Abstract
Objective: To examine the impact of previously operated complex congenital heart disease on health related quality of life and subjective health status and to determine the relation between these parameters and physical status.
Design: Cross sectional; information on medical follow up was sought retrospectively.
Setting: Patients were randomly selected from the archives of the paediatric cardiology department, Leiden University Medical Centre, Leiden, The Netherlands, and approached irrespective of current cardiac care or hospital of follow up.
Patients: Seventy eight patients with previously operated complex congenital heart disease (now aged 18–32 years) were compared with the general population.
Main outcome measures: Health related quality of life was determined with a specifically developed questionnaire (Netherlands Organisation for Applied Scientific Research Academic Medical Centre (TNO-AZL) adult quality of life (TAAQOL)) and subjective health status was assessed with the 36 item short form health survey (SF-36). Physical status was determined with the objective physical index, Somerville index, and New York Heart Association functional class.
Results: Health related quality of life of the patients was significantly worse than that of the general population in the dimensions gross motor functioning and vitality (p < 0.01). Correlations between health related quality of life and physical status were poor. Patients had significantly worse subjective health status than the general population in the dimensions physical functioning, role functioning physical, vitality, and general health perceptions (p < 0.01). Correlations between subjective health status and physical indices were weak.
Conclusion: Adult survivors with previously operated complex congenital heart disease experienced limitations only in the physical dimensions of health related quality of life and subjective health status. Objectively measured medical variables were only weakly related to health related quality of life. These results indicate that, when evaluating health related quality of life, dedicated questionnaires such as the TAAQOL should be used.
Keywords: complex congenital heart disease, health related quality of life, physical status
A dvances in surgery and intensive care have increased the life expectancy of children with complex congenital heart disease. Therefore, it is important to assess the long term results of treatment of these patients, not only in medical terms (for example, morbidity and mortality) but also in terms of health related quality of life and subjective health status. Since a longer life does not necessarily mean a better life, knowledge of the emotional response to health status problems may allow identification of areas of daily life that need to be improved (for example, by medical care or by provisions in social or infrastructural care management). Moreover, patients' satisfaction with the medical consultation may increase if physicians assess a patient's general wellbeing, as well as functional status.1 Some studies have explored the subjective health status of patients with congenital heart disease in adulthood2–10 but none have examined health related quality of life using a clear definition. In addition, correlating health related quality of life with the patient's physical condition may increase our understanding of the concept of health related quality of life.11
Therefore, in a group of patients with previously operated complex congenital heart disease, the aim of the study was, firstly, to compare patients' health related quality of life and subjective health status with those of the general Dutch population (age and sex matched) and, secondly, to relate health related quality of life and subjective health status to physical status.
METHODS
The study was approved by the local medical ethical committee and informed consent was obtained from each participant. A cross sectional design was used and information on medical follow up was searched for retrospectively.
Definitions
Health related quality of life
Although there is no universal definition for health related quality of life, there is growing consensus that it should be assessed multidimensionally, including physical health, psychological state, and social relationships.12–15 Moreover, quality of life and health status are distinct constructs12,16,17; quality of life is determined not only by the patient's health status problems but also by the emotional response to these problems. To measure quality of life according to this definition, quality of life questionnaires have been developed for children (Netherlands Organisation for Applied Scientific Research Academic Medical Centre (TNO-AZL) child quality of life TACQOL questionnaire14,18) and for adults (TNO-AZL adult quality of life (TAAQOL) questionnaire19). Both questionnaires have been validated in the general population as well as in patients with various chronic diseases, such as minor congenital heart disease.14,18–21Fig 1 shows an example of the format of the questionnaires. Health related quality of life is used since non-health factors such as income or housing (which may also contribute to quality of life) were not taken into account. For clinicians health related quality of life is most relevant.
Figure 1.
Example of the format of the health related quality of life questionnaire: TNO-AZL (adult/child) quality of life (TAxQOL).
The 36 item short form health survey (SF-36) is widely used and thoroughly validated.22,23 It measures subjective health status, posing such questions as “What are your limitations?” or “Do you feel healthy?” in contrast to “How do you feel about certain limitations?” in the TAAQOL.
Diagnosis
In the present study, patients with previously operated complex congenital heart disease were approached, excluding those who had undergone anatomical corrective surgery. All patients included in this study had undergone a non-anatomical correction—that is, partial or complete cavopulmonary connection, venous switch for transposition of the great arteries, or a correction with the use of allogenous tissue (for example, Rastelli correction, insertion of a mechanical valve). The main common characteristic was that postoperatively none of the participants had an anatomically normal heart as described by the segmental analysis,24 as opposed to patients after anatomical corrective surgery (for example, operated ventricular or atrial septal defects, coarctation of the aorta, patent ductus arteriosus, uncomplicated tetralogy of Fallot, total anomalous pulmonary venous connection, and uncomplicated pulmonary or aortic stenosis).
