 0–100 with higher scores reflecting better health. The Cronbach's α of the multi-item scales ranged from 0.80–0.88.5
Statistical analysis
All comparisons of functioning and wellbeing were based on patients that responded to the baseline and four year follow up questionnaires. There are concerns that coronary revascularisation may have a differential effect on HRQOL depending on the patient's age or sex.19–23 We therefore conducted a series of analyses specifically designed to answer these questions. For this, we divided patients into three age groups based on their age at the time of study entry: 55–62, 63–70, and 71–79 years.
For ordinal variables we used the χ2 statistic and when variables were binary we used Fisher's exact test. Univariate GLM (general linear model) was used for comparisons of functioning and wellbeing. As factors we included population (patient or population sample), sex, and age group (full model). All tests were two tailed and adjusted for multiple comparisons according to Bonferroni. All statistics were calculated using the SPSS 10.1 (SPSS Inc, Chicago, Illinois) computer program.
RESULTS
Among the 1013 patients who answered the baseline questionnaire, 827 (82%) completed the four year follow up questionnaire. Fifty nine patients (6%) died during follow up and 127 of the survivors (13%) did not respond to the four year survey. Among responders, 649 were men and 178 were women.
Before entry into the study, significantly more of those who later died had sustained a myocardial infarction, peripheral vascular disease, congestive heart failure, or reduced left ventricular function (p < 0.01 for all comparisons). Surviving responders and non-responders had a history of myocardial infarction, symptom severity (according to the Canadian Cardiovascular Society classification system),24 and angina frequency similar to those reported by the patients (p > 0.05). While there was a trend towards higher comorbidity among non-responders the only significant differences were a higher rate of stroke or transient ischaemic attack (p < 0.001) and worse physical functioning (p < 0.05) (table 1).
Table 1.
Characteristics of Swedish patients with chronic stable angina who underwent coronary revascularisation and survived at least four years, by response to four year follow up questionnaire
| Characteristic | Responders to baseline and four year questionnaire (n=827) | Surviving non-responders to four year questionnaire (n=127) | p Value |
| Mean age (years) | 66.0 | 66.6 | 0.33 |
| Male sex (%) | 78.5 | 73.2 | 0.19 |
| Angina class III/IV* (%) | 60.1 | 59.1 | 0.82 |
| Comorbid illness (%) | |||
| Prior myocardial infarction | 43.2 | 46.5 | 0.49 |
| Diabetes mellitus | 16.2 | 22.0 | 0.10 |
| Stroke/transient ischaemic attack | 6.7 | 16.5 | < 0.001 |
| Renal disease | 1.5 | 3.1 | 0.17 |
| Peripheral vascular disease | 7.5 | 10.2 | 0.29 |
| Congestive heart failure | 8.6 | 12.6 | 0.14 |
| Chronic obstructive lung disease | 3.9 | 4.7 | 0.65 |
| Hypertension | 37.4 | 46.5 | 0.05 |
| Very positive stress test | 69.3 | 69.4 | 0.98 |
| Left ventricular ejection fraction <50% | 23.8 | 26.0 | 0.60 |
| Severity of coronary artery disease (%) | 0.21 | ||
| Left main or 3 vessel stenosis | 55.6 | 52.8 | |
| 1 or 2 vessel stenosis involving the PLAD | 18.3 | 14.2 | |
| 1 or 2 vessel stenosis not involving PLAD | 26.1 | 33.1 | |
| Angina frequency and HRQOL | |||
| Angina attacks ≥3 times a week | 69.5 | 68.5 | 0.82 |
| Physical functioning | 69.9 | 66.2 | 0.03 |
| Relief from pain | 63.2 | 60.8 | 0.27 |
| Quality of sleep | 57.2 | 57.5 | 0.89 |
| Emotional wellbeing | 66.1 | 63.6 | 0.26 |
| General health perception | 55.6 | 52.2 | 0.12 |
*Angina class as defined by the Canadian Cardiovascular Society. HRQOL, health related quality of life (minimum score is 0; maximum score is 100); PLAD, proximal left anterior descending coronary artery.
