Abstract
Objectives: To investigate the impact of the redefinition of the diagnostic criteria for myocardial infarction on its apparent incidence in a non-selected and representative series of patients admitted with acute chest pain.
Design: Single centre prospective study.
Setting: Medical assessment unit and cardiology wards of an inner city university hospital.
Patients: 80 consecutive patients aged over 25 years admitted with suspected ischaemic acute chest pain (excluding those where the ECG indicated definite myocardial infarction).
Interventions: Measurement of concentrations of conventional cardiac biomarkers (creatine kinase and its MB isoenzyme, CK-MB) and concentrations of the highly specific diagnostic indicator of myocardial damage, cardiac troponin I (cTnI) 12–24 hours after the onset of acute chest pain.
Main outcome measures: Frequency of myocardial infarction as assessed by conventional diagnostic criteria (creatine kinase and CK-MB) plus clinical symptoms of infarction, versus frequency of infarction based on high sensitivity troponin assays.
Results: Among patients with acute coronary syndromes but non-diagnostic ECG changes, 40% (32/80) fulfilled the new criteria for myocardial infarction using high sensitivity cTnI measurement, compared with 29% (23/80) using the conventional diagnostic criteria for myocardial infarction.
Conclusions: The implications of the redefinition of myocardial infarction on patients, their care, and the use of health care resources are substantial.
Keywords: cardiac troponin I, myocardial infarction, epidemiology
The World Health Organization defined myocardial infarction by the combination of two of three characteristics: typical symptoms of infarction (that is, chest pain or discomfort), a rise in plasma or serum cardiac enzymes, and a typical ECG pattern involving the development of Q waves.1,2 The measurement of creatine kinase and its MB isoenzyme (CK-MB) are still often used as markers of myocardial damage. However, the release of cardiac troponins into the blood provides the most sensitive and specific biochemical marker of myocardial damage that is currently available.3–5
The troponin complex comprises three distinct structural proteins (troponins C, I, and T) that are encoded by different genes.5,6 The complex is located on the thin filament of the contractile apparatus in both skeletal and cardiac muscle tissue and regulates the calcium dependent interaction of myosin and actin.6 Isoforms of troponin I and T have been identified that are specific to the myocardium, and these are measured routinely using immunoassays.3–6 Clinical studies have shown that cardiac troponin I (cTnI) and T (cTnT) are similarly effective for detecting myocardial damage.6–9
Cardiac troponins are released within the first few hours after the onset of myocardial necrosis, typically reaching a peak concentration 12–24 hours after myocardial infarction.7,8 In this regard the time course is similar to creatine kinase, but troponins, because of their long plasma half life, stay raised when creatine kinase has returned to values within the reference range.5 In contrast to creatine kinase and CK-MB, cardiac troponins are undetectable in normal healthy subjects using most of the current assay systems available. This appears to reflect the relatively poor sensitivity of most assays for troponins. An exception is the Dade-Behring Stratus CS assay, which claims sensitivity sufficient to allow the detection of cTnI in a proportion of healthy individuals with a high degree of precision.5–9
The American College of Cardiology and the European Society of Cardiology (ACC/ESC) have redefined the diagnostic criteria for myocardial infarction. Under this new definition, the measurement of cardiac troponins becomes the new gold standard diagnostic indicator of myocardial injury.10 The consensus documents from these societies define a raised value of cardiac troponins as a measurement exceeding the 99th centile of the values obtained from a reference group.10 They also propose that the acceptable imprecision of the troponin measurement at the 99th centile should be < 10% coefficient of variation (CV). To satisfy the new diagnostic criteria for myocardial infarction, a raised cardiac troponin value should be accompanied by at least one of the following: ischaemic symptoms; the development of pathological Q waves on the ECG; ECG changes indicating ischaemia (ST segment elevation or depression); or coronary artery intervention (for example, coronary angioplasty).10
Few of the current assays for troponins are capable of meeting the performance criteria suggested by the ACC/ESC,6 so clinical cut off points must be determined for these insensitive assays. As the “functional sensitivity”of most assays for cTnI (defined as the concentration of troponin that has a 20% CV taken from a precision profile) exceeds the concentration found in any healthy individual, it could be argued that functional sensitivity could be used as a cut off for insensitive cTnI assays. Others have suggested, however, that the troponin concentration that meets the goal of 10% CV imprecision should be used as the diagnostic cut off for myocardial infarction until the goal of 10% CV can be achieved at the 99th centile of the reference population.
