The use of the implantable cardioverter-defibrillator (ICD) for life threatening ventricular arrhythmias is standard therapy, in large part because clinical trials data have consistently demonstrated its superiority over medical treatment in preventing sudden cardiac death.1 This success prompts closer examination and refinement of quality of life (QOL) outcomes in ICD patients. Although no universal definition of QOL exists, most researchers agree that “quality of life” is a generic term for a multi-dimensional health outcome in which biological, psychological, and social functioning are interdependent.2 To date, the clinical trials demonstrating the efficacy of the ICD have focused primarily on mortality differences between the ICD and medical treatment. While the majority of the QOL data from these trials is yet to be published, many small studies are available for review and support the concept that ICD implantation results in desirable QOL for most ICD recipients.3 In some patients, however, these benefits may be attenuated by symptoms of anxiety and depression when a shock is necessary to accomplish cardioversion or defibrillation. This paper reviews the published literature on QOL and psychological functioning of ICD patients and outlines the clinical and research implications of these findings.
QUALITY OF LIFE AND THE ICD: PATIENT REPORTS
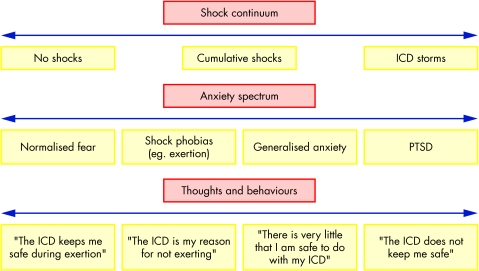
Definitive conclusions about QOL differences between patients managed with an ICD and those treated with antiarrhythmic drugs are difficult to make in the absence of large, randomised, controlled trials. Available evidence indicates that ICD recipients experience a brief decline in QOL from baseline but improve to pre-implant levels after one year of follow up.4 The largest clinical trial data published in final form is from the coronary artery bypass graft (CABG) Patch trial which randomised patients to ICD (n = 262) versus no ICD (n = 228) while undergoing CABG surgery.5 In contrast to May and colleagues,4 data from this trial indicate that the QOL outcomes (mental and physical) for the ICD patients were significantly worse compared to patients with no ICD. Subanalyses revealed that there was no difference in QOL for non-shocked ICD patients versus no ICD patients. These results indicated that the ICD group who had received shocks was responsible for the significantly worse mental and physical QOL outcome scores between the groups. Collectively, these data suggest that the experience of shock may contribute to psychological distress and diminished QOL. Figure 1 details the psychological continuum a patient may experience secondary to shock.
Figure 1.
Continuum of implantable cardioverter-defibrillator (ICD) shock response. PTSD, post-traumatic stress disorder.
Other investigators have examined patients with ICDs and compared them to patients with permanent pacemakers. Very few consistent differences can be demonstrated between these two populations. For example, Duru and colleagues6 found no differences in QOL score, anxiety or depression when comparing ICD patients with and without shock experience and pacemaker patients. ICD patients with a shock history were more likely to report limitations in leisure activities and anxiety about the ICD, but they also viewed the ICD as a “life extender”. Herbst and colleagues7 recently compared the QOL and psychological distress of four patient groups: ICD only (n = 24) v ICD plus antiarrhythmic drug (n = 25) v antiarrhythmic drug only (n = 35) v a general cardiac sample (n = 73). QOL was assessed using the short form 36 (SF-36) and three supplementary scales examining sleep, marital and family functioning, and sexual problems. Comparisons were made between ICD groups and drug groups. Results indicated that there were no significant differences on the 11 QOL scales, even after controlling for age, sex, disease severity, and duration of treatment. However, significant differences were found in drug groups versus no drug groups, such that the drug treated group consistently reported greater impairment in physical functioning, vitality, emotional, and sleep functioning, as well as psychological distress. Collectively, these results suggest that QOL is maintained in ICD treated groups, while antiarrhythmic drug treatment is associated with diminished QOL and increased psychological distress.
In contrast, others have compared ICD patients to either antiarrhythmic drug treated patients or a cardiac reference group and have not found significant differences between these treated groups. For example, Arteaga and Windle8 compared three groups: ICD (n = 45), medication (n = 30), and reference group (n = 29) on QOL and psychological distress. No significant differences were observed on measures of QOL and psychological distress between the treated groups, although psychological distress was associated with lower QOL for all groups. Younger patients and patients with greater cardiac dysfunction reported reduced QOL. Similarly, Carroll and colleagues9 compared cardiac arrest survivors who received either an ICD or medications and found no significant differences in QOL. Herrmann and associates10 also compared QOL between a group of ICD and general coronary artery disease (CAD) patients and found no significant differences on measures of QOL. Moreover, ICD patients reported significantly lower levels of anxiety than the CAD reference group.
