Abstract
Objective: To determine the clinical and prognostic differences between patients with heart failure who had preserved or deteriorated systolic function, defined as a left ventricular ejection fraction of > 50% or < 50%, respectively, within two weeks of admission to hospital.
Methods: The records of 229 patients with congestive heart failure were studied. There were 95 women and 134 men, mean (SD) age 66.7 (11.7) years, who had been admitted to a cardiology department for congestive heart failure in the period 1991 to 1994, and whose left ventricular systolic function had been evaluated echocardiographically within two weeks of admission. Data were collected on the main clinical findings, supplementary investigations, treatment, and duration of hospital admission. Follow up information was obtained in the spring of 1998 by searching the general archives of the hospital and by a telephone survey.
Results: Left ventricular systolic function was preserved in 29% of the patients. The preserved and deteriorated groups differed significantly in the sex ratio (more women in the preserved group) and in the presence of a third heart sound, cardiomegaly, alveolar oedema, ischaemic cardiomyopathy, and treatment with angiotensin converting enzyme (ACE) inhibitors (all more in the deteriorated group). There were no significant differences in age, New York Heart Association functional class, rhythm disturbances, left ventricular hypertrophy, treatment with drugs other than ACE inhibitors, or survival. In the group as a whole, the survival rates after three months, one year, and five years were 92.6%, 80%, and 48.4%, respectively.
Conclusions: In view of the unexpectedly poor prognosis of patients with congestive heart failure and preserved left ventricular systolic function, controlled clinical trials should be carried out to optimise their treatment.
Keywords: congestive heart failure, systolic function
The cardiovascular diseases that have shown the greatest increase in incidence and prevalence in recent years, especially among the elderly, are chronic atrial fibrillation and congestive heart failure.1,2 In Spain, the CARDIOTENS 1999 study showed that congestive heart failure accounted for 25% of all cardiopathies seen in primary care and cardiology services, its origin being traceable in most cases to arterial hypertension and ischaemic heart disease.3
It is now known that in a large proportion of patients with heart failure, overall left ventricular systolic functional variables are within normal limits.4–6 Significant clinical differences have been reported between such patients and those with “classical” congestive heart failure with deteriorated left ventricular systolic function.7–9 In particular, arterial hypertension appears to be more prevalent among patients with preserved systolic function, and ischaemic cardiomyopathy among those with deteriorated function. It has also been reported that preservation of systolic function is associated with improved prognosis in heart failure,4,5 although not all studies are in agreement5—possibly because of differences among the study groups, especially in relation to hospital admission.
Our study examined a sample of hospital inpatients with heart failure, determining the proportions with normal and abnormal left ventricular systolic function and the clinical characteristics of the two groups. We also began a long term study of mortality in heart failure patients.
METHODS
Study groups
This was a prospective observational study. We included all patients referred to the cardiology service of the University Clinical Hospital, Santiago de Compostela, who had been admitted to hospital for congestive heart failure between 1 January 1991 and 31 December 1994, whose left ventricular systolic function had been evaluated echocardiographically within two weeks of admission, and whose records showed that in our opinion they had satisfied the modified Framingham criteria for congestive heart failure. These require the presence of two or more major criteria (paroxysmal nocturnal dyspnoea, orthopnoea, rales, jugular venous distension, third sound, and radiological signs of pulmonary congestion and/or cardiomegaly), or one major criterion plus two or more minor criteria (effort dyspnoea, oedema, hepatomegaly, and pleural effusion).
Of the 301 patients admitted for congestive heart failure, the above inclusion criteria were satisfied by 229 (74%). The other 72 were excluded either because their records included no echocardiographic study or because its quality was too poor for proper evaluation of ventricular function. There were no significant differences between the patients who were included and excluded.
Of the 229 patients included in the study, congestive heart failure had been diagnosed previously in 43 cases, and 203 patients were admitted to hospital for congestive heart failure for the first time. Once included in the study, subjects were assigned to one of two groups on the basis of whether their systolic function was preserved or not, the criterion for preserved function being an echocardiographically determined ejection fraction of at least 50%.
