For many years decisions to treat or not treat hypertension with drugs were made considering the level of blood pressure alone. There was vigorous debate over whether patients should be treated at diastolic pressures of 110, 100, 90 mm Hg or some other threshold. However, epidemiological studies show that the risk of cardiovascular complications such as stroke or myocardial infarction is not determined by blood pressure alone, but is strongly influenced by other major risk factors such as age, sex, smoking habit, lipid concentrations, diabetes, target organ damage such as left ventricular hypertrophy (LVH), and established vascular disease such as angina or myocardial infarction.1 Furthermore clinical trials have shown that the absolute risk of cardiovascular disease (CVD) determines the chance of benefit from antihypertensive treatment.2 In 1995 a New Zealand guideline development group turned this knowledge into practice and recommended that treatment of hypertension should be determined by absolute cardiovascular disease risk and not blood pressure thresholds alone.3 Since then most international and national guidelines have embraced the principle of targeting antihypertensive drug treatment at absolute CVD risk, although the details and methods of estimating CVD risk differ greatly between guidelines. In the UK the British Hypertension Society and Joint British Societies (which include cardiology, lipid, hypertension, and diabetes specialist groups) have developed guidelines for the management of uncomplicated mild hypertension according to estimated absolute coronary heart disease (CHD) risk.4,5 This means that hypertension guidelines and guidelines for statins and aspirin in primary prevention cannot be implemented without a working knowledge of the estimation of absolute CHD or CVD risk. This article discusses the principle and practice of using absolute CVD or CHD risk for decisions on antihypertensive treatment.
▸ IMPORTANCE OF ABSOLUTE RISK IN HYPERTENSION
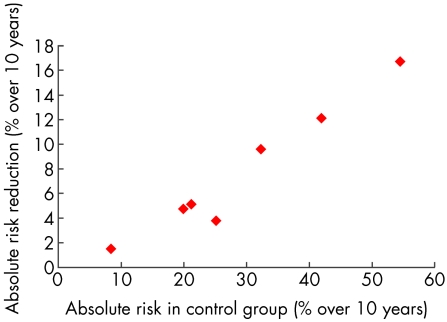
Hypertension is consistently associated with an increased risk of cardiovascular complications, including stroke, myocardial infarction, heart failure, and renal failure. Antihypertensive treatment decreases the risk of all cardiovascular complications by about 25%, largely through reducing stroke by 38% and coronary events by 16%.6 A key point is that the relative risk reduction, 25%, is approximately constant across all groups of patients,2 meaning that it is similar in men and women, young and old, smokers and non-smokers, and so on. When antihypertensive treatment was targeted only at a predetermined blood pressure threshold, the assumption was that the 25% relative risk reduction translated into a worthwhile chance of benefit for all patients. This assumption was incorrect. The relative risk reduction tells us nothing about the chance of an individual benefiting from treatment by avoiding a cardiovascular complication.7 The chance of benefit is determined by the absolute reduction in risk of cardiovascular complications, which is a product of the relative risk reduction and the absolute risk of developing a cardiovascular complication. Figure 1 shows the absolute reductions in cardiovascular events (or absolute benefit) from antihypertensive treatment plotted against the absolute CVD event rate observed in the placebo treated groups in randomised controlled trials of antihypertensive treatment. Because the relative risk reduction for CVD events was similar in all trials at around 25% there is a linear relation between absolute risk and benefit from treatment. Thus the absolute CVD risk and not the level of blood pressure per se determines the probability of benefit when treating hypertension.
Figure 1.
Absolute cardiovascular disease (CVD) risk reductions observed in selected randomised controlled trials of antihypertensive treatments plotted against the absolute CVD risk in the placebo groups. Note the linear relation between absolute risk and absolute risk reduction. Data from Collins and Peto6 and the Syst-Eur trial (see website for reference).