A US national survey of ICD patients and spouses (NSIRSO) parts 1 and 211 examined global QOL and psychosocial issues in 450 patients. Approximately 91% of ICD recipients reported desirable QOL, either better (45%) or the same (46%) following implantation. However, a small group of ICD recipients (approximately 15%) reported significant difficulty in emotional adjustment. Younger patients (50 years of age and under) reported better general health, but worse QOL and emotional functioning than each of the other age groups studied. ICD shock history did not have a significant effect on any of the global outcome ratings. The spouses and partners of these recipients (n = 380) provided convergent validity of the recipients' reports; no significant differences were found between raters on the 10 most common concerns. Of note, frequent ICD shocks, younger age, and being female were associated with increased adjustment difficulty. The results of these two surveys suggest that ICD recipients derive significant health related QOL benefits from ICD therapy, although some (approximately 10–20%) experience difficulty. This percentage is consistent with the expected rates of distress in comparable medical populations.
RETURN TO WORK AS A QOL PROXY
An objective index of QOL is the ability to return to work. ICD recipients have favourable return to work rates in currently available studies. The largest such study (n = 101) indicated that 62% of patients had resumed employment.12 Those who returned to work were more educated and less likely to have a history of myocardial infarction. No significant differences were found between those who returned to work and those who did not on measures of age, sex, race, functional class, ejection fraction, extent of CAD, reason for ICD, or concomitant surgery. Similar results were obtained from a sample of young ICD patients in which 10 of the 18 were gainfully employed; eight of those had returned to the same job that they held before implantation.13 These results suggest that the majority of ICD patients who wish to return to work are capable of doing so.
INCIDENCE AND IMPACT OF PSYCHOLOGICAL ISSUES
The typical ICD recipient must overcome both the stress of experiencing a life threatening arrhythmia and the challenge of adjusting to the ICD. Anxiety is particularly common, with approximately 24–87% of ICD recipients experiencing increased symptoms of anxiety after implantation and diagnostic rates for clinically significant anxiety disorders ranging from 13–38%.3 The occurrence of ICD shocks is generally faulted for this psychological distress, but its causal influence is confounded by the presence of a life threatening medical condition. Depressive symptoms reported in 24–33% of ICD patients are consistent with other cardiac populations.3
ICD related fears are universal and may be the most pervasive psychosocial adjustment challenge ICD patients face. Psychological theory suggests that symptoms of fear and anxiety can result from a classical conditioning paradigm in which certain stimuli or behaviours are coincidentally paired with an ICD shock and are thereby avoided in the future. Because of fear of present and/or future discharges, some patients increasingly limit their range of activities and inadvertently diminish the benefits of the ICD in terms of QOL. Pauli and colleagues14 examined the anxiety scores of ICD patients and found that anxiety was not related to ICD discharges but was highly related to a set of “catastrophic cognitions”. Patients with high anxiety scores tended to interpret bodily symptoms as signs of danger and believed that they had heightened risk of sudden death. In addition, catastrophic cognitions were associated with anxiety scores consistent with the scores of panic disorder patients and different from the scores of the healthy volunteer sample. These results suggest that psychosocial interventions that utilise cognitive–behavioural protocols will likely prevent and/or reduce anxiety problems regardless of shock exposure by changing catastrophic thinking and over-interpretation of bodily signs and symptoms. Figure 2 illustrates a hypothesised interrelationship between shocks, psychological distress, and QOL based on the available research.
Figure 2.
Hypothesised interrelationship between shocks, psychological distress, and quality of life (QOL).
Uncertainty related to illness has been demonstrated to be important and related to QOL and psychological functioning in ICD patients.9 The uncertainty of life with a potentially life threatening arrhythmia and an ICD may lead patients to resort to a “sickness scoreboard” mentality, by which they view the frequency of ICD shocks as indicative of how healthy they are and as predictive of their future health.3 In general, outcomes based on the frequency of shocks alone are not a valid indicator of health. ICD shocks can be triggered by both ventricular arrhythmias, for which the device was implanted, and supraventricular arrhythmias, which it was not meant to treat. Shocks for either arrhythmia feel the same to the patient but do not necessarily indicate a decline in health.