Patient selection
To prevent selection bias, patients were selected from the archives of the department of paediatric cardiology, Leiden University Medical Centre, Leiden, The Netherlands, which has complete information on patients seen from 1950 onwards. From these files, 4383 patients were born between 1968 and 1982. Of these, in the year 1999, 2280 were randomly selected. Then, 251 patients with operated complex congenital heart disease were included and further studied irrespective of current cardiac surveillance. The latest medical information and home addresses were obtained from the most recent medical file, general practitioners, or local authorities. Among the 251 included patients, 123 (49%) had died. Others (n = 41) were excluded for the following reasons: they were not living in the Netherlands or did not speak Dutch n = 28 (11%), they had learning disabilities n = 12 (5%), or they had participated in a pilot study n = 1 (0.5%). One patient was lost to follow up. The remaining 86 patients were invited to participate in the study; of these, 78 patients agreed to participate (91%). Table 1 lists the diagnoses and gives the number of patients per diagnosis or operation.
Table 1.
Diagnosis of 78 patients previously operated on for complex congenital heart disease (number of patients is given in parentheses)
| Main diagnosis | Main operation |
| 1. Systemic right ventricle (39) | |
| TGA (22) | Senning (12) or Mustard (10) |
| TGA + PS (5) | Senning (3) or Mustard (2) with PS repair |
| TGA + VSD + PS (6) | Senning (5) or Mustard (1) with VSD closure and PS repair |
| L-TGA + VSD + PS (2) | VSD closure with PS repair (2) |
| L-TGA + VSD + ASD (1) | VSD closure and ASD closure (1) |
| L-TGA + VSD (1) | VSD closure (1) |
| L-TGA + PS (1) | Tricuspid valve replacement (1) |
| AV discordance + DORV + PS (1) | Tricuspid valve replacement and conduit (1) |
| 2. Conduit or mechanical prosthesis (23) | |
| PA + VSD (11) | Rastelli (3); correction with other conduit (8) |
| AoS (4); AVSD (1); MI (1) | Mechanical prosthesis (6) |
| TGA + VSD + PS (4) | Rastelli (4) |
| TGA + VSD (1) | Arterial switch operation with conduit (1) |
| TrArt (1) | Correction with conduit (1) |
| 3. Univentricular connection (11) | |
| TA (8); DILV (2); hypoplastic LV (1) | Fontan (11) |
| 4. Palliative operation-shunt (5) | |
| AVSD (1) | Glenn shunt (1) |
| DILV (1) | Blalock-Taussig shunt (1) |
| Univentricular heart (1) | Modified Blalock-Taussig shunt (1) |
| TA (1) | After Glenn shunt: AV shunt axillary (1) |
| TA + TGA (1) | After banding AP: PH (1) |
AoS, aortic stenosis; AP, pulmonary artery; ASD, atrial septal defect; AV, atrioventricular; AVSD, atrioventricular septal defect; DILV, double inlet left ventricle; DORV, double outlet right ventricle; L-TGA, congenitally corrected TGA; LV, left ventricle; MI, mitral insufficiency; PA, pulmonary atresia; PH, pulmonary hypertension; PS, pulmonary stenosis; TA, tricuspid atresia; TGA, simple transposition of the great arteries; TrArt, common truncus arteriosus; VSD, ventricular septal defect.
Measurements
Questionnaires on health related quality of life and subjective health status were completed.
Health related quality of life
The TAAQOL is a Dutch questionnaire developed by TNO and the Leiden University Medical Centre. Psychometric performance (reliability and validity) of the TAAQOL is satisfactory.19 It consists of 45 questions divided into 12 domains. Each domain contains two to four questions (the actual number per domain is given in parentheses): gross motor functioning (4), fine motor functioning (4), pain (4), sleeping (4), cognitive functioning (4), social functioning (4), daily activities (4), sexual activity (2), vitality (4), happiness (4), depressive moods (4), and aggressiveness (3). For each item, the frequency of occurrence of a health status problem is assessed. If such a problem is reported, the emotional reaction to this problem is also determined. Fig 1 shows an example of the format of the question. The reference period is formulated as “the last month”. The two questions of the domain sexual activity were not appropriate for the present study since the occurrence of problems was compared with one month previously (“Were you less sexually active than a month ago?”). Because such questions are only relevant when an intervention has taken place, this domain was not considered. Scores of each subscale are normalised to a scale ranging from 0 to 100, with higher scores indicating better quality of life.19
Subjective health status
The SF-36 was used to measure subjective health status.22 This questionnaire is based on 35 items divided into eight domains (the number of questions per domain is indicated in parentheses): physical functioning (10), role functioning physical (4), bodily pain (2), general health perceptions (5), vitality (4), social functioning (2), role functioning emotional (3), and mental health (5). Scores range from 0 to 100, with higher scores indicating better subjective health status.