Table 1 shows data for two patients with the same average blood pressure, 150/96 mm Hg, which illustrate the key role of estimation of absolute risk in determining the chance of benefit from treatment. Patient A has very low CVD risk (2.5% over 10 years) because her other risk factors are favourable, and her chance of benefit from treatment is only 0.6% over 10 years. Patient B has a much higher CVD risk (51% over 10 years) because of his age, sex, smoking habit, and lipid profile, and his chance of benefit is nearly 13% over 10 years. The absolute benefit is succinctly described as the “number needed to treat” or “NNT”,8 which is the number of similar patients who have to be treated for a specified time period (usually five years) to prevent a CVD complication in one. Thus the five year NNT for patient A in table 1 is 321, and the five year NNT for patient B is 16. Although the two patients have the same blood pressure, 150/96 mm Hg, patient B has a much higher absolute risk of cardiovascular disease and is far more likely to benefit from treatment. When compared to other treatments in general use, the benefit from treatment for patient B (NNT 16) would be considered very worthwhile whereas the merits of treatment for patient A (NNT 321) might be debated. Informed people may decline treatment with such a small chance of benefit, and it is also possible that “harm” from treatment might outweigh any benefit.
Table 1.
Two patients with identical blood pressures (150/96 mm Hg) but pronounced differences in other major risk factors, illustrating a 20-fold difference in absolute cardiovascular risk and in chance of benefit from treatment between patients with “mild hypertension”
| Patient A | Patient B | |
| Blood pressure (mm Hg) | 150/96 | 150/96 |
| Sex | Female | Male |
| Age (years) | 35 | 65 |
| Total cholesterol (mmol/l) | 5.0 | 7.0 |
| HDL cholesterol (mmol/l) | 1.4 | 1.0 |
| Smoking | No | Yes |
| Diabetes | No | No |
| Left ventricular hypertrophy | No | No |
| Absolute CVD risk (% over 10 years) | 2.5 | 51.0 |
| Relative risk reduction (%) | 25 | 25 |
| Absolute benefit (% over 10 years) | 0.6 | 12.8 |
| NNT (5 years) | 321 | 16 |
POSSIBLE HARM FROM TREATING LOW RISK PATIENTS
Harm from treatment can take several forms. Serious adverse reactions to modern antihypertensive drugs, such as fatal airways obstruction with β blockers or renal failure with angiotensin converting enzyme (ACE) inhibitors, are probably very rare. However, the chance of an adverse reaction is generally unrelated to the CVD risk, and therefore similar in low risk and high risk patients.9 Below some level of CVD risk the chance of harm from treatment will outweigh benefit. Hoes and colleagues suggested that the risk from antihypertensive treatment may exceed benefit when the pretreatment risk of all cause mortality was below 6% over 10 years,10 although their analysis has been criticised. Antihypertensive drugs can also cause subjective side effects (for example, cold extremities with β blockers, flushing with calcium channel blockers, cough with ACE inhibitors) which may be harmful, although the treatment withdrawal rates in unbiased studies are very low, and quality of life is not influenced adversely when compared with placebo treatment. However the “labelling” effect of treating hypertension can itself cause perceived ill health and psychological morbidity. People do not like taking tablets and may develop “side effects” that impair quality of life. These disadvantages of treatment are of little concern when treating high risk patients who have a high probability of benefiting from treatment, but they may outweigh the benefits of treatment in very low risk patients.
Abbreviations.
ABPM: ambulatory blood pressure monitoring
ACE: angiotensin converting enzyme
CHD: coronary heart disease
CVD: cardiovascular disease
HDL: high density lipoprotein
JNC: Joint National Committee
LVH: left ventricular hypertrophy
NNT: number needed to treat
WHO-ISH: World Health Organization-International Society of Hypertension
Patients with high CVD risk who will get worthwhile benefit from treatment need to be identified and offered treatment, whereas very low risk patients may choose observation rather than drug treatment. Estimation of the absolute CHD or CVD risk is essential to separate those who require treatment from those who may not.