Echocardiography was performed using a Sonos 1000 apparatus (Hewlett-Packard Inc, Andover, Massachusetts, USA) with 3.5 MHz transducers for images, in accordance with the guidelines of the American Society of Echocardiography. Ventricular volumes were obtained from apical four chamber views using the mean area × length method. Left ventricular ejection fraction (%) was calculated as 100 × (LVEDV − LVESV)/LVEDV, where LVEDV is left ventricular end diastolic volume and LVESV is left ventricular end systolic volume.
All measurements were repeated for four to six successive heart beats, and the values accepted for each patient were the averages of these four to six measurements.
Data collected
For all patients included in the study, data were collected on the main clinical findings, supplementary investigations, treatment, and the duration of hospital admission. In the case of patients admitted on more than one occasion during the study period, the only occasion considered was the first on which an echocardiographic evaluation of systolic function had been undertaken. Follow up information on the subjects' current situation and mortality data were obtained by searching the general archives of the hospital and by a telephone survey carried out in April and May 1998.
Aetiology of heart failure
Ischaemic cardiomyopathy was diagnosed if any of the following criteria were satisfied: a recorded diagnosis of ischaemic cardiomyopathy, previous admission for an acute coronary event (acute myocardial infarct or unstable angina), previous surgical or percutaneous myocardial revascularisation, the presence of pathological Q waves on an ECG obtained during the hospital admission, and coronary images showing more than 50% stenosis of at least one coronary artery. Valve disease was diagnosed if previously identified or if it was indicated by echocardiographic or catheterisation studies (however, the study did not include patients who had been admitted to the cardiology service because of congestive heart failure secondary to severe valve disease). Arterial hypertension was diagnosed if previously identified or if the patient had been taking, or needed, antihypertensive drugs to control the blood pressure. Dilated cardiomyopathy was diagnosed if the patient had shown deteriorating systolic function and a dilated left ventricle but no evidence of ischaemic cardiomyopathy, valve disease, or arterial hypertension.
Statistical analysis
Data for categorical or dichotomous variables were expressed as percentages and compared using a χ2 test or Fisher's exact test. Data for continuous variables are expressed as mean (SD) and compared using Student's t test. Survival curves for the two groups and the whole sample were estimated by the Kaplan–Meier method, and those of the two groups were compared using the two sample log rank test. Factors with independent significant association with survival were identified using Cox's proportional hazards model in a backward stepwise regression analysis, with age, sex, New York Heart Association (NYHA) class IV status, third heart sound, cardiomegaly, alveolar oedema, hypertension, hyperlipidaemia, diabetes, smoking, ischaemic cardiomyopathy, and ejection fraction as independent variables, followed by a secondary Cox analysis in which the independent variables were those identified as significant in the first analysis plus the ejection fraction. The resulting regression coefficients were used to estimate relative risks and the corresponding 95% confidence intervals. The validity of the assumption of proportional hazards was supported by the results of calculating log-log survival plots for each variable, with age and sex controlled. The criterion for significance was p < 0.05.
RESULTS
Sample characteristics
The sample comprised 229 patients, mean (SD) age 66.7 (11.7) years: 95 women (41.5%) and 134 men (58.5%). The duration of hospital admission was 18.1 (16.7) days. The main clinical characteristics are listed in table 1.
Table 1.