EFFECT OF SHOCK ON QOL
Credner and her colleagues defined an “ICD storm” as ≥ 3 shocks in a 24 hour period. She found that approximately 10% of their sample of 136 ICD patients experienced an ICD storm during the first two years following ICD implantation.15 Moreover, the mean (SD) number of shocks for this group of storm patients was 17 (17) (range 3–50; median 8). The experience of an ICD storm may prompt catastrophic cognitions and feelings of helplessness. These adverse psychological reactions have been linked in initial research as prospective predictors for the occurrence of subsequent arrhythmias and shocks at one, three, six, and nine month intervals, leading the researchers to conclude that “negative emotions were the cause, rather than a consequence, of arrhythmia events”.16 Although additional research focusing on a wide range of potentially identifiable “triggers” of arrhythmias is needed, this initial research indicates that reducing negative emotions and psychological distress may also decrease the chances of receiving a shock.
The literature defines specific risk factors for poor QOL and psychosocial outcomes for ICD patients that include, but extend beyond, simple shock experience. ICD patients who are younger—defined in the literature as < 50 years of age—have increased psychological distress.17 ICD patients who do not understand their device and their condition often experience difficulties making lifestyle adjustments. Similarly, ICD patients that have the additional stressors such as loss of job or loss of role functioning often experience psychosocial difficulties that warrant additional professional attention and referral. Table 1 details additional suspected risk factors from the general cardiac literature that can serve as markers for psychosocial attention.
Table 1.
Additional suspected risk factors that can serve as markers for psychosocial attention in patients with ICDs
| ICD specific |
| ▸ Young ICD recipient (age <50 years) |
| ▸ High rate of device discharges |
| ▸ Poor knowledge of cardiac condition or ICD |
| General cardiac |
| ▸ Significant history of psychological problems |
| ▸ Poor social support |
| ▸ Increased medical severity or comorbidity |
CLINICAL AND RESEARCH IMPLICATIONS RELATED TO QOL
Psychosocial and QOL interventions for ICD patients
Table 2 details each of the studies available that used psychosocial intervention for ICD patients. General methodological problems are consistent across studies. Firstly, the studies report on very limited sample sizes and incur a resulting low statistical power. Secondly, most of the studies were conducted using a support group format, which typically involves a participant led, unstructured approach rather than a professional led, structured approach. Although the participant led approach has some merit, such as a high level of involvement for some members, this approach often does not involve sufficient factual and objective information to produce measurable change. Instead, this approach tends to focus predominantly on the emotional aspects of the illness. In contrast, professional led groups tend to focus more on strategy and skill building rather than simply the expression of emotion. Taken together, the methodologic flaws of most of these interventions limit their utility in gauging the potential of professional led, structured cognitive–behavioural psychosocial intervention.
Table 2.
Psychosocial intervention studies with ICD recipients
| Study | n | Duration of treatment | Summary of results and critique of findings | |
| Badger and Morris (1989) | 12 | 8 non-structured support group sessions | Purpose: support group intervention v no treatment control group. Results: no significant between group differences. Trends were reported towards improvement in the treatment group | Very small number of patients were studied. No systematic treatment protocol was delivered. This was a patient led methodology |
| Molchany and Peterson (1994) | 11 | Not specified | Purpose: support group intervention v no treatment control group. Results: no significant between group differences. Qualitative analyses demonstrated improved ability to cope and increased satisfaction with life in group participants | Very small number of patients were studied. No known systematic treatment protocol was delivered. Duration of treatment is unknown but may not have been sufficient to detect differences |
| Sneed et al (1997) | 34 | 2 inpatient individual sessions, 2 support group sessions, and 12 telephone contacts over a 16 week period. | Purpose: support group intervention v no treatment control group. Results: no significant between group differences at 4 month follow up. Results indicated that tension/anxiety reduced for both groups | Small number of patients were studied. Systematic treatment protocol was delivered but group format was patient led. Longer duration of treatment was a significant improvement in methodology but the content of the follow up phone contacts was not well specified |
| Kohn et al (2000) | 49 | 9 sessions (pre-implant, pre-discharge, 7 routine follow up visits) | Purpose: compared individual cognitive–behavioural treatment to usual care. Results: individual treatment group reported less depression, less anxiety, less general distress, (p<0.05), despite receiving a higher level of shocks (p<0.07) | Sufficient sample size. Most comprehensive and well documented treatment protocol study available. Effects were robust enough to detect differences. Used an expensive and time intensive, individual therapy protocol |
Support groups are a popular adjunctive treatment for ICD patients because they provide an efficient conduit for patient education spanning the biopsychosocial domains.2 The active ingredients of support groups probably centre on the universality of many patient concerns and the sharing of information and strategies to deal effectively with these concerns. We suggest that support groups are a valuable but not necessarily sufficient means of providing psychosocial care for all ICD patients. Some patients will need more individualised, tailored cognitive–behavioural or pharmacological interventions to address more completely their psychosocial needs. As noted above, professional led groups are preferable because a systematic presentation of information via selected expert speakers and a broad based curriculum could be designed for maximal benefit for the majority of participants. Certainly patient stories or testimonials can also play a regular role, but that is a process that can occur both formally and informally during the meetings among group members. The majority of the groups are maintained by ICD health professionals with a strong commitment to psychosocial care. There is no formula on how to structure support groups for maximal effectiveness, but they remain important in the care of ICD patients as one of a set of strategies to improve the psychosocial care of ICD patients.