HIGH RISK HYPERTENSIVE PATIENTS
Some patient groups have such high CVD risk and chance of benefit that they require antihypertensive treatment even for mild hypertension (≥ 140/90 mm Hg) without formal calculation of absolute risk. Patients with any form of symptomatic atherosclerotic vascular disease, including previous myocardial infarction, bypass graft surgery, angina, stroke or transient ischaemic attack, peripheral vascular disease or atherosclerotic renovascular disease need treatment of even very mild hypertension (≥ 140/90 mm Hg) for secondary prevention. Indeed there is mounting evidence that secondary prevention patients with “normal” blood pressure (< 140/90 mm Hg) benefit from blood pressure reduction. This is similar in principle to reducing normal or even “low” cholesterol with statins. Patients with target organ damage such as LVH, heart failure, proteinuria or renal impairment also have high CVD risk and need treatment of even very mild hypertension. Older patients (> 60 years) have high CHD risk by virtue of their age alone, and benefit from treatment of even mild hypertension (≥ 140/90 mm Hg). Patients with long term average blood pressure ≥ 160/100 mm Hg have high CVD risk because of the steep association between blood pressure and risk of stroke. The risk of developing cardiovascular complications increases dramatically with the long term average diastolic blood pressure ≥ 100 mm Hg.11 Formal risk calculation will underestimate true CVD risk for reasons discussed later, and all patients with blood pressure ≥ 160/100 mm Hg after prolonged observation and despite lifestyle advice should be treated.
Patients with type II diabetes also have high CVD risk, but in addition gain extra benefit from antihypertensive treatment because it prevents microvascular complications (for example, nephropathy, retinopathy) as well as large vessel complications. All patients with type II diabetes and mild hypertension (≥ 140/90 mm Hg) should be treated regardless of their absolute CVD risk. Patients with type I diabetes and mild hypertension (≥ 140/90 mm Hg) generally have diabetic nephropathy and should be treated.
These high risk groups all require drug treatment for hypertension and it follows that formal risk assessment is only necessary for decisions on antihypertensive treatment in patients below age 60 with uncomplicated mild hypertension (long term average blood pressure 140–159/90–99 mm Hg). However, because of the distribution of blood pressure levels in the population, a large majority of hypertensive patients do have uncomplicated mild hypertension, and do require formal risk calculation.
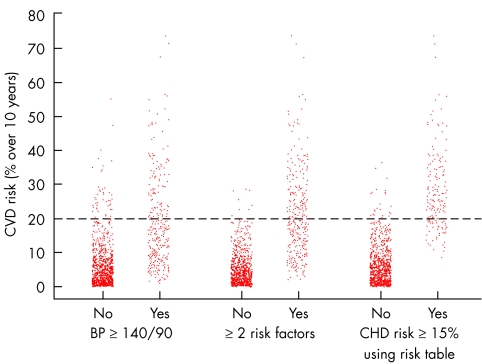
ESTIMATING ABSOLUTE RISK
Single risk factors such as blood pressure or serum cholesterol are very poor predictors of absolute risk. Counting the number of risk factors present improves accuracy, but the most accurate method of absolute risk estimation is to count and weight appropriately all the major risk factors for CVD.12 This is done using risk equations which are derived from large prospective epidemiological studies such as the Framingham study and use age, sex, systolic blood pressure, total cholesterol, high density lipoprotein (HDL) cholesterol, smoking history, and presence or absence of diabetes and LVH to compute CVD or CHD risk.1 Computer programs and paper based risk assessment tables or charts based on the Framingham risk function have been developed to enable doctors to calculate absolute risk easily and with reasonable accuracy.3,5,13,14 Figure 2 illustrates how a paper based risk assessment method based on the Framingham risk function can identify patients at high or low CVD risk much more accurately than methods based on counting risk factors or a single threshold for blood pressure. Thus, the risk assessment methods based on Framingham recommended by the British,5 New Zealand,2 and European14 guidelines all estimate absolute risk much more accurately than the methods based on counting risk factors recommended in the World Health Organization-International Society of Hypertension (WHO-ISH) and Joint National Committee (JNC) VI guidelines. The WHO-ISH and JNC-VI methods do not differentiate patients at high risk from those at low risk with acceptable accuracy.
Figure 2.
Cardiovascular disease (CVD) risks of individuals identified (“Yes”' columns) or not identified (“No” columns) as “high risk” using a single risk factor threshold (systolic blood pressure ≥ 140 mm Hg); counting risk factors (two or more risk factors for CVD); or a Framingham based method (the Sheffield table) to identify individuals with CVD risk ≥ 20% over 10 years. Note that use of a single risk factor gives very poor discrimination between people at low and high CHD risk. Counting risk factors improves the targeting of treatments but leads to identification for treatment of many low risk people. Framingham based methods such as the Sheffield table are more accurate in ensuring identification of those at high risk while avoiding treatment of those at low risk.