Patients who had surgery and angioplasty differed with respect to subsequent interventions. Within two years after the primary intervention, 2% of the 615 surgical patients and 33.5% of the 212 angioplasty patients had undergone additional revascularisation procedures (p < 0.001). At both the six month and the 21 month follow up surveys, surgical patients reported significantly better physical functioning (p < 0.01), less pain (p < 0.01), better quality of sleep (p < 0.05), and a more positive general health perception (p < 0.001), but similar emotional wellbeing compared with angioplasty patients. These results are in accord with previously published results from this study on patients with one or two vessel disease.10 However, since there were no significant differences at baseline or four years in functioning and wellbeing between patients referred for CABG and those referred for PTCA (p > 0.05), we present the results for all patients who underwent revascularisation as one group.
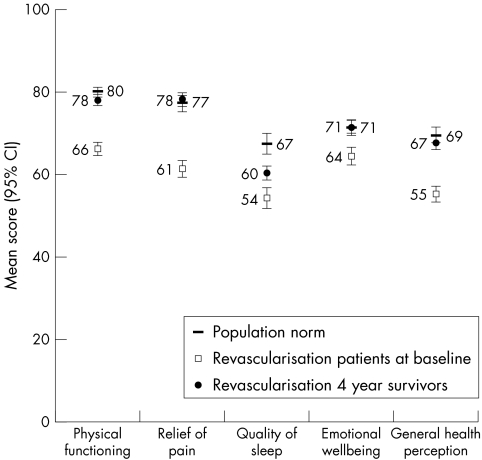
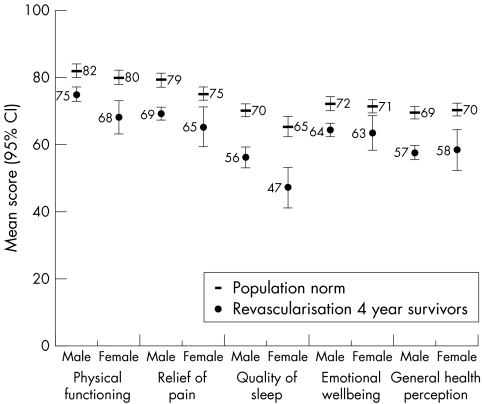
Comparison of HRQOL of patients with population norms
Figure 1 shows the mean HRQOL scores (and their 95% confidence intervals) of patients with chronic stable angina who survived four years following coronary revascularisation compared with Swedish population norms adjusted for age and sex. At baseline, before revascularisation, the patients' mean scores on all domains were substantially lower, implying poorer quality of life, than Swedish population norms (p < 0.001). The mean difference in scores ranged from 13–16 points on a 100 point scale for four of the five domains. A smaller difference was found for the domain of emotional wellbeing. By the four year follow up, the levels of functioning and wellbeing among patients had improved to the same level as population norms (p > 0.05) for all domains except quality of sleep, which was still lower than community norms (p < 0.001). The level of improvement we found in physical functioning, increasing from 66 at baseline to 78 at four year follow up, would have occurred if the proportion of respondents who either could not walk 100 m or could walk that distance only with difficulty before revascularisation were able to walk that same distance without difficulty following revascularisation.
Figure 1.
Mean (95% confidence interval (CI)) Swedish quality of life survey (SWED-QUAL) scores at baseline and by four years for patients with chronic stable angina who had undergone coronary revascularisation compared with age and sex adjusted Swedish norms (minimum score is 0; maximum score is 100).