The most significant study of psychosocial interventions for ICD patients involved a randomised controlled methodology to reduce psychological distress.18 Individual cognitive–behavioural therapy was used to reduce psychological distress in newly implanted ICD patients to determine if such treatment would also reduce arrhythmic events requiring shocks for termination. These investigators randomised 49 ICD patients to active treatment versus no treatment. The treatment consisted of an individual therapy session at pre-implant, pre-discharge from the hospital, consecutive weeks for four weeks, and then sessions at routine cardiac clinic appointments at one, three, and five months post-implantation. They found that active treatment patients reported less depression, less anxiety, and less general psychological distress than the no treatment group at nine month follow up evaluations. These results suggest that more systematic interventions for new ICD patients would likely produce optimal psychological and QOL outcomes. Although this study did not include information about the cost effectiveness of the intervention, it is reasonable to assume that psychological intervention delivered in this manner would likely be at least cost-neutral if it prevented more expensive hospitalisations, additional medications, and unnecessary accessing of care. Future research on psychosocial interventions should provide further information about the costs of their interventions for closer cost effectiveness analysis.
Clinician readiness for psychosocial interventions
The realistic probability of practising cardiologists and nurses having the time or skills necessary to provide such extensive psychosocial interventions is small. We surveyed physicians and nurses (n = 261) to rate their views of specific ICD patient outcomes, common daily life problems for ICD patients, and their own comfort in managing these concerns.19 The majority of ICD patients experience desirable QOL, emotional wellbeing, and family functioning post-implantation, as viewed by health care providers. However, healthcare providers reported that approximately 10–20% of ICD patients were significantly worse in these areas post-implantation. The most common problems for ICD recipients in daily life included driving restrictions/limitations, coping with ICD shocks, and depression. Health care providers generally reported the most comfort handling traditional medical issues (that is, 92% of the sample reported comfort in managing patient adherence concerns), and the least comfort in managing emotional wellbeing issues (for example, only 39% of the sample reported comfort in managing depression and anxiety symptoms). These results are somewhat disconcerting when we consider that our previous work also showed that ICD patients were equally likely to seek discussion about emotional issues with health care providers (37%) as they were with family and friends (36%).11 Our survey of health care providers also found that the majority believed that their ICD patients wanted more information to help them cope with or adjust to their ICD (91%) and that they believed that education as an intervention would be effective (83%).
Discomfort while addressing psychosocial issues for cardiology practitioners is not surprising and most likely reflects lack of training and experience in behavioural medicine and psychology. We have suggested the “Four A's checklist” to detect and manage psychosocial issues in ICD clinics: ask, advise, assist, and arrange referral.17, 20 The first step is to ask the patient about their ICD related concerns in an effort to define accurately their perceived problem. In table 3, we have provided sample diagnostic questions that can assist the clinician and yield sufficient diagnostic precision.21 Secondly, the healthcare provider can advise the ICD patient on the common challenges that lie ahead and how to manage these concerns via supportive communication. The healthcare provider should take care to respect the coping style and adjustment difficulties of each patient. Thirdly, the provider can assist the patient by addressing the immediate concerns of the patient, normalising the most common challenges, educating the patient about their device, and provide brief problem solving. Finally, the health care provider should arrange a consultation for those recipients who would benefit from speaking with a mental health specialist. ICD recipients should be told that anxiety and depression are common and expected side effects for many medical patients including ICD patients, and for that reason, attending to the psychosocial aspects of adjustment is part of the overall treatment strategy. This rationale of a “stress management” based approach is broadly acceptable to most patients.