ACCURACY OF FRAMINGHAM RISK ESTIMATES
Framingham risk estimates are acceptably accurate in North American, UK, and northern European populations, but underestimate absolute risk in populations with much lower rates of cardiovascular disease than North America—for example, some Far Eastern and Mediterranean populations. Framingham may not be accurate in individuals from certain ethnic groups such as British Asians. The Framingham function incorporates the most powerful predictors of cardiovascular disease and omitted family history because its independent effect on risk was less than the other risk factors that were included. A family history of CHD death in a first degree relative before age 65 increases absolute CHD risk by a factor of 1.4, and this can be approximated simply by adding six years to age when calculating risk.
The Framingham risk function may seriously underestimate risk in those with persistent extreme values of blood pressure or total cholesterol:HDL ratio because it was derived from single measurements rather than long term averages as discussed previously. Patients with long term average blood pressure ≥ 160/100 mm Hg (or total cholesterol:HDL ratio ≥ 8.0) probably have considerably higher risk than is estimated by Framingham and should be treated.
There are also difficulties in estimating CHD/CVD risk in patients with treated hypertension. Use of the “on treatment” blood pressure underestimates risk because antihypertensive treatment does not completely reverse the increased CHD risk associated with hypertension. Conversely use of the pretreatment blood pressure will overestimate risk because risk is reduced by treatment. Overestimation of risk is preferable to underestimation, and pretreatment blood pressure should be used when possible. “Controlled” hypertension should be regarded as having CHD/CVD risk equivalent to that of untreated mild hypertension—for example, with systolic blood pressure of 160 mm Hg.
Absolute CHD/CVD risk increase with age and risk assessment is not therefore once only. Patients with uncomplicated mild hypertension and very low risk may be observed rather than treated, but they also need advice on lifestyle measures to reduce blood pressure. Blood pressure should be followed up and CHD risk should be reassessed periodically. Around 10% of patients with mild hypertension will progress to levels needing treatment (≥ 160/100 mm Hg) within 5–6 years.2 Furthermore, advancing age increases absolute CHD risk and most risk assessment methods can be used to “look forward” in time and predict when the CHD risk threshold needing treatment will be reached.
CHD OR CVD RISK?
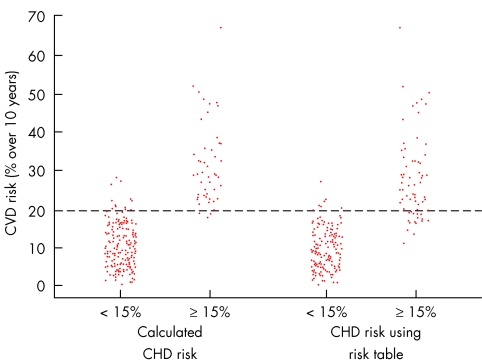
The Framingham risk function can calculate the absolute risk of any cardiovascular event (CVD risk) or only coronary events (CHD risk). The guidelines from New Zealand which first targeted antihypertensive treatment at absolute risk logically used absolute CVD rather than CHD risk because antihypertensive treatment prevents CHD events and strokes.3 Treatment of mild hypertension was recommended at CVD risk ≥ 20% over 10 years. However, decisions about statins and aspirin often have to be made in the same patient and these are aimed logically at CHD risk, not CVD risk, because they prevent myocardial infarction but have not been shown to prevent stroke in primary prevention. British guidelines recommend CHD risk assessment for all three preventative treatments4,5 to avoid confusion. CHD and CVD risks are not numerically equivalent but correlate highly with a ratio of 4:3.15 British guidelines recommend antihypertensive treatment at CHD risk ≥ 15% over 10 years and this is equivalent to CVD risk of 20% over 10 years. The accuracy of CHD risk 15% for targeting CVD risk 20% is acceptable and is shown on the left hand side of fig 3.
Figure 3.