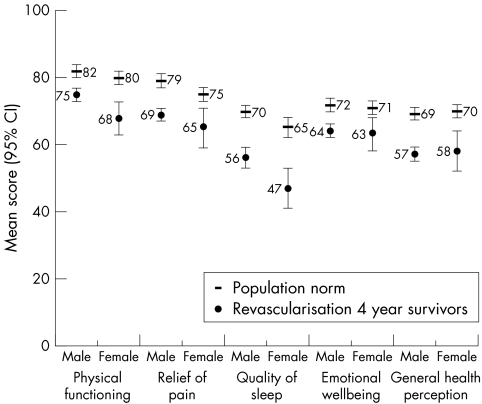
Subgroup analysis by sex
We next examined whether there were any differences between the patients who had undergone revascularisation and the normative population by sex while controlling for age differences. At baseline, both male and female patients had significantly lower mean scores for all HRQOL domains than their population norms (p < 0.001). By four years, male and female patients reported levels of relief of pain, emotional wellbeing, and general health perception similar to the population norm (p > 0.05). However, male patients reported significantly better physical functioning (p < 0.05) and female patients significantly worse physical functioning (p < 0.05) than the population norm.
Subgroup analysis by age
We then compared patients' HRQOL by age group (that is, ages 55–62, 63–70, and 71–79 years) with that of the population norm while controlling for sex. We found that patients, irrespective of age group, had systematically lower scores at baseline (p < 0.001). By four years, with the exception of quality of sleep, which was still lower among patients aged 63 or older (p < 0.05), and emotional wellbeing, which was lower in those aged 63–70 years (p < 0.05), there were no longer any significant differences in HRQOL between patients and the normative population (p > 0.05).
Effect of angina on HRQOL
Before revascularisation, 97% of patients were classified as having Canadian Cardiovascular Society angina class II or higher by their cardiologist. At the same time, 98% of patients reported that they had had angina attacks at least once during the preceding four weeks and 68% reported frequent angina (angina three or more times a week). By four years, 60% of patients reported that they were free from angina, 28% that they had angina fewer than three times a week, and 12% that they had frequent angina (p < 0.001).
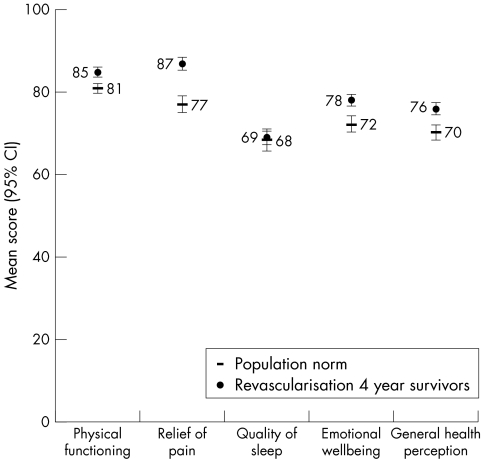
When we compared HRQOL by angina frequency among patients, we found a strong effect on all five HRQOL domains (p < 0.001) (table 2). For example, mean physical functioning among patients without angina during the preceding four weeks was 88 compared with 76 among those with angina fewer than three times a week and 66 among those with frequent angina (p < 0.001). Compared with age and sex adjusted population norms, patients without angina had better physical functioning (85 v 81, p < 0.001) while those with angina had worse physical functioning (71 v 81, p < 0.001). Figures 2 and 3 show these results. We found similar relations between the other four HRQOL measures and angina status.
Table 2.
Relation between frequency of angina and mean Swedish quality of life survey (SWED-QUAL) scores (minimum score is 0; maximum score is 100) among Swedish patients with chronic stable angina four years following coronary revascularisation
| Frequency of angina during preceding four weeks | ||||
| Questionnaire component | None | <3 a week | ≥3 a week | p Value |
| Physical functioning | 88 | 76 | 66 | <0.001 |
| Relief from pain | 90 | 74 | 52 | <0.001 |
| Quality of sleep | 70 | 57 | 44 | <0.001 |
| Emotional wellbeing | 79 | 67 | 58 | <0.001 |
| General health perception | 76 | 62 | 46 | <0.001 |
Figure 2.
Mean (95% CI) SWED-QUAL scores for patients with chronic stable angina who had undergone coronary revascularisation and reported no angina at the four year follow up compared with age and sex adjusted Swedish norms (minimum score is 0; maximum score is 100).