Table 3.
Pocket guide to key interview questions for the psychosocial care of ICD patients
| Key concept | Sample interview question | Interpretation |
| Affective functioning depression | Depressed mood question: during the past month, have you often been bothered by feeling down, hopeless, or depressed? | If either of these questions screen positive, the presence of depression should be pursued via additional interview or referral to |
| Anhedonia question: during the past month, have you felt less interested in or gotten less pleasure from doing the things you typically enjoy? | a mental health professional. If both of these questions are negative, the patient is unlikely to have major depression | |
| Anxiety | Generalised anxiety: are you generally a nervous person? | A positive response to general anxiety indicates a condition that is unlikely to be responsive to clinic based intervention by a cardiologist and should be referred. Specific |
| Specific anxiety: do you have regular and continuous fears of ICD shocks? | anxiety, however, is likely to be improved by a clinic based discussion from a cardiologist. However, referral may still be necessary if education and reassurance related to the specific cardiac concerns are not sufficient | |
| Behavioural functioning avoidance behaviour | Avoidant behaviour: do you avoid doing anything simply because of your fear of shocks? | Confirmed avoidance behaviour increases the probability of a significant anxiety problem and warrants referral for additional work up by a mental health professional |
| Cognitive functioning attention and memory | Attention and memory change and perceived impact: have you noticed any significant changes in your attention or memory since ICD implantation? Have these changes presented any problems in your daily functioning? | Cognitive changes are a recognised part of significant cardiac illness Neuropsychological evaluation is indicated if the changes have presented any problems or concerns for the patient or family members |
CONCLUSIONS
The ICD is the treatment of choice for life threatening arrhythmias. The QOL data from these trials, which focused primarily on mortality, now warrants equal scrutiny. All available data suggest that the ICD will achieve comparable if not better QOL than alternative treatments. Future research must place greater emphasis on ICD specific and arrhythmia specific measures that may be more sensitive to more changes in outcome. Measurement and interventions should focus on patient acceptance of the device. Interdisciplinary studies that include cardiology, psychology, nursing, and cardiac rehabilitation specialists are needed to guide best clinical practice. The reputation of the ICD as a “shock box” is a significant source of anxiety to potential patients. Today, third generation ICDs are much improved in their sensing and tiered therapy options to reduce shocks and their resulting distress. Despite improvements in therapy such as antitachycardia pacing, ICD patients are likely always to need some attention to psychological adjustment. We suggest that routine consideration of psychosocial needs be integrated into the clinical care of ICD patients worldwide.
QOL and psychological functioning of ICD patients: key points.
-
▸ Incidence of psychological diagnosis
- anxiety 13–38%
- depression 34–43%
-
▸ Risk factors for maladjustment
- young age
- frequent shocks
- women
-
▸ Four A's
- ask
- advise
- assist
- arrange
-
▸ Multidisciplinary care team
- cardiologist
- nurse
- mental health professional
- rehabilitation
REFERENCES
- 1.Glikson M, Friedman PA. The implantable cardioverter defibrillator. Lancet 2001;357:1107–17. ▸ This article provides a thorough review of the details of device functioning and clinical trial data for health care professionals. [DOI] [PubMed] [Google Scholar]
- 2.Engel GE. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129–36. [DOI] [PubMed] [Google Scholar]
- 3.Sears SF, Todaro JF, Saia TL, et al. Examining the psychosocial impact of implantable cardioverter defibrillators: a literature review. Clin Cardiol 1999;22:481–9. ▸ All psychosocial literature is reviewed and interpreted including specific psychological and behavioural theory posited about the development and manifestation of distress in ICD patients. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.May CD, Smith PR, Murdock CJ, et al. The impact of the implantable cardioverter defibrillator on quality of life. Pacing Clin Electrophysiol 1995;18:1411–8. [DOI] [PubMed] [Google Scholar]
- 5.Namerow PB, Firth BR, Heywood GM, et al. Quality of life six months after CABG surgery in patients randomized to ICD versus no ICD therapy: findings from the CABG Patch trial. Pacing Clin Electrophysiol 1999;22:1305–13. ▸ This randomised controlled trial data implicated the specific role of ICD shock in the quality of life outcomes of ICD patients. [DOI] [PubMed] [Google Scholar]
