Marfan syndrome is a connective tissue disorder with manifestations in multiple organ systems.1 Dilatation of the main pulmonary artery is one of the established criteria for the diagnosis of Marfan syndrome. Normal values have been assessed for the pulmonary artery bifurcation but not for the pulmonary artery root.2 Since the pulmonary artery root consists basically of the same tissue as the ascending aorta, dilatation of the pulmonary artery might predominantly occur in the root similar to the dilatation process occurring in the ascending aorta in Marfan patients.3 The prevalence and prognosis of pulmonary artery dilatation in Marfan syndrome is still unknown. The aim of the present study was to assess main pulmonary artery dimensions both at the level of the pulmonary artery bifurcation and at the pulmonary artery root in normal subjects and in Marfan patients with and without aortic root replacement.
METHODS
Fifty consecutive Marfan patients (mean age 33 (10) years, 34 men, 16 women) underwent routine cardiac magnetic resonance (MR) imaging. Thirty five of these patients had previously undergone aortic root replacement. The control group consisted of 15 age and sex matched healthy subjects (mean age 28 (4) years, nine men, six women).
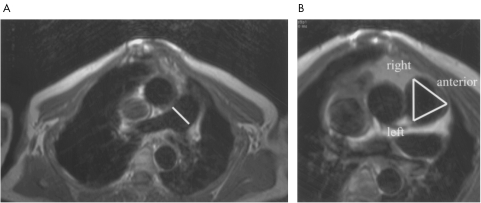
Main pulmonary artery dimensions were assessed with MR imaging on axial spin echo images at two levels: (1) the level of the pulmonary artery bifurcation, and (2) the level of the pulmonary artery root (fig 1). The anterior right diameter of the pulmonary root showed the smallest variability and was used for analysis.
Figure 1.
Levels of measurement on axial spin echo planes in a patient with Marfan syndrome. (A) Main pulmonary artery diameter measurement at the level of pulmonary artery bifurcation. (B) Pulmonary artery root measurements: anterior-right diameter, anterior-left diameter and right-left diameter. Note the pectus carinatum.
RESULTS
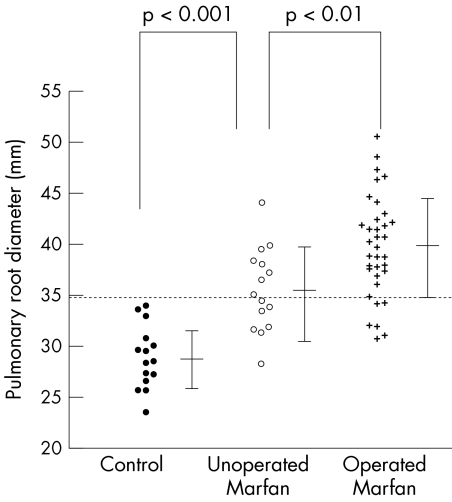
At the pulmonary artery bifurcation the mean (SD) diameter was 24.0 (2.0) mm (range 21.0–27.5 mm) in normal subjects and 30.7 (3.6) mm (range 21.4–38.5 mm) in Marfan patients. The mean diameter of the pulmonary artery root in normal subjects and Marfan patients was 28.8 (3.0) mm (range 23.5–33.9 mm) and 38.4 (5.1) mm (range 28.3–50.7 mm), respectively. The upper limits of normal at the level of the pulmonary artery bifurcation and at the pulmonary artery root in our study were 28.0 mm and 34.8 mm, respectively. Using these cut-off values, 38 (76%) of all Marfan patients had an enlarged pulmonary artery at the level of the bifurcation and 37 (74%) had an enlarged pulmonary artery root (fig 2).
Figure 2.
Pulmonary artery root diameter in Marfan patients with and without aortic root replacement and the control group. Dotted line is the cut-off value. In 74% of the Marfan patients the pulmonary artery root diameter was above the cut-off value.