Accuracy of CHD risk ≥ 15% over 10 years calculated from the full Framingham equation (shown on the left) or estimated using the Sheffield table (on the right) for predicting CVD risk ≥20% over 10 years in 202 patients with mild uncomplicated hypertension. Reproduced with permission from Wallis et al.15
ACCURACY OF RISK ESTIMATION METHODS
Computer programs based on the Framingham risk function are available and are slightly more accurate than paper based methods, and may be valuable if the program can be linked to the risk factor database. However, when data have to be entered to calculate risk, computers are considerably slower than paper based methods. Also computers are not available in every clinical setting. Precise risk calculation is of doubtful value when guidelines target only two risk thresholds that can be identified accurately by paper based methods (see below). Some of the computer programs available are over-elaborate and misleading. Some give CHD risk and stroke risk separately, which is unnecessary given their high correlation. Some give relative risk in addition to absolute risk. Relative risk may have a role in motivating patients towards dietary or lifestyle change but has no role in drug treatment decisions. Some computer programs incorporate “risk factors” that are not independent predictors of CHD risk for patient motivation or political correctness (for example, obesity and exercise levels). Finally some programs purport to show the effect of treatment on absolute risk but use inaccurate estimates of relative risk reduction.
Paper based risk estimation methods such as the Joint British Societies chart,5 the Sheffield table,13 and the New Zealand chart3 are used widely in the UK. These use all of the major risk factors in the Framingham function except for LVH, and use the total cholesterol:HDL cholesterol ratio rather than total cholesterol alone, unlike the European Task Force guidelines chart.14 The Joint British Societies chart and Sheffield table estimate 10 year risk of CHD events, whereas the New Zealand chart estimates five year risk of CVD events.
The accuracy of these methods for antihypertensive treatment decisions is determined by the proportion of patients with uncomplicated mild hypertension (140–159/90–99 mm Hg) classified correctly as having CVD risk over 10 years above or below the 20% threshold. High sensitivity is essential because the CHD risk threshold recommended in British guidelines is relatively conservative—high risk patients should not be left untreated. Specificity, meaning the proportion of low risk people identified correctly as not requiring treatment, is less important than the sensitivity—provided that people with very low risk are not identified for treatment. The accuracy of these methods for predicting CVD risk ≥ 20% over 10 years in patients with uncomplicated mild hypertension is shown in table 2 and illustrated for the Sheffield table on the right hand side of fig 3. The New Zealand chart was surprisingly inaccurate, despite using CVD risk, as it failed to identify 25% of patients with CVD risk ≥ 20%. The Sheffield table had higher sensitivity (81% v 75% for the New Zealand chart), but similar specificity (96% for both charts) even though it targets CVD risk indirectly through CHD risk. The Joint British Societies chart has unacceptably low sensitivity (63%) and fails to treat 37% of patients with mild hypertension who have high CVD risk (≥ 20% over 10 years). None of these methods identified any very low risk patients for treatment.
Table 2.
Accuracy (with 95% confidence intervals) of the New Zealand chart, Sheffield table, and Joint British Societies chart for predicting cardiovascular disease risk ≥ 20% over 10 years in 202 patients with uncomplicated mild hypertension
| New Zealand chart | Sheffield table | Joint Societies chart | |
| Sensitivity (%) | 75 (64 to 86) | 81 (71 to 91) | 63 (51 to 75) |
| Specificity (%) | 96 (92 to 99) | 96 (92 to 99) | 98 (95 to 100) |
| PPV (%) | 88 (79 to 97) | 89 (81 to 97) | 93 (85 to 100) |
| NPV (%) | 90 (85 to 95) | 92 (87 to 96) | 86 (80 to 91) |
NPV, negative predictive value; PPV, positive predictive value.
ADDITIONAL METHODS OF RISK ESTIMATION
Ambulatory blood pressure measurement
There has been considerable interest and debate over whether accurate blood pressure measurement by ambulatory blood pressure monitoring (ABPM) improves CVD risk prediction. ABPM does predict CVD risk, and the benefit from treatment, better than a limited number of clinic or surgery measurements, and there is some evidence that it may even be superior to the long term average of numerous clinic or surgery measurements.16 However blood pressure itself makes only a relatively small contribution to absolute risk, and improvements in accuracy of measurement will therefore alter absolute risk estimates little. ABPM is not needed routinely for decisions to start antihypertensive treatment. It is valuable for treatment decisions in patients who have uncomplicated moderate–severe hypertension (≥ 160/100 mm Hg) in clinic but low absolute CHD risk (< 15% over 10 years). In such patients the blood pressure level is the only indication for treatment and it is important to ensure accuracy. ABPM is also useful if there is unusual variability in blood pressure, if there are symptoms of hypotension with normal clinic measurements, or in resistant hypertension. ABPM is remarkably variable on repeated measurements and should be repeated when it influences treatment decisions. The average of the two results should be used. Blood pressure thresholds and targets for treatment should be adjusted downwards for ABPM readings by a factor of around 10/5 mm Hg. Thus in a low risk patient with no indications for treatment of mild hypertension, antihypertensive treatment should be started if the average daytime ABPM blood pressure is ≥ 150/95 mm Hg.