- 6.Duru F, Buchi S, Klaghofer R, et al. How different from pacemaker patients are recipients of implantable cardioverter-defibrillators with respect to psychosocial adaptation, affective disorders, and quality of life? Heart 2001;85:375–9. ▸ These authors were the first to use generic quality of life indices to compare implantable device patients on measures of quality of life and adaptation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herbst JH, Goodman M, Feldstein S, et al. Health related quality of life assessment of patients with life-threatening ventricular arrhythmias. Pacing Clin Electrophysiol 1999;22:915–26. [DOI] [PubMed] [Google Scholar]
- 8.Arteaga WJ, Windle JR. The quality of life of patients with life threatening arrhythmias. Arch Intern Med 1995;155:2086–91. [PubMed] [Google Scholar]
- 9.Carroll DL, Hamilton GA, McGovern BA. Changes in health status and quality of life and the impact of uncertainty in patients who survive life-threatening arrhythmias. Heart Lung 1999;28:251–60. [DOI] [PubMed] [Google Scholar]
- 10.Herrmann C, von zur Muhen F, Schaumann A, et al.Standardized assessment of psychological well-being and quality-of-life in patients with implanted defibrillators. Pacing Clin Electrophysiol 1997;20:95–103. [DOI] [PubMed] [Google Scholar]
- 11.Sears SF, Eads A, Marhefka S, et al. The U.S. national survey of ICD recipients: examining the global and specific aspects of quality of life [abstract]. Eur Heart J 1999;20:232.10082156 [Google Scholar]
- 12.Kalbfleisch KR, Lehmann MH, Steinman RT, et al. Reemployment following implantation of the automatic cardioverter defibrillator. Am J Cardiol 1989;64:199–202. [DOI] [PubMed] [Google Scholar]
- 13.Dubin AM, Batsford WP, Lewis RJ, et al. Quality of life in patients receiving implantable cardioverter defibrillators at or before age 40. Pacing Clin Electrophysiol 1996;19:1555–9. [DOI] [PubMed] [Google Scholar]
- 14.Pauli P, Wiedemann G, Dengler W, et al.Anxiety in patients with an automatic implantable cardioverter defibrillator: what differentiates them from panic patients? Psychosom Med 1999;61:69–76. ▸ This study provided specific examination of the role of cognitive appraisal processes in the development of psychological distress in ICD patients by comparing their responses to both anxiety populations and healthy same aged populations. [DOI] [PubMed] [Google Scholar]
- 15.Credner SC, Klingenheben T, Mauss O, et al.Electrical storm in patients with transvenous implantable cardioverter defibrillators. J Am Coll Cardiol 1998;32:1909–15. ▸ These authors defined a criteria for ICD storm and provided data regarding its incidence in a clinical sample of ICD patients. [DOI] [PubMed] [Google Scholar]
- 16.Dunbar SB, Kimble LP, Jenkins LS, et al.Association of mood disturbance and arrhythmia events in patients after cardioverter defibrillator implantation. Depress Anxiety 1999;9:163–8. ▸ This study provided prospective examination of psychological factors and the incidence of shock that allowed for prediction of shock by psychological distress. [DOI] [PubMed] [Google Scholar]
- 17.Sears SF Jr, Burns JL, Handberg E, et al. Young at heart: understanding the unique psychosocial adjustment of young implantable cardioverter defibrillator recipients. Pacing Clin Electrophysiol 2001;24:1113–7. [DOI] [PubMed] [Google Scholar]
- 18.Kohn CS, Petrucci RJ, Baessler C, et al. The effect of psychological intervention on patients' long-term adjustment to the ICD: a prospective study. Pacing Clin Electrophysiol 2000;23:450–6. ▸ This study was the first randomised controlled trial of a comprehensive psychosocial intervention programme for ICD patients. [DOI] [PubMed] [Google Scholar]
- 19.Sears SF, Todaro JF, Urizar G, et al. Assessing the psychosocial impact of the ICD: a national survey of implantable cardioverter defibrillator health care providers. Pacing Clin Electrophysiol 2000;23:939–45. ▸ This study provided US physician and nurse data and indicated the specific psychosocial concerns that ICD patients report to health care providers and their degree of comfort managing these concerns. [DOI] [PubMed] [Google Scholar]
- 20.Sotile WM, Sears SF. You can make a difference: brief psychosocial interventions for ICD patients and their families. Minneapolis, Minnesota: Medtronic Inc, 1999. ▸ This book provides a comprehensive review and set of clinical strategies of the common psychosocial challenges for ICD patients and families for nurses and physicians.
- 21.Whooley MA, Simon GE. Managing depression in medical outpatients. N Engl J Med 2000;343:1942–50. [DOI] [PubMed] [Google Scholar]