Clinical characteristics and treatment of 229 consecutive patients with heart failure in whom left ventricular systolic function was evaluated echocardiographically
| Variable | n | % |
| Age (years)* | 66.7 (11.7) | |
| <65 | 86 | 37.6 |
| 65–74 | 90 | 39.3 |
| >75 | 53 | 23.1 |
| Male | 134 | 58.5 |
| Female | 95 | 41.5 |
| Hospital admission (days)* | 18.1 (16.7) | |
| NYHA IV | 140 | 62.8 |
| Third heart sound | 60 | 26.2 |
| Chest radiography | ||
| Cardiomegaly | 193 | 84.3 |
| Redistribution of flow | 187 | 81.7 |
| Interstitial oedema | 120 | 52.4 |
| Alveolar oedema | 49 | 21.4 |
| Electrocardiography | ||
| Sinus rhythm | 126 | 55.0 |
| Atrial fibrillation | 85 | 37.1 |
| LV hypertrophy | 91 | 39.7 |
| Echocardiography | ||
| LVEF <50% | 163 | 71.2 |
| LVEF >50% | 66 | 28.8 |
| Treatment | ||
| Digoxin | 138 | 60.3 |
| Diuretics | 179 | 78.2 |
| ACE inhibitors | 82 | 35.8 |
| Nitrates | 70 | 30.6 |
| Vasodilators | 12 | 5.2 |
| Calcium antagonists | 31 | 13.5 |
| β Blockers | 14 | 6.1 |
| Anticoagulants | 48 | 21.0 |
*Mean (SD).
ACE, angiotensin converting enzyme; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association functional class.
Aetiology
The most common risk factor for congestive heart failure was systemic arterial hypertension, which was present in 119 patients (52%). The most common underlying heart condition was ischaemic cardiomyopathy, which was diagnosed in 104 patients (45.4%), 63 of whom also had systemic arterial hypertension. Table 2 lists the prevalence of these and other possible causes of congestive heart failure.
Table 2.
Cardiovascular risk factors and underlying cardiopathies in the study sample
| n | % | |
| Cardiovascular risk factors | ||
| Arterial hypertension | 119 | 52.2 |
| Hyperlipidaemia | 76 | 33.2 |
| Diabetes mellitus | 50 | 21.8 |
| Smoking | 72 | 31.4 |
| Underlying cardiomyopathy | ||
| Ischaemic heart disease | 104 | 45.4 |
| Heart valve disease | 54 | 23.6 |
| Dilated cardiomyopathy | 22 | 9.6 |
Left ventricular systolic function
Systolic function had deteriorated in 163 patients (71.2%, the “deteriorated group”) and was preserved in the other 66 (28.8%, the “preserved group”). These two groups differed significantly with regard to the female to male sex ratio (greater in the preserved group), the presence of a third heart sound, cardiomegaly, and alveolar oedema (all more prevalent in the deteriorated group), the prevalence of treatment with angiotensin converting enzyme (ACE) inhibitors (greater in the deteriorated group), and aetiology (coronary disease, valve disease, or dilated cardiomyopathy). There were no significant differences between the two groups with regard to age, NYHA functional class, the presence of sinus rhythm or atrial fibrillation, left ventricular hypertrophy, underlying cardiomyopathy, or treatment with drugs other than ACE inhibitors (table 3).
Table 3.