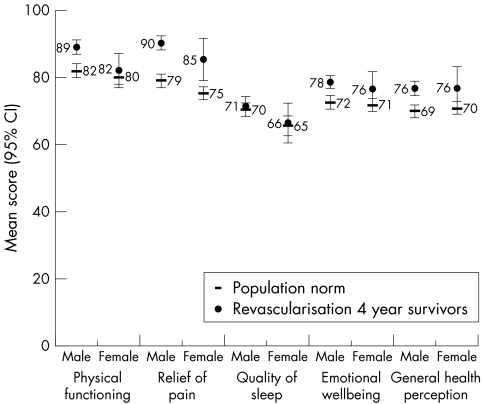
Figure 3.
Mean (95% CI) SWED-QUAL scores for patients with chronic stable angina who had undergone coronary revascularisation and reported angina at the four year follow up compared with age and sex adjusted Swedish norms (minimum score is 0; maximum score is 100).
By four years, more female than male patients had angina (55% v 36%, p < 0.001). Male patients without angina had better HRQOL than the population norm for males (p < 0.001) on all scales but quality of sleep (p > 0.05) (fig 4). Female patients without angina had less pain (p < 0.01) and better general health perception (p < 0.05) but similar physical functioning, quality of sleep, and emotional wellbeing compared with their population counterparts.
Figure 4.
Mean (95% CI) SWED-QUAL scores for patients with chronic stable angina who had undergone coronary revascularisation and reported no angina at the four year follow up compared with age adjusted Swedish norms, by sex (minimum score is 0; maximum score is 100).
Both male and female patients who had experienced at least one anginal attack during the preceding four weeks had significantly worse HRQOL by four years than their population norms (p < 0.01) (fig 5). The strong effect of angina was also present when we compared age groups. Irrespective of age group, patients without angina had similar or better HRQOL and patients with angina had similar or worse HRQOL compared with the population norm. Table 3 summarises the results of the comparisons by sex and age group. Female patients with and without angina had lower physical functioning scores than male patients four years following revascularisation (p < 0.01 for all comparisons). There were no significant differences between male and female patients for the other four HRQOL domains.
Figure 5.
Mean (95% CI) SWED-QUAL scores for patients with chronic stable angina who had undergone coronary revascularisation and reported angina at the four year follow up compared with age adjusted Swedish norms, by sex (minimum score is 0; maximum score is 100).
Table 3.
Summary of statistical tests of differences in HRQOL between Swedish population norms and patients with chronic stable angina who underwent coronary revascularisation, by angina status, sex, and age four years following revascularisation
| Characteristics of patients | Physical functioning | Relief from pain | Quality of sleep | Emotional wellbeing | General health perception |
| No angina | |||||
| Men | ↑↑↑ | ↑↑↑ | = | ↑↑↑ | ↑↑↑ |
| Women | = | ↑↑ | = | = | |
| Age 55–62 | = | ↑ | = | = | ↑ |
| Age 63–70 | = | ↑↑↑ | = | ↑ | ↑ |
| Age 71–79 | = | ↑↑ | = | ↑ | ↑ |
| All | ↑↑ | ↑↑↑ | = | ↑↑↑ | ↑↑↑ |
| Angina | |||||
| Men | ↓↓↓ | ↓↓↓ | ↓↓↓ | ↓↓↓ | ↓↓↓ |
| Women | ↓↓↓ | ↓↓ | ↓↓↓ | ↓↓ | ↓↓↓ |
| Age 55–62 | ↓↓↓ | ↓↓ | ↓↓↓ | ↓↓ | ↓↓↓ |
| Age 63–70 | ↓↓↓ | ↓↓↓ | ↓↓↓ | = | ↓↓↓ |
| Age 71–79 | ↓↓ | ↓↓ | ↓↓↓ | ↓↓ | ↓↓↓ |
| All | ↓↓↓ | ↓↓↓ | ↓↓↓ | ↓↓↓ | ↓↓↓ |
↑, patients have significantly better HRQOL than population norm;↓, patients have significantly worse HRQOL than population norm. ↑↑↑, ↓↓↓, p<0.001; ↑↑, ↓↓ p<0.01; ↑, ↓ p<0.05; =, p>0.05.