Echocardiography
LVH on ECG, defined as increased voltage plus T wave abnormality, doubles CHD risk. However, LVH with T wave abnormality is uncommon in hypertensive patients. Echocardiography is more “sensitive” for detecting LVH in patients with hypertension. Many doctors equate higher sensitivity with more powerful risk prediction and believe that echocardiography is superior to the ECG for CHD risk estimation. This is incorrect. Because echocardiographic LVH is more prevalent it is a much less powerful predictor of risk than LVH detected on an ECG. Quantitative measurement of left ventricular mass by echocardiography has been shown to add to the accuracy of risk prediction using the ECG, but the very small gain in accuracy is irrelevant for clinical decisions.17 There are also major problems with the accuracy of left ventricular mass measurement and test–retest variability, and disagreement over the definition of echo LVH and the thresholds of normality. Of course, when echocardiographic LVH is detected this represents end organ damage and so even mild hypertension should be treated regardless of the absolute risk estimate. Echocardiography should not be done routinely in hypertensive patients. It should be reserved for patients with “voltage criteria” LVH on ECG but no T wave abnormality in whom echocardiography often disproves the presence of true LVH, and in patients with other indications for echocardiography such as a heart murmur or symptoms suggestive of heart failure.
AT WHAT LEVEL OF CVD RISK IS TREATMENT JUSTIFIED?
British guidelines recommend treatment for those with CHD risk ≥ 15% over 10 years,4,5 and this is equivalent to the CVD risk threshold of ≥ 20% over 10 years recommended in the New Zealand guidelines.3 Around 25% of patients with uncomplicated mild hypertension have CHD risk ≥ 15% over 10 years.15 The relative risk reduction by treatment is 25%, and the absolute risk reduction with treatment at this level of risk is 5% over 10 years. This equates to a five year NNT of 40 to prevent one major cardiovascular complication. The WHO-ISH and JNC-VI guidelines advocate risk assessment but are not explicit on the level of risk to be treated. However, their risk assessment methods lead to treatment of very low risk patients and to a much larger NNT. The minimum acceptable level of absolute benefit from antihypertensive treatment can be debated but really needs to be studied. Antihypertensive treatment targeted at the level of risk recommended in British guidelines is undoubtedly safe, meaning that benefit clearly outweighs any serious harm. Cost effectiveness is also well within generally accepted limits. However, the level of absolute benefit at which treatment becomes worthwhile is extremely difficult to assess. The chance of a cardiovascular complication being prevented, and the value of this, must be weighed against possible harm, discomfort, and inconvenience of long term tablet taking. Doctors can debate this endlessly, but the correct answers can only come from formal study of the choices of fully informed patients or potential patients. Little research has been done to determine what benefit (or NNT) is generally acceptable to patients. One study suggested that most would opt to take preventative treatment for an NNT of 40, while another suggested they would not. It is doubtful whether fully informed people would choose to take treatment for the extremely low chance of benefit (or high NNT) that follows from the WHO-ISH or JNC-VI guidelines.
PROBLEMS WITH TARGETING ABSOLUTE RISK
The principle of targeting treatment at high absolute CHD risk rather than high cholesterol is now accepted for statin treatment, but the similar policy for antihypertensive treatment is less widely known and practised. Antihypertensive treatment was targeted at defined blood pressure thresholds for decades, and the idea that treatment to lower blood pressure should not be targeted at blood pressure but at CHD risk is difficult for some to grasp. This difficulty is compounded by the intense interest in more precise measurement of blood pressure using ABPM, and ever more detailed analyses of ABPM patterns.