Clinical characteristics, cardiovascular risk factors, underlying cardiomyopathies, and treatment of congestive heart failure patients with preserved and deteriorated left ventricular systolic function
| Ejection fraction | |||||
| <50% (n=163) | >50% (n=66) | ||||
| Variable | n | % | n | % | p Value |
| Age (years)* | 66.4 (12.0) | 67.2 (10.9) | 0.44 | ||
| Male | 110 | 67.5 | 24 | 36.4 | <0.001 |
| Female | 53 | 32.5 | 42 | 63.6 | |
| NYHA IV | 105 | 75.0 | 53 | 63.9 | 0.079 |
| Third heart sound | 56 | 34.3 | 4 | 6.1 | <0.001 |
| Chest radiography | |||||
| Cardiomegaly | 141 | 86.5 | 52 | 78.7 | 0.024 |
| Alveolar oedema | 43 | 26.4 | 6 | 9.1 | 0.005 |
| Electrocardiography | |||||
| Sinus rhythm | 91 | 55.8 | 35 | 53.0 | 0.53 |
| Atrial fibrillation | 55 | 33.7 | 30 | 45.4 | 0.13 |
| LV hypertrophy | 59 | 36.2 | 32 | 48.5 | 0.15 |
| Cardiovascular risk factors | |||||
| Arterial hypertension | 84 | 51.5 | 35 | 53.0 | 0.87 |
| Hyperlipidaemia | 57 | 34.9 | 19 | 28.7 | 0.36 |
| Diabetes mellitus | 39 | 23.9 | 11 | 16.6 | 0.22 |
| Smokers | 56 | 34.3 | 16 | 24.2 | 0.11 |
| Aetiology | <0.001 | ||||
| Ischaemic heart disease | 85 | 52.1 | 19 | 28.8 | |
| Heart valve disease | 25 | 15.3 | 29 | 43.9 | |
| Dilated cardiomyopathy | 22 | 13.5 | 0 | 0 | |
| Treatment | |||||
| Digoxin | 91 | 55.8 | 47 | 71.2 | 0.13 |
| Diuretic | 129 | 79.1 | 50 | 75.8 | 0.70 |
| ACE inhibitor | 74 | 45.4 | 8 | 12.1 | 0.003 |
| Nitrate | 50 | 30.7 | 20 | 30.3 | 0.93 |
| Vasodilator | 12 | 7.4 | 0 | 0 | 0.16 |
| Calcium antagonist | 19 | 11.7 | 12 | 18.2 | 0.38 |
| β Blocker | 9 | 5.5 | 5 | 7.6 | 0.66 |
| Dicoumarin | 32 | 19.6 | 16 | 24.2 | 0.65 |
*Mean (SD).
ACE, angiotensin converting enzyme; LV, left ventricular.
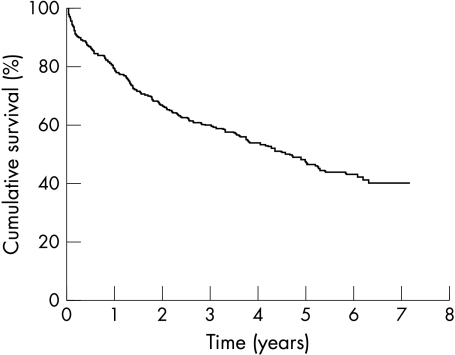
Survival
Among the 212 patients (92.6%) for whom it was possible to obtain reliable survival data, the time elapsed since hospital admission was 4.4 (0.2) years. At the time of the study, 111 had died (52.4%). The death rates after one, three, and five years were 19.1%, 38.1%, and 50.4%, respectively. Figure 1 shows the survival curve of the whole sample. Table 4 lists the results of univariate analyses carried out to determine the effects of several variables on survival. Only age, diabetes, the presence of a third heart sound, NYHA class IV, cardiomegaly, and radiologically detected alveolar oedema were found to have a significant influence.
Figure 1.
Kaplan–Meier survival curve for the whole sample.
Table 4.
Influence of various clinical variables on survival at the time of study (mean 4.4 years after diagnosis)
| Variable | Survival (%) | p Value | RR (95% CI) |
| Age (years) | 0.002 | ||
| <65 | 61.2 | — | |
| 65–75 | 46.8 | 1.82 (1.22 to 2.72) | |
| >75 | 25.0 | 2.48 (1.65 to 3.74) | |
| Female | 49.6 | 0.503 | — |
| Male | 44.9 | 1.03 (0.75 to 1.40) | |
| NYHA IV | 0.007 | ||
| No | 53.5 | — | |