DISCUSSION
In this study we compared the health related functioning and wellbeing of Swedish patients with chronic stable angina aged 55–79 years at the time of intervention and four years following coronary revascularisation with those of a population based cross sectional cohort of Swedish citizens. We found that patients improved their HRQOL to levels similar to population norms in four of the five domains examined in the four year follow up. The exception was quality of sleep, which was still found to be significantly lower among patients. Our results are similar to three other reports in the literature comparing patients undergoing coronary revascularisation with population norms. Krumholtz and colleagues14 found that the pre-PTCA scores of 98 patients were well below the national norm and that six months following PTCA scores were at least as high as the norm. Caine and associates13 examined five year outcomes after elective bypass surgery of 84 male patients who were age 60 or younger at the time of surgery. These patients were found to have similar functioning to a general population sample in the six major domains from part I of the NHP. Pocock and colleagues15 reported on the three year follow up of 1011 patients randomised to angioplasty or bypass surgery in the RITA (randomized intervention treatment of angina) trial. The majority of these patients, who were free from angina, had NHP mean scores similar to the population norm.
We also found that the HRQOL patients achieve following revascularisation is strongly influenced by whether they experience angina. In our study, patients who experienced angina had lower HRQOL scores than community norms while those without angina had higher scores. More than half the women in our study had angina on four year follow up compared with one third of the men. Similar findings have been reported regarding patients who have undergone revascularisation.15
In contrast to a study from western Sweden, which reported that men experienced better HRQOL than women following revascularisation,8,25 we found similar outcomes after controlling for angina and age. Although the HRQOL scores for men in our study, irrespective of anginal status, were generally higher than for women, these differences reached significance only for physical functioning. This makes intuitive sense since the scale that measures physical functioning includes questions such as “Can [you] perform strenuous activities (such as heavy manual work, strenuous sports) without difficulty?” There may be several explanations for these contrasting results. Our study was restricted to patients with chronic stable angina and we followed outcomes through four years. The western Swedish study included all patients who underwent bypass surgery, except those also receiving valve surgery, and outcomes were followed for only two years. In addition, the western Swedish population had a much higher prevalence of left main or three vessel coronary artery disease than our patients (80% v 55%). Thus, their population was less homogeneous, had more severe disease, and was followed for less time.
One unique finding of our study was that the quality of sleep was the same for patients without angina and the population norm. This was in contrast to the better HRQOL in the other four domains for patients without angina compared than community norms. Among patients with angina, the quality of sleep was significantly worse than community norms. This may indicate that the adverse quality of sleep experienced by patients with angina is a direct effect of their angina while their quality of sleep in patients without angina is not improved compared with community norms.
Patients may also be interested in other outcomes such as cognitive function, employment, and sexual function. Health care administrators and public health specialists might be interested in the relation between a patient's social class and educational status and the outcomes they experience. Physicians may wonder how effective medical treatment was in those patients not referred for revascularisation since aggressive lipid lowering therapy has been found to be as effective as angioplasty and usual care in patients at low risk with stable coronary artery disease.26 Unfortunately, we could not address these issues in this study.
Ultimately, the question that we must address is how this information will best help us to make decisions in the future. Health care decision making, whether by the patient or the physician, is relying to ever greater degrees on the evidence we find in clinical research. We already know that patients with severe coronary artery disease achieve better outcomes with bypass surgery than with medical treatment. Among patients with disease treatable by both bypass surgery and PTCA, pain relief is greater with bypass surgery and there is less chance of undergoing a second revascularisation procedure. Our study extends these findings by providing detailed outcomes data for patients with chronic stable angina, the most common indication for revascularisation in Sweden and many other countries, who could be treated by bypass surgery or angioplasty.
We may counsel patients that by four years after revascularisation, three fifths of them will be free of angina and more than one quarter will experience angina fewer than three times a week. The quality of life for patients without angina will actually be better than or similar to that of people in the community. However, fewer than half of all women and two thirds of men who undergo revascularisation will be angina-free after four years.