In normal subjects as well as in Marfan patients with and without aortic root replacement, dimensions measured at the pulmonary artery root were significantly larger than dimensions measured at the pulmonary artery bifurcation (p < 0.001). The mean difference between pulmonary artery root diameter and diameter at the pulmonary artery bifurcation was larger in Marfan patients with (8.0 (4.4) mm) and without (7.0 (3.8) mm) aortic root replacement than in normal subjects (4.8 (3.2) mm). Marfan patients with aortic root replacement had significantly larger main pulmonary artery diameters at both levels than Marfan patients without aortic root replacement. In Marfan patients without aortic root replacement, diameters were significantly larger at both the pulmonary root and at the pulmonary bifurcation level compared to control subjects (p < 0.001) (fig 2). There was a good correlation between pulmonary artery root diameter and aortic root diameter in non-operated patients (r = 0.76).
DISCUSSION
Our study provides the first clinical data on normal values for main pulmonary artery root diameter and on main pulmonary artery dimensions in Marfan patients. Normal values of pulmonary artery bifurcation diameter were comparable with previously published data.2
Marfan patients with elective aortic root replacement had significantly larger pulmonary artery dimensions than non-operated Marfan patients. A logical explanation would be that patients with an aortic root replacement represent a subgroup of patients in whom the cardiovascular system is more affected and therefore also have increased main pulmonary artery dimensions. This is supported by the good correlation we found between pulmonary and aortic root diameter in non-operated Marfan patients.
The difference between pulmonary artery root diameter and the diameter measured at the pulmonary artery bifurcation was larger in Marfan patients than in normal subjects. This indicates that in Marfan patients dilatation is most prominent in the pulmonary artery root, similar to the dilatation process in the aortic root in Marfan patients. This is consistent with the study of Niwa and colleagues who found the same medial abnormalities in the main pulmonary artery in patients with pulmonary trunk aneurysm, as in the ascending aorta of Marfan patients.4 Thus, measurement of the pulmonary artery root, and not only at the level of the bifurcation, seems advisable in all Marfan patients.
Main pulmonary artery dilatation and aneurysms are rare and associated with congenital heart disease, most frequently patent ductus arteriosus, followed by ventricular and atrial septal defects. Until now 48 cases of pulmonary artery dissection have been reported, of which only two cases have been in patients with Marfan syndrome.5 The largest pulmonary root diameter found in our study was 50.4 mm, but further pulmonary artery dilatation and dissection could become of clinical relevance in the near future, as survival has greatly increased during the past decades because of improved medical treatment and surgical techniques for aortic complications.
In this study we showed that the main pulmonary artery, particularly the pulmonary artery root, was dilated in the majority of Marfan patients. There was a good correlation between pulmonary and aortic root diameter in non-operated Marfan patients. Marfan patients with aortic root replacement had larger main pulmonary artery dimensions than non-operated patients. These findings suggest that dilatation of the pulmonary root increases with progressive involvement of the cardiovascular system in Marfan patients. Although, until now, main pulmonary artery aneurysm and dissection are rare, they may become of more clinical relevance in the near future because of increased longevity in Marfan patients.
REFERENCES
- 1.Pyeritz RE, McKusick VA. The Marfan syndrome: diagnosis and management. N Engl J Med 1979;300:772–7. [DOI] [PubMed] [Google Scholar]
- 2.Paz R, Mohiaddin RH, Longmore DB. Magnetic resonance assessment of the pulmonary arterial trunk anatomy, flow, pulsatility and distensibility. Eur Heart J 1993;14:1524–30. [DOI] [PubMed] [Google Scholar]
- 3.Hokken RB, Bartelings MM, Bogers AJJC, et al. Morphology of the pulmonary and aortic roots with regard to the pulmonary autograft procedure. J Thorac Cardiovasc Surg 1997;113:453–61. [DOI] [PubMed] [Google Scholar]
- 4.Niwa K, Perloff JK, Bhuta SM, et al. Structural abnormalities of great arterial walls in congenital heart disease: light and electron microscopic analyses. Circulation 2001;103:393–400. [DOI] [PubMed] [Google Scholar]
- 5.Senbaklavaci O, Kaneko Y, Bartunek A, et al. Rupture and dissection in pulmonary artery aneurysms: incidence, cause, and treatment – review and case report. J Thorac Cardiovasc Surg 2001;121:1006–8. [DOI] [PubMed] [Google Scholar]