| Yes | 36.8 | 1.96 (1.36 to 2.81) | |
| Third heart sound | 0.017 | ||
| No | 53.5 | — | |
| Yes | 36.8 | 1.61 (1.12 to 2.30) | |
| Chest radiography | |||
| Cardiomegaly | 0.010 | ||
| No | 75.0 | — | |
| Yes | 45.3 | 2.06 (1.01 to 4.21) | |
| Alveolar oedema | 0.003 | ||
| No | 55.0 | — | |
| Yes | 28.3 | 2.06 (1.44 to 2.95) | |
| Electrocardiography | |||
| Sinus rhythm | 0.405 | ||
| No | 44.1 | — | |
| Yes | 50.9 | 0.83 (0.60 to 1.15) | |
| Atrial fibrillation | 0.535 | ||
| No | 50.0 | — | |
| Yes | 45.5 | 1.25 (0.90 to 1.74) | |
| LV hypertrophy | 0.215 | ||
| No | 51.5 | — | |
| Yes | 41.4 | 1.23 (0.88 to 1.73) | |
| Cardiovascular risk factors | |||
| Arterial hypertension | 0.560 | ||
| No | 50.5 | — | |
| Yes | 45.5 | 1.13 (0.82 to 1.56) | |
| Hyperlipidaemia | 0.130 | ||
| No | 55.7 | — | |
| Yes | 43.7 | 1.17 (0.83 to 1.59) | |
| Diabetes mellitus | 0.036 | ||
| No | 50.0 | — | |
| Yes | 38.6 | 1.53 (1.07 to 2.18) | |
| Smoking | 0.951 | ||
| No | 46.5 | — | |
| Yes | 49.2 | 0.87 (0.60 to 1.25) | |
| Aetiology | |||
| Ischaemic heart disease | 0.932 | ||
| No | 47.9 | — | |
| Yes | 47.3 | 1.05 (0.76 to 1.44) | |
| Heart valve disease | 0.563 | ||
| No | 49.1 | — | |
| Yes | 43.1 | 1.25 (0.86 to 1.81) | |
| Dilated cardiomyopathy | 0.108 | ||
| No | 45.5 | — | |
| Yes | 66.7 | 1.37 (0.74 to 2.50) |
CI, confidence interval; LV, left ventricular; NYHA IV, New York Heart Association functional grade IV; RR, relative risk.
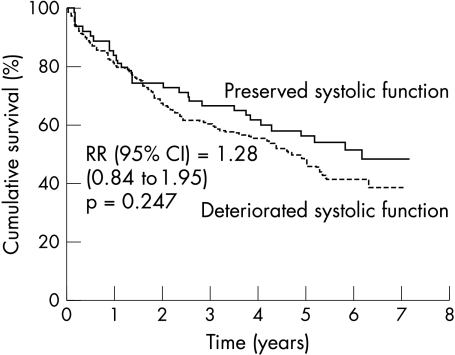
The survival curves for the deteriorated and preserved groups (fig 2) did not differ significantly. The death rates at one, three, and five years after hospital admission were 20.3%, 39.9%, and 54.7% in the deteriorated group, and 17.2%, 33.9%, and 44.2% in the preserved group.
Figure 2.
Kaplan–Meier survival curve of the groups with preserved and deteriorated left ventricular systolic function.
Multivariate analysis showed that only age, sex, alveolar oedema, and NYHA class IV had significant effects on survival (table 5); the left ventricular ejection fraction had no effect even after adjusting for those variables.
Table 5.
Proportional hazards analysis of variables affecting survival
| Variable | β | SE | p Value | RR (95% CI) |
| Age (years) | 0.050 | 0.011 | 0.000 | 1.05 (1.03 to 1.07) |
| Male sex | 0.584 | 0.226 | 0.010 | 1.79 (1.15 to 2.79) |
| NYHA IV | 0.498 | 0.247 | 0.044 | 1.65 (1.01 to 2.67) |
| Alveolar oedema | 0.518 | 0.240 | 0.031 | 1.68 (1.05 to 2.68) |
| Systolic function | 0.102 | 0.243 | 0.673 | 1.11 (0.69 to 1.78) |
β represents regression coefficients; SE is the standard error of β.
Variables considered in the model were age, sex, NYHA class IV, third heart sound, cardiomegaly, alveolar oedema, systolic function (deteriorated or preserved), hypertension, hyperlipidaemia, diabetes, smoking, and ischaemic cardiopathy. Systolic function was forced into the final analysis.