The overwhelming influence of age on CHD risk leads to treatment of mild hypertension in older people while most younger people are observed rather than treated.18 European guidelines for CHD prevention suggest that CHD risk should be projected to age 60 to target treatment.14 This may be better than using blood pressure thresholds alone, but in essence it identifies those at high relative risk rather than high absolute risk. Many of those treated will have extremely low absolute risk and may be disadvantaged by treatment. One reason for this recommendation may be concern that failure to treat mild hypertension in young people may allow development of LVH or other target organ damage. Once established, target organ damage confers a bad prognosis that cannot be completely reversed by treatment. However, the risk of developing LVH in patients with uncomplicated mild hypertension is remote.2 Concern has been expressed that absolute risk reduction may not be the best measure of benefit because it assumes that the prevention of a CVD event has equal worth in all people regardless of age.18 Prevention of death in a younger person may save more years of extra life than prevention of death in an older person, and similarly prevention of a non-fatal complication may attain more quality adjusted life-years. Therefore prevention of a cardiovascular complication may be more valuable in younger patients. If so, applying a uniform absolute risk threshold for treatment regardless of age would disadvantage the young.
Methods of targeting treatment at total life-years gained, total quality adjusted life-years gained, or life-years gained per year of treatment have been examined.19 The latter method makes surprisingly little difference to the age of introducing treatment when compared to the use of a single absolute risk threshold.20 Furthermore there will always be a trade off in these methods. Any reduction in the level of absolute risk treated or absolute benefit sought will narrow the margin between benefit and harm from treatment. Younger people may value benefit more highly, but will they take more kindly to rare but serious side effects, subjective side effects, inconvenience, and the need to take tablets? One suspects not.
Our own view is that the question of whether the risk threshold should differ with age, and how, is unlikely to be resolved by any mechanistic method. Fully informed patients should decide what benefit they require from treatment, not their doctors, and there is a need to develop better methods to study patient choice. Only then will we know whether older people feel that they have had a “good innings” and do not wish treatment, or whether they have attended many funerals and wish to postpone their own. Are young people keen to take treatment to prevent complications 20–40 years in the future or are their priorities elsewhere?
Key points.
The absolute risk of cardiovascular disease dictates the absolute benefit from antihypertensive treatment. Absolute risk assessment is essential to ensure high risk patients are treated while avoiding treatment of low risk patients
In certain patients formal risk assessment is unnecessary because certain risk factors always place patients at high risk
Where formal risk assessment is necessary, methods based on the Framingham risk function are preferable and a number of computer programs and simple paper based risk assessment methods are available
CHD risk multiplied by 4/3 is an acceptable surrogate for CVD risk.
Additional refinements in risk factor measurement such as ambulatory blood pressure measurement or echocardiography usually add little information to formal risk estimates
The threshold of CVD risk at which treatment is justified is a matter for continued research and debate
CONCLUSION
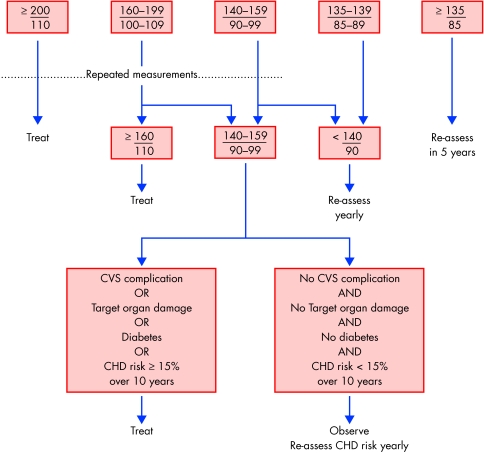
There is a consensus in the UK that antihypertensive treatment should be targeted at absolute risk rather than at any single blood pressure threshold. A summary of the recommendations for targeting of antihypertensive treatment by the British Hypertension Society4 is shown in fig 4.
Figure 4.
Summary of recommendations in the British Hypertension Society guidelines for targeting of antihypertensive treatment.4
Supplementary Material
REFERENCES
- 1.Anderson KM, Odel PM, Wilson PWF, et al. Cardiovascular disease risk profiles. Am Heart J 1991;121:293–8. This paper contains the Framingham risk functions. [DOI] [PubMed] [Google Scholar]
- 2.Ramsay LE. The hypertension detection and follow-up program 17 years on. JAMA 1997;277:167–70. A discussion outlining how absolute benefit is predicted by absolute risk and the implications of this for antihypertensive treatment guidelines. [DOI] [PubMed] [Google Scholar]
- 3.New Zealand Ministry of Health. Guidelines for the management of mildly raised blood pressure in New Zealand. Wellington: Core Services Committee, Ministry of Health, 1995. These were the first guidelines to advocate the use of absolute risk in antihypertensive treatment decisions.