Acknowledgments
The SECOR/SBU project was supported by grants from the Swedish Medical Research Council and the Swedish Federation of County Councils. We thank Ann-Sofie Nord, who coordinated data collection at SBU. We are especially grateful to the patients who agreed to participate in this study. Dr Bernstein was partially supported by grants from the Dirección General de Enseñanza Superior e Investigación Científica of the Spanish Ministry of Education and Culture (SAB1999–0100) and Programa Cátedra Fundación BBV, Spain.
SECOR/SBU project group: Lars Werkö MD (chairman); Bengt Brorsson PhD (principal investigator); Nina Rehnqvist MD; Olof Edhag MD; Håkan Emanuelsson MD; Ulf Haglund MD; Kjell Rådegran MD; Göran Stenport MD; Egon Jonsson PhD; Gunilla Lamnevik BSc; and Torkel Åberg MD.
SECOR/SBU investigators: Carl Gunnar Gustavsson MD, Carina Wendel RN (Lund University Hospital; Lars Ohlsson (deceased) MD, Mikael Kehler MD (Karlskrona Hospital); Kjell Jansson MD, Christina Wikström RN (Linköping University Hospital); Per Albertsson MD, Marie Carlsson RN (Sahlgrenska University Hospital, Östra Hospital, Skövde Hospital, Uddevalla Hospital, Norra Älvsborg Hospital, Borås Hospital and Varberg Hospital); Stella Scizinsky MD, Gunilla Forsell MD, Birgitta Grape RN (Karolinska University Hospital); Carl-Göran Ericsson MD, Margret Lundström RN (Danderyd Hospital); Inger Axelsson MD, Curt Thorstrand MD (South Hospital); Bo Lindvall MD (Huddinge University Hospital); Christina Stafberg MD, Lena Jideus MD, Jenny Kjellgren RN (Uppsala University Hospital); Helge Saetre MD, Britt-Marie Nilsson RN (Falu Hospital); Stellan Bandh MD, Inger Alexandersson RN (Västerås Hospital); Gunnar Gustafsson MD (Gävle Hospital); Jan Hellström MD, Hans Petter Ildgruben MD, Margaretha Ritfeldh RN (Norrland University Hospital); Håkan Forsberg MD, Birgitta Palmreidh RN (Boden Hospital); and Bengt Möller MD, Carina Lundblom RA (Sundsvall Hospital).
Abbreviations
CABG, coronary artery bypass graft
HRQOL, health related quality of life
NHP, Nottingham health profile
PTCA, percutaneous transluminal coronary angioplasty
RITA, randomized intervention treatment of angina
SECOR/SBU, Swedish coronary revascularisation—Swedish Council on Technology Assessment
SWED-QUAL, Swedish quality of life survey
REFERENCES
- 1.Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle angina questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol 1995;25:333–41. [DOI] [PubMed] [Google Scholar]
- 2.Wilson A, Wiklund I, Lahti T, et al. A summary index for the assessment of quality of life in angina pectoris. J Clin Epidemiol 1991;44:981–8. [DOI] [PubMed] [Google Scholar]
- 3.Ware JE, Sherbourne CD. The MOS 36-item short form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 4.Hunt SM, McEwen J, McKenna SP. Measuring health status. London: Croom Helm, 1986.