TAAQOL and SF-36 data of the Dutch general population are available.19,22
Physical status
Medical data were collected from the medical records. If clinical information was older than one year, patients were re-examined at the Leiden University Medical Centre (by MK and JO or HV). Physical status was scored by means of three indices determined from these data. Firstly, to measure objectively the severity of the congenital heart disease, the presence of cyanosis, arrhythmia, cardiac failure, and residual defects was combined into an “objective physical index”. Because each variable counted for one point, a score of 0 to 4 was possible, with a higher score indicating a more serious cardiac condition. Secondly, the index of Somerville25 and, thirdly, the New York Heart Association (NYHA) functional class26 were determined (table 2). In both, a higher score indicates more complaints or limitations.
Table 2.
New York Heart Association (NYHA) functional class for patients with cardiac disease and ability index of Somerville
| Somerville index | |
| 1 | Normal life: full time work or school, pregnancy manageable. |
| 2 | Able to work (part time): interference with life (socio/community imposition). |
| 3 | Unable to work: limitations on all activities, pregnancy risk. |
| 4 | Extreme limitation: dependent, almost housebound. |
| NYHA classes | |
| I | No limitations of physical activities. Ordinary activity does not cause undue anginal pain, dyspnoea, fatigue, or palpitations. |
| II | Slight limitations of physical activities. Comfortable at rest, but ordinary activity results in anginal pain, dyspnoea, fatigue, or palpitations. |
| III | Marked limitations of physical activities. Comfortable at rest, less than ordinary activity causes anginal pain, dyspnoea, fatigue, or palpitations. |
| IV | Unable to carry on any physical activities without discomfort. Symptoms of cardiac insufficiency or anginal syndrome may be present even at rest. If any physical activity is undertaken discomfort is increased. |
Statistical analyses
Sample size was based on results of the pilot study19 in which a mean difference of 11 units (on the 0 to 100 scale) was found between patients and the general population on the SF-36 vitality scale. Similar effect sizes are reported in the American SF-36 manual for similar conditions. The sample size (n = 80) was chosen to have 80% power for such a difference. With this sample size there is at least an 80% power to detect a correlation coefficient of 0.30 or more.
The participants' health related quality of life (as measured by the TAAQOL) and their subjective health status (as measured by the SF-36) were compared with those of a random sample of the general Dutch population using analysis of variance with adjustment for age and sex. The sample of the general Dutch population comprised 831 persons for the TAAQOL and 361 for the SF-36.19 After comparison, the data were summarised as mean values and 95% confidence intervals.
Within the group of patients, the overall association between health related quality of life and subjective health status on the one hand and the objective physical index, the Somerville index, and the NYHA class on the other was quantified using canonical correlation analysis to reduce the number of statistical tests. With this method, the maximum association between two sets of variables is quantified.27 When the canonical correlation was significant, pairwise Spearman rank correlations were used to quantify the association between the various indices.
Since the distribution of a number of these variables was skewed, all statistical analyses were performed on rank transformed data. A probability value of p ≤ 0.01 was considered significant because many statistical tests were done. SPSS for Windows version 10.07 (SPSS Inc, Chicago, Illinois, USA) was used to perform statistical calculations.
RESULTS
Patient characteristics
There was an overall response rate of 91%. Medical data were available for all 78 participants and questionnaires for 76 of them. There were 44 men and 34 women, with an average age of 24.3 (range 18–32) years. At the time of the study, 46 participants had a job for more than 12 h/week (59%; two patients were receiving a partial disability benefit), 15 were receiving a full or partial disability benefit (19%), 11 were still at school (14%), three were housewives (4%), and three (4%) were on sick leave or unemployed. Participants lived with a partner n = 34 (43%) or with their parents n = 31 (40%), had their own house n = 7 (9%), or lived in a student (or other) house n = 6 (8%).
For n = 47 60% of the participants the main surgery had been performed before the patient was three years old. Fifty participants (64%) had undergone a previous palliative procedure (such as Rashkind septostomy or banding of the pulmonary artery). The mean age at first operation or intervention was 2.2 (range 0–24) years; 45 patients (58%) had had an intervention soon after birth.