DISCUSSION
Cases of congestive heart failure have traditionally been classified in terms of either systolic or diastolic dysfunction. The truth is, however, that many patients who are admitted to hospital for congestive heart failure are not subjected to evaluation of left ventricular diastolic function, even when it is found that they have normal systolic function. Strictly, such patients should not be given a diagnosis of congestive heart failure caused by diastolic dysfunction, but rather should be classified as having congestive heart failure with preserved systolic function.10,11
Although several groups have studied the epidemiology of congestive heart failure in Spain,3,12,13 none has investigated the proportions of patients with deteriorated and preserved systolic left ventricular function, nor have there been any comparisons of these groups with regard to long term prognosis. In the present study we classified a series of patients admitted to hospital for congestive heart failure as having deteriorated or preserved left ventricular systolic function, as reflected by a left ventricular ejection fraction less than or greater than 50%, and we compared the survival of the two groups over a period of seven years.
The ejection fraction is not a constant characteristic of a given patient, depending as it does on the work required of the heart. However, the fact that it was always measured while the patient was in hospital (within two weeks of admission) may have limited its variability in our study. The echocardiographic method used to measure the ejection fraction, though imperfect, is sufficiently precise for the purpose for which it was employed. An ejection fraction of 50% was chosen as the divide between normal and deteriorated systolic function because it has been the most usual threshold in work in this area.
Fewer than 30% of our patients had preserved left ventricular systolic function. Previous studies have reported figures ranging from 13–74%.4–6,14–16 This variability may be attributable to differences in the definition of congestive heart failure, differences in the time between the onset of symptoms and echocardiographic examination (both advancing disease and the treatment used can lead to changes in systolic function in either direction), and differences in the kinds of unit the patients are admitted to. In the latter respect, most studies have included patients admitted to both cardiology and internal medicine services, although two studies of community based samples4,5 have coincided with certain studies of hospital based series and with the Helsinki aging study17 in reporting figures of about 50%. The lower proportion of patients with preserved left ventricular function in our study may reflect the fact that elderly patients whose congestive heart failure is not thought to be caused by ischaemic cardiomyopathy are not usually referred to our cardiology service.
As in other studies,4,5 we found no significant difference in age between the deteriorated and preserved groups. The fact that our patients were on average younger than those studied by Vasan and colleagues,4 Senni and associates,5 or a recent epidemiological study of cardiovascular disease in Spain3 may be because our sample was taken from patients admitted to hospital.
We found a very significant difference between the sex ratios of the two groups—63.6% of the preserved group were women as against only 32.5% of the deteriorated group. There have been similar findings in other studies.4,5,18 This difference may be related to the preponderance of women among elderly patients with hypertensive hypertrophic cardiomyopathy.19
Although preserved left ventricular systolic function in patients with heart failure has traditionally been related to arterial hypertension, and deteriorated left ventricular systolic function to ischaemic cardiomyopathy, these relations have not been corroborated in all studies. Like us, Senni and associates found no significant difference between the prevalences of arterial hypertension in preserved and deteriorated groups,5 although—as in our study—ischaemic cardiomyopathy was more common in the deteriorated group. With regard to other clinical characteristics, the most salient findings were the greater frequency of a third heart sound and the greater severity of pulmonary congestion in the deteriorated group.
Both in clinical trials and in series of patients seen in routine clinical practice, it has been found that congestive heart failure has a worse prognosis than many neoplasias—a fact that is attributable not only to the characteristics and severity of the disease itself but also to the advanced age of most patients with congestive heart failure. An annual death rate greater than 40% has been reported.20 Published survival curves have varied: the survival rates at three months, one year, and five years after diagnosis were respectively 73%, 57%, and 25% in the Framingham study21; 86%, 76%, and 35% in Sennis study5; and 92.6%, 80%, and 48.4% in our own study. The Rotterdam group recently reported two year and five year survival rates of 79% and 59%.22 These differences are no doubt partly caused by variations among the patient samples studied, but may also reflect the effects of improvements in diagnostic techniques and treatments—though in our study the younger age of our patients and the very small proportion on β blockers in comparison with other studies may well have helped to increase the survival rates.