- 5.Brorsson B, Ifver J, Hays RD. The Swedish health-related quality of life survey (SWED-QUAL). Qual Life Res 1993;2:33–45. [DOI] [PubMed] [Google Scholar]
- 6.Cleary PD, Epstein AM, Oster G, et al. Health-related quality of life among patients undergoing percutaneous transluminal coronary angioplasty. Med Care 1991;29:939–51. [DOI] [PubMed] [Google Scholar]
- 7.Wahrborg P, on behalf of the CABRI trialists. Quality of life after coronary angioplasty or bypass surgery. 1-year follow-up in the coronary angioplasty versus bypass revascularization investigation (CABRI) trial. Eur Heart J 1999;20:653–8. [DOI] [PubMed] [Google Scholar]
- 8.Herlitz J, Wiklund I, Caidahl K, et al. Determinants of an impaired quality of life five years after coronary artery bypass surgery. Heart 1999;81:342–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nash IS, Curtis LH, Rubin H. Predictors of patient-reported physical and mental healtrh 6 months after percutaneous coronary revascularization. Am Heart J 1999;138:422–9. [DOI] [PubMed] [Google Scholar]
- 10.Brorsson B, Bernstein SJ, Brook RH, et al. Quality of life of chronic stable angina patients 4 years after coronary angioplasty or coronary artery bypass surgery. J Intern Med 2001;249:47–57. [DOI] [PubMed] [Google Scholar]
- 11.Engblom E, Korpilahti K, Hamalainen H, et al. Quality of life and return to work 5 years after coronary artery bypass surgery: long-term results of cardiac rehabilitation. J Cardiopulm Rehabil 1997;17:29–36. [DOI] [PubMed] [Google Scholar]
- 12.BARI. Five-year clinical and functional outcome comparing bypass surgery and angioplasty in patients with multivessel coronary disease: a multicenter randomized trial. Writing group for the bypass angioplasty revascularization investigation (BARI) investigators. JAMA 1997;277:715–21. [PubMed] [Google Scholar]
- 13.Caine N, Sharples LD, Wallwork J. Prospective study of health related quality of life before and after coronary artery bypass grafting: outcome at five years. Heart 1999;81:347–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krumholtz HM, McHorney CA, Clark L, et al. Changes in health after elective percutaneous coronary revascularization. Med Care 1996;34:754–9. [DOI] [PubMed] [Google Scholar]
- 15.Pocock SJ, Henderson RA, Seed P, et al. Quality of life, employment status, and anginal symptoms after coronary angioplasty or bypass surgery. 3-year follow-up in the randomized intervention treatment of angina (RITA) trial. Circulation 1996;94:135–42. [DOI] [PubMed] [Google Scholar]
- 16.Brown N, Melville M, Gray D, et al. Quality of life four years after acute myocardial infarction: short form 36 scores compared with a normal population. Heart 1999;81:352–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernstein SJ, Brorsson B, Åberg T, et al, on behalf of the SECOR/SBU project group. The appropriateness of referral of coronary angiography patients in Sweden. Heart 1999;81:470–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johansson SR, Brorsson B, Bernstein SJ. Coronary artery bypass graft and percutaneous transluminal coronary angioplasty. Report no 120E. Stockholm: Swedish Council on Technology Assessment in Health Care, 1994.
- 19.Peigh PS, Swartz MT, Vaca KJ, et al. Effect of advancing age on cost and outcome of coronary artery bypass grafting. Ann Thorac Surg 1994;58:1362–6. [DOI] [PubMed] [Google Scholar]
- 20.Lindsay J Jr, Reddy VM, Pinnow EE, et al. Morbidity and mortality rates in elderly patients undergoing percutaneous transluminal coronary angioplasty. Am Heart J 1994;128:697–702. [DOI] [PubMed] [Google Scholar]
- 21.Arnold AM, Mick MJ, Piedmonte MR, et al. Gender differences for coronary angioplasty. Am J Cardiol 1994;74:18–21. [DOI] [PubMed] [Google Scholar]
- 22.Sjoland H, Caidahl K, Wiklund I, et al. Effects of age on quality of life before and after coronary bypass grafting. Cardiol Elder 1996;4:195–200. [Google Scholar]
- 23.Bell MR, Grill DE, Garratt KN, et al. Long-term outcome of women compared with men after successful coronary angioplasty. Circulation 1995;91:2876–81. [DOI] [PubMed] [Google Scholar]
- 24.Campeau L. Grading of angina pectoris. [letter] Circulation 1976;54:522–3. [PubMed] [Google Scholar]
- 25.Sjoland H, Wiklund K, Caidahl K, et al. Improvement in quality of life differs between women and men after coronary artery bypass surgery. J Intern Med 1999;245:445–54. [DOI] [PubMed] [Google Scholar]
- 26.Pitt B, Waters D, Brown WV, et al. Aggressive lipid lowering therapy compared with angioplasty in stable coronary artery disease. N Engl J Med 1999;341:70–6. [DOI] [PubMed] [Google Scholar]