These new diagnostic criteria are likely to result in more patients being diagnosed as having myocardial infarction, but the percentage of patients recategorised from angina to myocardial infarction will be critically dependent on the performance of the troponin assay used.
In this study we aimed to investigate the impact of the ACC/ESC redefinition of myocardial infarction on the apparent incidence of infarction in unselected patients admitted with suspected acute coronary syndromes, from a geographically defined population. For this we have used the Dade-Behring cTnI Stratus CS assay (Dade-Behring Inc, Milton Keynes, Buckinghamshire, UK), which meets the performance standards recommended by the ACC/ESC.5 The hypothesis was that among patients with abnormal but non-diagnostic ECG changes, the application of this new definition would cause the apparent incidence of myocardial infarction to rise. If confirmed, this would not only have significant implications for individual patients, with respect to psychological status, life insurance, and occupation, but would also affect measures of cardiovascular epidemiology and the wider use of healthcare resources. We have also studied the influence of using an assay for cTnI that has a performance more typical of the assays currently used by most laboratories (Immuno 1, Bayer Diagnostics UK, Newbury, Berkshire, UK).5
METHODS
Criteria for selection of patients
Consecutive patients admitted over a six week period to the medical assessment unit and the cardiology wards of the Royal Infirmary of Edinburgh with chest pain at rest or on minimal exertion, consistent with myocardial ischaemia, were eligible for inclusion in the study. Patients were included if they had given informed consent, had no history of trauma, and if no other non-cardiac cause of chest pain had been diagnosed (determined from inpatient case notes). Patients were only included if their chest pain had begun within the previous 24 hours, was of greater than 10 minutes’ duration, and was accompanied by an abnormal resting 12 lead ECG. We excluded patients with renal failure or with ECG evidence of an evolving myocardial infarct based upon diagnostic ST elevation (> 1 mm in two leads).11 In all, 80 patients from 96 admissions qualified for inclusion in the study, which was approved by the Lothian research ethics committee. The inpatient case notes were reviewed two weeks or more after discharge to establish the final clinical diagnosis of each patient. In each case, diagnosis was made blind to the results from the sensitive troponin assay and the CK-MB results.
Sample collection and measurement of cardiac markers
Venepuncture was performed on each patient using a 6.4 ml Sarstedt Li/heparin tube 12–24 hours after the onset of chest pain. Plasma was prepared by centrifugation and used immediately for the measurement of creatine kinase activity. Portions of plasma were frozen for subsequent measurement of cTnI and CK-MB.
Cardiac troponin I (CTNI) analysis
Cardiac troponin I was measured using both the Dade-Behring Stratus CS and the Bayer Immuno 1 immunoassay systems. The clinical cut off limits (based on the 99th centile of a reference population), functional sensitivity (20% CV), and 10% CV for each of the two assays are given in table 1. The Bayer Immuno 1 system is used for “routine” troponin I measurements in our hospital.
Table 1.
Clinical cut off limits on Dade-Behring Stratus CS and Bayer Immuno 1 cTnI immunoassays
| Clinical cut off limits | Stratus CS (μg/l) | Immuno 1 (μg/l) |
| 99th centile | ≥0.07 | Not applicable |
| 10% CV | ≥0.06 | ≥0.35 |
| Functional sensitivity (20% CV) | ≥0.04 | ≥0.20 |
CV, coefficient of variation.