In spite of its evident clinical importance, there are remarkably few published reports on the prognosis of patients with congestive heart failure and preserved left ventricular systolic function. The reported annual death rates among such patients have ranged from 1.3–17.5%,4–6,14–16 probably because of differences in age and severity of disease. In the Veterans Administration cooperative study of a group of patients with congestive heart failure whose average age was 60 years at diagnosis, and who had a normal left ventricular ejection fraction and no ischaemic cardiomyopathy, the death rate after 5.7 years was only 23%.14 In contrast, Setaro and colleagues reported a seven year death rate of 46% in a group of elderly patients with normal left ventricular systolic function and ischaemic cardiomyopathy as the main cause of the disease.14 In Senni's study,5 the survival of patients with normal left ventricular systolic function was even worse, at 86%, 76%, and 48% after three months, one year, and five years, respectively. The survival curve of our patients with a normal left ventricular ejection fraction was closer to that of Senni's study than the former two studies,14,16 possibly because our study and Senni's are the most recent.
Vasan and colleagues found that patients with preserved left ventricular systolic function had a better prognosis than those with deteriorated systolic function, although their sample was quite small.4 They tentatively attributed their findings to the large proportion of women with arterial hypertension in their study group—in keeping with reports that women with non-ischaemic congestive heart failure have a better prognosis than men,23,24 and that patients with hypertensive congestive heart failure but no evidence of ischaemic cardiomyopathy on coronary angiography have a good prognosis.25 It should be borne in mind, however, that in Vasan's study4 the echocardiographic recordings used to classify the patients as having preserved or deteriorated left ventricular systolic function were not obtained until a median of 2.8 years after the initial appearance of congestive heart failure (range 0.1–15.0 years). Thus the study failed to include those patients who died without ever having had echocardiography. In both our study and Senni's,5 the post-diagnosis survival rates of patients with preserved and deteriorated left ventricular systolic function were initially very similar (three years in Senni's study and 18 months in ours); and although, as in Vasan's study,4 survival was subsequently worse in the deteriorated group, the difference was not significant. However, in our study this difference might have been larger if the proportion of patients taking ACE inhibitors had not been significantly greater in the deteriorated group than in the preserved group—the only significant difference between the two groups with regard to pharmacological treatment.
Conclusions
This is the first Spanish study of the clinical characteristics and long term prognosis of hospital inpatients with congestive heart failure, with and without deteriorated left ventricular systolic function as defined by the left ventricular ejection fraction. Survival in the group with preserved left ventricular systolic function was no better than in the deteriorated group, although this may partly have reflected the more common use of ACE inhibitors in the latter group. As patients with congestive heart failure and a normal left ventricular ejection fraction are currently treated empirically, their poor prognosis suggests the need for controlled clinical trials aimed at identifying the optimal therapeutic strategy for such patients.
REFERENCES
- 1.The SEOSI Investigators. Survey on heart failure in Italian hospital cardiology units. Eur Heart J 1997;18:1457–64. [DOI] [PubMed] [Google Scholar]
- 2.Mosterd A, Hoes AW, de Bruyne MC, et al. Prevalence of heart failure and left ventricular dysfunction in the general population. The Rotterdam Study. Eur Heart J 1999;20:447–55. [PubMed] [Google Scholar]
- 3.González-Juanatey JR, Alegría E, Lozano JV, et al. Impacto de la hipertensión en las cardiopatías en España. Estudio CARDIOTENS 1999. Rev Esp Cardiol 2001;54:139–49. [DOI] [PubMed] [Google Scholar]