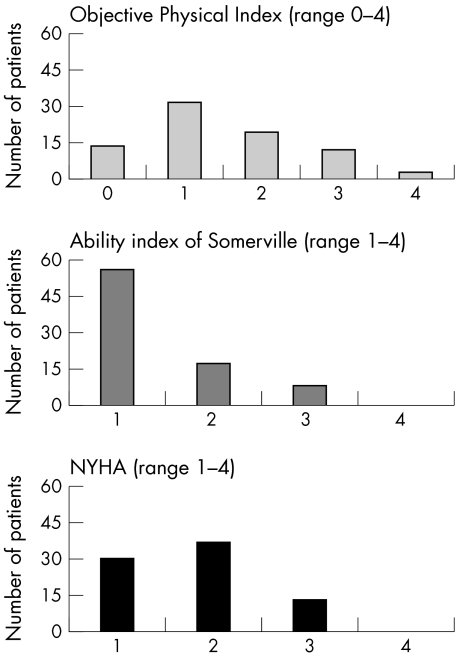
Fig 2 shows the physical status of the patients. Mean score for the objective physical index was 1.48, for the Somerville index 1.41, and for the NYHA class 1.8. Most patients scored 1 in the objective physical index n =31 (40%), indicating that they had at least one of the physical complications. According to the Somerville index, n = 9 (11%) of the participants were unable to work and were limited in all activities (score 3). For the NYHA class, n = 36 (46%) of the participants were in class II and were thus experiencing slight limitations in physical activities.
Figure 2.
Outcome of physical status in the three indices (n = 78).
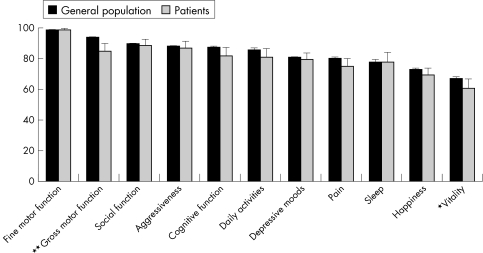
Health related quality of life: patients compared with the general population
Fig 3 gives the average TAAQOL scores of the patients and of the general population sample. The patients had lower health related quality of life in almost all dimensions and scored significantly lower on gross motor functioning (p < 0.001) and vitality (p < 0.01).
Figure 3.
Health related quality of life (TAAQOL) in 76 patients with previously operated complex congenital heart disease is compared with that of the general population (n = 831). Horizontal axis: TNO-AZL adult quality of life (TAAQOL) domains. Vertical axis: score (range 0–100). *p < 0.01; **p < 0.001.
Health related quality of life related to physical status: within the patient group
Several health related quality of life dimensions correlated significantly with the objective physical index, the Somerville index, and the NYHA class (table 3). Canonical correlation analysis showed that the first canonical correlation was significant (r = 0.768); in particular the NYHA class was the most important correlate of gross motor functioning. The pairwise Spearman correlations (table 3) showed the following pattern: health related quality of life correlated weakly with the objective physical index but significantly with gross motor functioning and cognitive functioning. The strongest relations were between the TAAQOL dimensions and the NYHA class.
Table 3.
Spearman's r correlation for medical indices correlated with the TNO-AZL adult quality of life questionnaire (TAAQOL) and the 36 item short form health survey (SF-36) for 76 patients previously operated on for complex congenital heart disease
| Questionnaire | Objective physical index | Somerville index | NYHA class |
| TAAQOL | |||
| Gross motor functioning | −0.33* | −0.53** | −0.77** |
| Daily activities | −0.23 | −0.46** | −0.45** |
| Vitality | −0.12 | −0.42** | −0.47** |
| Sleep | −0.25 | −0.38** | −0.43** |
| Social functioning | −0.10 | −0.30* | −0.35* |
| Pain | −0.03 | −0.24 | −0.36** |
| Cognitive functioning | −0.30* | −0.33* | −0.32* |
| Depressive moods | −0.17 | −0.24 | −0.31* |
| Fine motor functioning | −0.18 | −0.22 | −0.29* |
| Happiness | −0.19 | −0.06 | −0.22 |
| Aggressiveness | −0.03 | −0.15 | −0.19 |
| SF-36 | |||
| Physical functioning | −0.42** | −0.64** | −0.87** |
| Mental health | −0.36** | −0.16 | −0.2 |
| Social functioning | −0.24 | −0.54** | −0.45** |
| Role functioning physical | −0.28 | −0.48** | −0.42** |
| General health | −0.25 | −0.41** | −0.47** |
| Vitality | −0.25 | −0.31* | −0.45** |
| Bodily pain | −0.22 | −0.32* | −0.45** |
| Role functioning emotion | −0.24 | −0.20 | −0.22 |
*p<0.01; **p<0.001
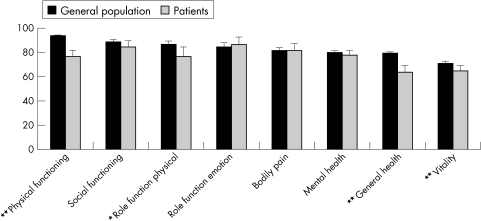
Subjective health status: patients compared with the general population
The SF-36 dimensions physical functioning, role functioning physical (p < 0.01), vitality, and general health perception were significantly lower (p < 0.001) in patients than in the general population (fig 4).
