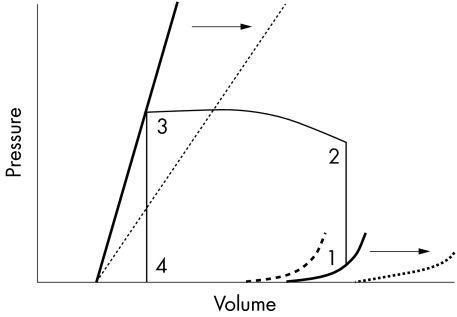
Figure 1.
Left ventricular pressure-volume relationships.5 The bold straight line shows the normal end systolic pressure–volume relationship (ESPVR), defining ventricular contraction. ESPVR is independent of changes in preload and afterload. The slope is maximal at end systole and has the units of elastance, E=ΔP/ΔV. It has therefore been designated Emax. The bold curved line shows normal end diastolic pressure–volume relationship (EDPVR). The straight section of the line represents addition of the initial volume. While ventricular volume increases from zero to approximately 50 ml, transmural pressure remains at zero. Left ventricular end diastolic pressure (LVEDP) then increases in a curvilinear manner during addition of further volume. The pressure–volume loop (1–4) represents one cardiac cycle (1–2, isovolumetric contraction; 2–3, stroke volume; 3–4, isovolumetric relaxation). The interrupted straight line represents Emax in sepsis, with depressed contractility indicated by a downward and right shift of the ESPVR. In survivors of septic shock this is accompanied by a right shift of the EDPVR (interrupted curved line) caused by ventricular dilatation, enabling an increase in stroke volume. In non-survivors diastolic stiffness develops represented by an upward and left shift of the EDPVR (bold interrupted curved line), leading to impaired diastolic filling and a reduction in stroke volume. Arrows represent possible contribution of nitric oxide (NO) to the pressure–volume relationships in sepsis. While NO may be responsible for the reduction in systolic contractility, the septic patient is able to maintain end systolic volume because of a reduction in systemic vascular resistance; therefore the overriding haemodynamic effect of NO in sepsis may be facilitation of ventricular dilatation, which acts to further stroke volume and maintain cardiac output. Potentially, NO blockade in sepsis may convert the EDPVR of a surviving septic patient to a non-survivor.