- 4.Vasan RS, Larson MG, Benjamin EJ, et al. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction. J Am Coll Cardiol 1999;33:1948–55. [DOI] [PubMed] [Google Scholar]
- 5.Senni M, Tribouilloy CM, Rodeheffer RJ, et al. Congestive heart failure in the community. A study of all incident cases in Olmsted County, Minnesota, in 1991. Circulation 1998;98:2282–9. [DOI] [PubMed] [Google Scholar]
- 6.Vasan RS, Benjamin EJ, Levy D. Prevalence, clinical features and prognosis of diastolic heart failure: an epidemiologic perspective. J Am Coll Cardiol 1995;26:1565–74. [DOI] [PubMed] [Google Scholar]
- 7.Rich MW. Epidemiology, pathophysiology, and etiology of congestive heart failure in older adults. J Am Geriatr Soc 1997;45:968–74. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto K, Wilson DJ, Canzanello VJ, et al. Left ventricular diastolic dysfunction in patients with hypertension and preserved systolic function. Mayo Clin Proc 2000;75:148–55. [DOI] [PubMed] [Google Scholar]
- 9.Levy D, Larson MG, Vasan RS, et al. The progression from hypertension to congestive heart failure. JAMA 1996;275:1557–62. [PubMed] [Google Scholar]
- 10.Rodriguez Artalejo F, Guallar-Castillon P, Banegas JR, et al. Trends in hospitalization and mortality for heart failure in Spain, 1980–1993. Eur Heart J 1997;18:1771–9. [DOI] [PubMed] [Google Scholar]
- 11.Brotons C, Moral I, Ribera A, et al. Tendencias de la morbimortalidad por insuficiencia cardíaca en Cataluña. Rev Esp Cardiol 1998;51:972–6. [DOI] [PubMed] [Google Scholar]
- 12.Cohn JN, Johnson G, and Veterans Administration Cooperative Study Group. Heart failure with normal ejection fraction: the V-HEFT Study. Circulation 1990;81(suppl III):48–53. [PubMed] [Google Scholar]
- 13.Ghali JK, Kadakia S, Bhatt A, et al. Survival of heart failure patients with preserved versus impaired systolic function: the prognostic implications of blood pressure. Am Heart J 1992;123:993–7. [DOI] [PubMed] [Google Scholar]
- 14.Setaro JF, Soufer R, Remetz MS, et al. Long-term outcome in patients with congestive heart failure and intact left ventricular systolic performance. Am J Cardiol 1992;69:1212–16. [DOI] [PubMed] [Google Scholar]
- 15.European Study Group on Diastolic Heart Failure. How to diagnose diastolic heart failure. Eur Heart J 1998;19:990–1003. [DOI] [PubMed] [Google Scholar]
- 16.Senni M, Redfield MM. Heart failure with preserved systolic function. A different natural history. J Am Coll Cardiol 2001;38:1277–82. [DOI] [PubMed] [Google Scholar]
- 17.Kupari M, Lindroos M, Iivanainen AM, et al. Congestive heart failure in old age: prevalence, mechanisms and 4-year prognosis in the Helsinki Ageing Study. J Intern Med 1997;241:387–94. [DOI] [PubMed] [Google Scholar]
- 18.Aronow WS, Ahn C, Kronzon I. Normal left ventricular ejection fraction in older persons with congestive heart failure. Chest 1998;113:867–9. [DOI] [PubMed] [Google Scholar]
- 19.Topol EJ, Traill TA, Fortuin NJ. Hypertensive hypertrophic cardiomyopathy of the elderly. N Engl J Med 1984;312:277–83. [DOI] [PubMed] [Google Scholar]
- 20.McMurray JJ, Stewart S. Heart failure. Epidemiology, aetiology, and prognosis of heart failure. Heart 2000;83:596–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ho KK, Anderson KM, Kannel WB, et al. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation 1993;88:107–15. [DOI] [PubMed] [Google Scholar]
- 22.Mosterd A, Cost B, Hoes AW, et al. The prognosis of heart failure in the general population. The Rotterdam Study. Eur Heart J 2001;22:1318–27. [DOI] [PubMed] [Google Scholar]
- 23.Adams KF, Dunlap SH, Sueta CA, et al. Relation between gender, etiology and survival in patients with symptomatic heart failure. J Am Coll Cardiol 1996;28:1781–8. [DOI] [PubMed] [Google Scholar]
- 24.Ghali JK, Mosley L, Danzell J, et al. Heart failure in women. J LA State Med Soc 1998;150:85–91. [PubMed] [Google Scholar]
- 25.Anguita M, Castillo JC, Ramirez A, et al. Heart failure caused by severe systolic ventricular dysfunction of hypertensive origin. Long-term clinical and functional course. Rev Esp Cardiol 2000;53:927–31. [PubMed] [Google Scholar]