Figure 4.
Subjective health status (SF-36) in 76 patients with previously operated complex congenital heart disease is compared with that of the general population (n = 361). Horizontal axis: 36 item short form health survey (SF-36) domains. Vertical axis: score (range 0–100). *p < 0.01; **p < 0.001.
Subjective health status related to physical status: within the patient group
Almost all SF-36 dimensions correlated significantly with the three physical indices (table 3). Canonical correlation analysis showed that the NYHA class was the strongest correlate of the SF-36 dimensions and of physical functioning in particular (r = 0.864). The patterns for pairwise Spearman correlations were the same as those for health related quality of life, with the strongest relations between subjective health status dimensions and the NYHA class (table 3).
DISCUSSION
This study evaluated health related quality of life and subjective health status in adults with previously operated complex congenital heart disease and determined the relation between these parameters and physical status.
Patients compared with the general population
Comparison between the patients and the general population showed significantly lower scores in the patient group in the physical dimensions only: gross motor functioning and vitality (in the TAAQOL) and physical functioning, role functioning physical, general health perceptions, and vitality (in the SF-36). Thus, both physical function and appraisal of physical dysfunction were significantly lower in the patient group.
There was no significant difference in any of the scores for the non-physical dimensions (social functioning, role functioning emotional, daily activities, depressive moods, etc) between patients and the general population. Some studies on social, psychological, and behavioural outcome in children and adolescents with heart disease have reported problems in these fields,5,28–32 whereas others show normal social behaviour and successful educational and occupational achievements in this group of patients,8,9,33–36 thus supporting the promising outcome of the present study. These latter studies indicate that, over time, patients may adapt to their disease and that denial may even help to normalise functioning.
To improve the patients' long term quality of life, physical aspects must be taken into account.
Firstly, appropriate exercise should be encouraged to avoid patients imposing unnecessary restrictions on themselves,37 sometimes caused when patients receive insufficient information from the specialist.38 In addition, parents should be informed that overprotection can have a negative impact on the physical activities of the child.39 Counselling should, therefore, be based on a thorough clinical assessment together with the use of specific recommendations.39–41 Another way to improve physical capacity is to offer exercise training. For example, in adult male patients with chronic heart failure, specific cardiac training has been shown to improve physical capacity and quality of life,42,43 as in healthy subjects.44 In addition, training in children with various congenital heart diseases has been shown to improve physical abilities.45–47 However, in patients with previously operated complex congenital heart disease the value of exercise training should be further studied, focusing on long term effects in adulthood.48
Prevention of postoperative complications may also avoid poor outcome of the physical dimension of health related quality of life, but this topic is beyond the scope of the present study.
Relation to physical status
Relating physical indices to the dimensions of health related quality of life and subjective health status showed weak correlations. The objective physical index correlated less with health related quality of life and subjective health status than the index of Somerville and the NYHA class. This means that variables such as cyanosis, cardiac failure, or arrhythmia (the best indicators for the objective severity of the disease) do not correlate with the patient's health related quality of life or subjective health status. This is a surprising finding, but other reports on these correlations show the same pattern: factors other than the complexity of the disease (for example, parental attitudes and perceptions, mother's concern, and social support) play a more important part in psychosocial outcome.9,33,49,50 Correlations between all the quality of life dimensions and the Somerville index were significantly weaker than those between the quality of life dimensions and the NYHA class. Thus, although the Somerville index was specifically devised to take into account the adjustment and perception of patients with congenital heart disease,51 its usefulness for this purpose was not confirmed in the present study. The NYHA class correlated significantly and relevantly with the dimensions gross motor functioning (TAAQOL) and physical functioning (SF-36) (Spearman's r = 0.77 and r = 0.87, respectively). When focusing solely on these dimensions, the NYHA class can indeed provide a good estimate of health related quality of life and subjective health status. However, when evaluating the patients' overall health related quality of life and subjective health status, parameters other than those routinely used in a physically oriented cardiological setting should be included.
