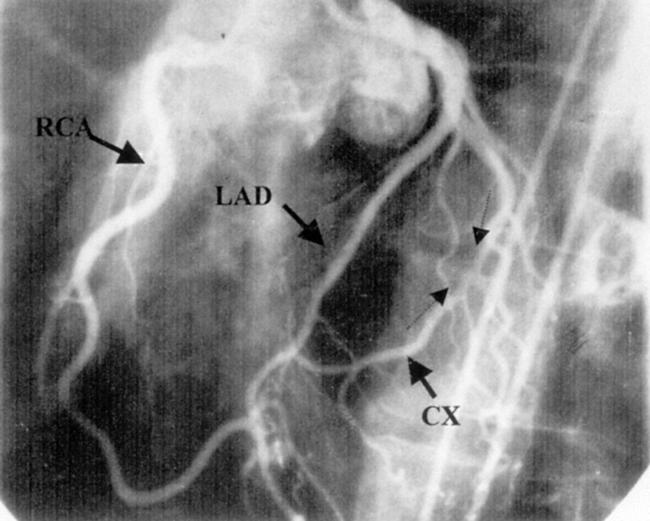
A 49 year old man presented with atypical chest pain for five months. He had no risk factors for atherosclerosis. Exercise electrocardiography was stopped prematurely because of leg cramp. Coronary angiography was performed and revealed normal left ventricular function. Left and right coronary angiography did not show any evidence of luminal narrowing or occlusion of either coronary artery (below left). However, with the selective injection of the right coronary artery (RCA) in a left anterior oblique view, the RCA and distal and mid portion of left circumflex artery (CX) were simultaneously visualised. An intercoronary connection was also seen near the crux (below centre). The RCA and CX were then catheterised at the same time. There was no pressure damping during selective placement of the catheter tip in either coronary ostium. In the left anterior oblique view with cranial angulation, simultaneous injection of contrast material into both coronary ostia revealed interarterial continuity between the RCA and CX (below right: arrowheads show both antegrade and retrograde filling of CX lumen).
Intercoronary artery continuity or “coronary cascade” is a rare variant of the coronary circulation. Two types have been described: communication between the CX and the RCA in the posterior atrioventricular groove (as in this patient), and communication between left anterior descending and posterior descending artery in the distal interventricular groove. Compared with collaterals, intercoronary arterial connections are larger in diameter (≥ 1 mm), extramural, and straight. Furthermore, the structure of an intercoronary arterial connection is typical of an epicardial coronary artery, with a well defined muscular layer. Intercoronary arterial connections are thought to be congenital in origin. It is suggested that faulty embryological development allows the existing intercoronary channel to remain prominent and maintain a large calibre.
In our case selective injection of the left coronary artery did not demonstrate retrograde filling of the distal RCA. One may propose that both the force of injection and the velocity of flow in the left coronary artery would account for this discrepancy.
True prevalence of this entity is unknown but we identified only one patient among the 7086 angiograms performed at our laboratory during the last 10 years. The functional significance of this large anastomotic connection between normal coronary arteries is unclear but one may speculate that they have a potential role in protecting the myocardium should significant atherosclerosis develop in either of the parent arteries.
Figure 1.
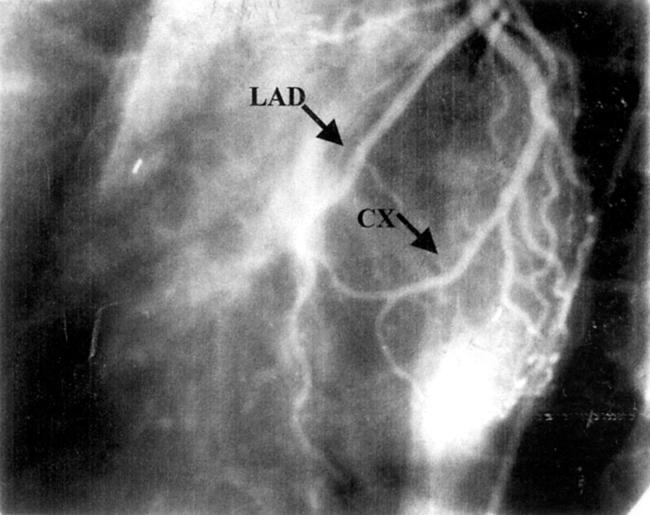
Figure 2.
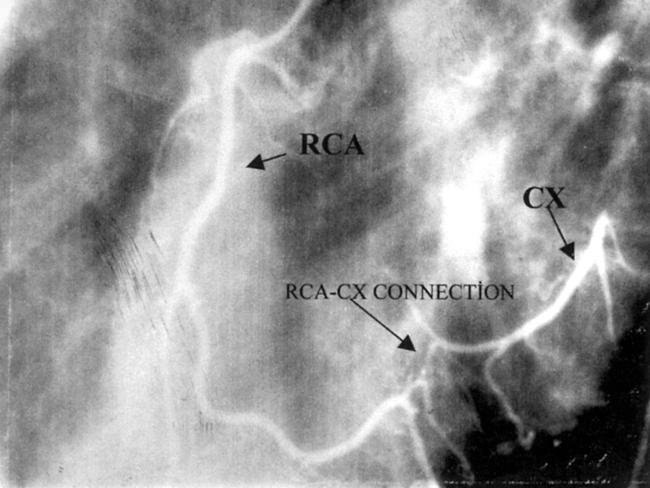
Figure 3.