- 4.Ramsay LE, Williams B, Johnston GD, et al. British Hypertension Society guidelines for hypertension management 1999: summary. BMJ 1999;319:630–5. Summary version of British Hypertension Society guidelines. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wood D, Durrington P, Poulter N, et al on behalf of the British Cardiac Society, British Hyperlipidaemia Association, British Hypertension Society and endorsed by the British Diabetic Association. Joint British recommendations on prevention of coronary heart disease in clinical practice. Heart 1998;80(suppl 2):S1–29. Guidelines containing the Joint British Societies chart. [PMC free article] [PubMed] [Google Scholar]
- 6.Collins R, Peto R. Antihypertensive drug therapy: effects on stroke and coronary heart disease. In: Swales JD, ed. Textbook of hypertension. Oxford: Blackwell Scientific, 1992:1156–64.
- 7.Madhavan S, Alderman MH. The potential effect of blood pressure reduction on cardiovascular disease. Arch Intern Med 1981;141:1583–6. [PubMed] [Google Scholar]
- 8.Cook RJ, Sackett DL. The number needed to treat: a clinically useful measure of treatment effect. BMJ 1995;310:452–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glasziou PP, Irwig LM. An evidence based approach to individualising patient treatment. BMJ 1995;311:1356–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoes AW, Grobbee DE, Lubson J. Does drug treatment improve survival? Reconciling the trials in mild to moderate hypertension. J Hypertens 1995;13:805–11. This paper attempts to quantify the risk of serious harm from antihypertensive treatment. It has methodological weaknesses outlined in an accompanying editorial by Eggar. [PubMed] [Google Scholar]
- 11.Ramsay LE. Mild hypertension: treat patients, not populations. J Hypertens 1985;3:449–55. [PubMed] [Google Scholar]
- 12.Grover SA, Coupal L, Hu X-P. Identifying adults at increased risk of coronary disease. How well do the current cholesterol guidelines work? JAMA 1995;274:801–6. [PubMed] [Google Scholar]
- 13.Wallis EJ, Ramsay LE, Haq IU, et al. Coronary and cardiovascular risk estimation for primary prevention: validation of a new Sheffield table in the 1995 Scottish health survey population. BMJ 2000;320:671–6. This paper contains a colour version of the updated Sheffield table, a detailed assessment of its accuracy, and a critical assessment of the use of absolute risk in primary prevention. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wood D, De Backer G, Faergeman O, et al with members of the Task Force. Prevention of coronary heart disease in clinical practice. Recommendations of the second joint task force of European and other societies on coronary prevention. Eur Heart J 1998;19:1434–503. [DOI] [PubMed] [Google Scholar]
- 15.Wallis EJ, Ramsay LE, Haq IU, et al. Is coronary risk an accurate surrogate for cardiovascular risk for treatment decisions in mild hypertension? A population validation. J Hypertens 2001;19:691–6. This paper examines the relation between coronary and cardiovascular risk in patients with mild hypertension in detail. [DOI] [PubMed] [Google Scholar]
- 16.Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic hypertension in Europe trial investigators. JAMA 2000;282:539–46. [DOI] [PubMed] [Google Scholar]
- 17.Levy D, Garrison RJ, Savage MS, et al. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham heart study. N Engl J Med 1990;322:1561–6. [DOI] [PubMed] [Google Scholar]
- 18.Simpson FO. Guidelines for antihypertensive therapy: problems with a strategy based on absolute cardiovascular risk. J Hypertens 1996;14:683–9. This editorial gives a full discussion of the problems with targeting treatment at absolute risk relating to patient age. [DOI] [PubMed] [Google Scholar]
- 19.Ulrich S, Hingorani AD, Martin J, et al. What is the optimal age for starting lipid lowering treatment? A mathematical model. BMJ 2000;320:1134–40. One of the first articles to show how preventative treatments could be targeted at life-years gained rather than absolute risk, although it has methodological weaknesses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jackson PR, Wallis EJ, Ramsay LE. Optimal age for starting lipid lowering treatment. Adjusted data do not justify a lower optimal age. BMJ 2000;34:637. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.