Remarks and study limitations
When measuring long term outcome of patients with previously operated congenital heart disease, mortality has to be considered. In the unbiased group of 251 selected patients, 123 (49%) had died and could therefore not participate in the study; at least nine of these latter patients were over 18 years old when they died. In addition, two of the participants died from cardiac causes during the study period. Mortality in the age group 18–32 years is, therefore, at least 8.1% (that is, 11 of 135 patients died). Although the study found good health related quality of life in many aspects, the considerable risk of dying after the age of 18 years has to be taken into account. In addition, studying only surviving patients implies a positive selection bias.
The overall response rate in this study was 91%. There was no significant difference between the participants and non-participants in terms of sex or residence. Similarly, there was no significant difference in response between the subdiagnosis groups. However, there was a significant difference between age groups. The response rate in the 24–32 year age group was lower than in the 18–24 year age group (77% and 95%, respectively; p = 0.02). Communication with some of the non-participants indicated that older patients may have more family or work responsibilities and thus less time to participate in a study; how this may have influenced our results remains, however, unclear.
Conclusions
Patients with previously operated complex congenital heart disease experienced limitations only in the physical dimensions of health related quality of life and subjective health status. Objective medical variables correlated only weakly with health related quality of life and can therefore not be used to assess health related quality of life. Wagner and colleagues52 reported that “the routine use of health status measures may enhance patients' care”. The dedicated health related quality of life instrument used in the present study (TAAQOL) is well validated19 and valuable in patient care since it measures the patients' own health related feelings and problems in daily life. It provides more relevant information than just measuring functioning with subjective health status.12,16,17 These results indicate that, when evaluating health related quality of life, dedicated questionnaires such as the TAAQOL should be used.
Acknowledgments
We thank Jeanet Bruil PhD for expert advice in drafting and revising the questionnaires, Stef van Buuren PhD for statistical assistance after data collection, and Minne Fekkes MA for help with the data from the general population.
Abbreviations
NYHA, New York Heart Association
SF-36, 36 item short form health survey
TAAQOL, Netherlands Organisation for Applied Scientific Research-Academic Medical Centre (TNO-AZL) adult quality of life TACQOL, TNO-AZL child quality of life
REFERENCES
- 1.Schor EL, Lerner DJ, Malspeis S. Physicians' assessment of functional health status and well-being. The patient's perspective. Arch Intern Med 1995;155:309–14. [PubMed] [Google Scholar]
- 2.Gersony WM, Hayes CJ, Driscoll DJ, et al. Second natural history study of congenital heart defects: quality of life of patients with aortic stenosis, pulmonary stenosis, or ventricular septal defect. Circulation 1993;87:I52–65. [PubMed] [Google Scholar]
- 3.Ghisla R, Stocker F, Weber JW, et al. [Psychosocial effects of heart disease in adolescents and adults with tetralogy of Fallot]. Schweiz Med Wochenschr 1983;113:20–4. [PubMed] [Google Scholar]
- 4.Kaemmerer H, Tintner H, Konig U, et al. [Psychosocial problems of adolescents and adults with congenital heart defects]. Z Kardiol 1994;83:194–200. [PubMed] [Google Scholar]
- 5.Mir TS, Brockhoff C, Eiselt M, et al. Messung der gesundheitsbezogenen Lebensqualität (LQ) von Erwachsenen mit angeborenen Herzerkrankungen mit dem SF-36 Health Survey. J Kardiol 2000;7:506–10. [Google Scholar]
- 6.Mair DD, Puga FJ, Danielson GK. Late functional status of survivors of the Fontan procedure performed during the 1970s. Circulation 1992;86:II106–9. [PubMed] [Google Scholar]
- 7.Meijboom F, Szatmari A, Deckers JW, et al. Cardiac status and health-related quality of life in the long term after surgical repair of tetralogy of Fallot in infancy and childhood. J Thorac Cardiovasc Surg 1995;110:883–91. [DOI] [PubMed] [Google Scholar]
- 8.Saliba Z, Butera G, Bonnet D, et al. Quality of life and perceived health status in surviving adults with univentricular heart. Heart 2001;86:69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ternestedt BM, Wall K, Oddsson H, et al. Quality of life 20 and 30 years after surgery in patients operated on for tetralogy of Fallot and for atrial septal defect. Pediatr Cardiol 2001;22:128–32. [DOI] [PubMed] [Google Scholar]
- 10.Tong EM, Sparacino PS, Messias DK, et al. Growing up with congenital heart disease: the dilemmas of adolescents and young adults. Cardiol Young 1998;8:303–9. [DOI] [PubMed] [Google Scholar]
- 11.Guyatt GH, Naylor CD, Juniper E, et al. Users' guides to the medical literature. XII. How to use articles about health-related quality of life. Evidence-based medicine working group. JAMA 1997;277:1232–7. [DOI] [PubMed] [Google Scholar]
- 12.Leventhal H, Colman S. Quality of life: a process view. Psychol Health 1997;12:753–67. [Google Scholar]
- 13.Schipper H, Clinch JJ, Olweny CLM. Quality of life studies: definitions and conceptual issues. In: Spilker B, ed. Quality of life and pharmacoeconomics in clinical trials. Philadelphia: Lippincott-Raven Publishers, 1996:11–23.
- 14.Vogels T, Verrips GH, Verloove-Vanhorick SP, et al. Measuring health-related quality of life in children: the development of the TACQOL parent form. Qual Life Res 1998;7:457–65. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Constitution of the World Health Organization. Geneva: World Health Organization, 1948.
- 16.Bradley C. Importance of differentiating health status from quality of life. Lancet 2001;357:7–8. [DOI] [PubMed] [Google Scholar]
- 17.Smith KW, Avis NE, Assmann SF. Distinguishing between quality of life and health status in quality of life research: a meta-analysis. Qual Life Res 1999;8:447–59. [DOI] [PubMed] [Google Scholar]
- 18.Verrips GH, Vogels T, Verloove-Vanhorick SP, et al. Health-related quality of life measure for children: the TACQOL. J Appl Ther 1997;1:357–60. [Google Scholar]
- 19.Fekkes M, Kamphuis RP, Ottenkamp J, et al. Health-related quality of life in young adults with minor congenital heart disease. Psychol Health 2001;16:239–51. [Google Scholar]
- 20.Rovers MM, Krabbe PF, Straatman H, et al. Randomised controlled trial of the effect of ventilation tubes (grommets) on quality of life at age 1–2 years. Arch Dis Child 2001;84:45–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stolk EA, Busschbach JJ, Vogels T. Performance of the EuroQol in children with imperforate anus. Qual Life Res 2000;9:29–38. [DOI] [PubMed] [Google Scholar]
- 22.Aaronson NK, Muller M, Cohen PDA, et al. Translation, validation, and norming of the Dutch language version of the SF-36 health survey in community and chronic disease populations. J Clin Epidemiol 1998;51:1055–68. [DOI] [PubMed] [Google Scholar]
- 23.Gandek B, Ware JE. Methods for validating and norming translations of health status questionnaires: the IQOLA project approach. International quality of life assessment. J Clin Epidemiol 1998;51:953–9. [DOI] [PubMed] [Google Scholar]
- 24.Tynan MJ, Becker AE, Macartney FJ, et al. Nomenclature and classification of congenital heart disease. Br Heart J 1979;41:544–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Warnes CA, Somerville J. Tricuspid atresia in adolescents and adults: current state and late complications. Br Heart J 1986;56:535–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Criteria Committee of the New York Heart Association, Inc. Nomenclature and criteria for diagnoses of diseases of the heart and blood vessels, 5th edn. New York: New York Heart Association, 1953:81.
- 27.Hotelling H. Relations between two sets of variates. Biometrika 1936;28:321–77. [Google Scholar]
- 28.Alden B, Gilljam T, Gillberg C. Long-term psychological outcome of children after surgery for transposition of the great arteries. Acta Paediatr 1998;87:405–10. [DOI] [PubMed] [Google Scholar]
- 29.Bjørnstad PG, Spurkland I, Lindberg H. The impact of severe congenital heart disease on physical and psychosocial functioning in adolescents. Cardiol Young 1995;5:56–62. [Google Scholar]
- 30.Casey FA, Sykes DH, Craig BG, et al. Behavioral adjustment of children with surgically palliated complex congenital heart disease. J Pediatr Psychol 1996;21:335–52. [DOI] [PubMed] [Google Scholar]
- 31.Mahle WT, Clancy RR, Moss EM, et al. Neurodevelopmental outcome and lifestyle assessment in school-aged and adolescent children with hypoplastic left heart syndrome. Pediatrics 2000;105:1082–9. [DOI] [PubMed] [Google Scholar]
- 32.Utens EM, Verhulst FC, Duivenvoorden HJ, et al. Prediction of behavioural and emotional problems in children and adolescents with operated congenital heart disease. Eur Heart J 1998;19:801–7. [DOI] [PubMed] [Google Scholar]
- 33.Brandhagen DJ, Feldt RH, Williams DE. Long-term psychologic implications of congenital heart disease: a 25-year follow-up. Mayo Clin Proc 1991;66:474–9. [DOI] [PubMed] [Google Scholar]
- 34.Van Doorn C, Yates R, Tunstill A, et al. Quality of life in children following mitral valve replacement. Heart 2000;84:643–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horner T, Liberthson R, Jellinek MS. Psychosocial profile of adults with complex congenital heart disease. Mayo Clin Proc 2000;75:31–6. [DOI] [PubMed] [Google Scholar]
- 36.Zeltzer L, Kellerman J, Ellenberg L, et al. Psychologic effects of illness in adolescence. II. Impact of illness in adolescents: crucial issues and coping styles. J Pediatr 1980;97:132–8. [DOI] [PubMed] [Google Scholar]
- 37.Fritsch J, Winter UJ, Kaemmerer H, et al. [Cardiopulmonary capacity of patients with congenital heart defects in childhood, adolescence and adulthood]. Z Kardiol 1994;83(suppl 3):131–9. [PubMed] [Google Scholar]
- 38.Swan L, Hillis WS. Exercise prescription in adults with congenital heart disease: a long way to go. Heart 2000;83:685–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kitchiner D. Physical activities in patients with congenital heart disease [editorial]. Heart 1996;76:6–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gutgesell HP, Gessner IH, Vetter VL, et al. Recreational and occupational recommendations for young patients with heart disease: a statement for physicians by the Committee on Congenital Cardiac Defects of the Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 1986;74:1195A–8A. [PubMed] [Google Scholar]
- 41.Liberthson RR. Arrhythmias in the athlete with congenital heart disease: guidelines for participation. Annu Rev Med 1999;50:441–52. [DOI] [PubMed] [Google Scholar]
- 42.Wielenga RP, Erdman RA, Huisveld IA, et al. Effect of exercise training on quality of life in patients with chronic heart failure. J Psychosom Res 1998;45:459–64. [DOI] [PubMed] [Google Scholar]
- 43.Willenheimer R, Erhardt L, Cline C, et al. Exercise training in heart failure improves quality of life and exercise capacity. Eur Heart J 1998;19:774–81. [DOI] [PubMed] [Google Scholar]
- 44.Fletcher GF, Balady G, Blair SN, et al. Statement on exercise: benefits and recommendations for physical activity programs for all Americans: a statement for health professionals by the Committee on Exercise and Cardiac Rehabilitation of the Council on Clinical Cardiology, American Heart Association. Circulation 1996;94:857–62. [DOI] [PubMed] [Google Scholar]
- 45.Fredriksen PM, Kahrs N, Blaasvaer S, et al. Effect of physical training in children and adolescents with congenital heart disease. Cardiol Young 2000;10:107–14. [DOI] [PubMed] [Google Scholar]
- 46.Longmuir PE, Tremblay MS, Goode RC. Postoperative exercise training develops normal levels of physical activity in a group of children following cardiac surgery. Pediatr Cardiol 1990;11:126–30. [DOI] [PubMed] [Google Scholar]
- 47.Tomassoni TL. Role of exercise in the management of cardiovascular disease in children and youth. Med Sci Sports Exerc 1996;28:406–13. [DOI] [PubMed] [Google Scholar]
- 48.Driscoll DJ. Exercise rehabilitation programs for children with congenital heart disease: a note of caution. Pediatr Exerc Sci 1990;2:191–6. [DOI] [PubMed] [Google Scholar]
- 49.Hommeyer JS, Holmbeck GN, Wills KE, et al. Condition severity and psychosocial functioning in pre-adolescents with spina bifida: disentangling proximal functional status and distal adjustment outcomes. J Pediatr Psychol 1999;24:499–509. [DOI] [PubMed] [Google Scholar]
- 50.Stein RE, Jessop DJ. Relationship between health status and psychological adjustment among children with chronic conditions. Pediatrics 1984;73:169–74. [PubMed] [Google Scholar]
- 51.Somerville J. `Grown-up' survivors of congenital heart disease: who knows? Who cares? Br J Hosp Med 1990;43:132–6. [PubMed] [Google Scholar]
- 52.Wagner AK, Ehrenberg BL, Tran TA, et al. Patient-based health status measurement in clinical practice: a study of its impact on epilepsy patients' care. Qual Life Res 1997;6:329–41. [DOI] [PubMed] [Google Scholar]