Analyses were repeated in 14 samples (17.5%) using both cTnI assays because either the result was near the functional sensitivity of one assay (functional sensitivity ± 0.01 μg/l) or the cTnI was only detectable by the Dade-Behring Stratus CS assay.
Creatine kinase and CK-MB analysis
The activity of creatine kinase was measured using the Olympus Diagnostics AU640 assay (Olympus Diagnostics UK, Southall, Middlesex, UK). Values exceeding 200 U/l in male subjects and 150 U/l in female subjects were considered to be raised. The concentration of the MB isoenzyme of creatine kinase (CK-MB) was measured using the Ortho-Clinical Diagnostics Vitros ECi automated immunoassay system (Ortho-Clinical Diagnostics, Amersham, Buckinghamshire, UK). Values above 2.37 μg/l for heparin plasma samples were considered significant for this assay.
Statistical analyses
Analyses of the data were carried out using Microsoft Excel software. Statistical comparisons of the data were undertaken using the χ2 test. Significance was assumed at a probability value of p < 0.05.
RESULTS
Demography and sample collection
Eighty consecutive patients were enrolled in the study in the six week period. Their baseline characteristics are shown in table 2. The median duration of ischaemic chest pain was two hours (range 10 minutes to 23 hours). A history of a previous myocardial infarction was present in 44% of the patients (35/80); only 9% (7/80) had no past cardiac history. The median time interval from the onset of chest pain to venepuncture was 15 hours 35 minutes (range 12 hours to 23 hours 55 minutes).
Table 2.
Baseline characteristics of the patient group
| Number of patients | 80 |
| Median age (years) | 63.5 |
| Age range (years) | 39 to 96 |
| Sex ratio (male:female) | 1.6 (49:31) |
ECGs
All of the patients recruited had abnormal ECGs upon admission: 86.3% (69/80) had ischaemic changes (T wave inversion with or without ST depression), 11.3% (9/80) had bundle branch block (6.3% right, 5% left), and 2.5% (2/80) had paced rhythms.
Final clinical diagnoses
The inpatient case notes were reviewed two weeks or more after discharge to establish the final clinical diagnosis for each patient (table 3). Two patients (2.5%) diagnosed with myocardial infarction died during the period of the study. The causes of death were a ruptured abdominal aortic aneurysm and severe cardiac failure.
Table 3.
Final clinical diagnosis upon discharge
| Final clinical diagnosis | Number of patients (%) |
| Unstable angina | 42 (52.5) |
| Angina (type unspecified) | 19 (23.8) |
| Myocardial infarction | 13 (16.3) |
| Non-cardiac causes (e.g. musculoskeletal) | 5 (6.3) |
| Other cardiac causes (e.g. pericarditis) | 1 (1.3) |
Influence of troponin I assay system and cut off limit used on diagnosis
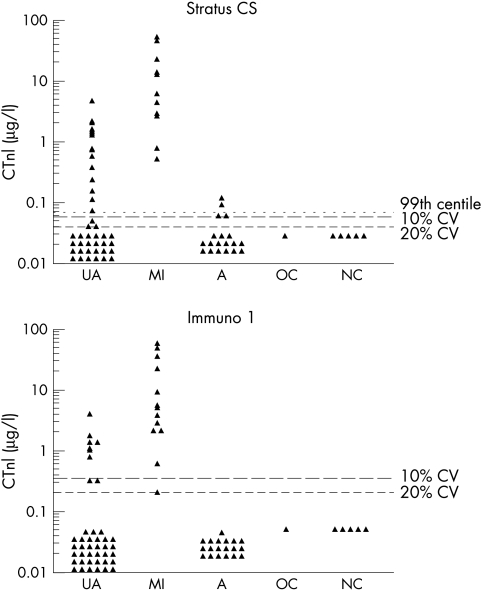
Figure 1 shows the data obtained by the two assays for the 80 patients. The influence of the assay system and cut off limit used on the number of patients categorised as having a myocardial infarct is shown in table 4.
Figure 1.
Troponin I concentrations measured by two assay methods for each of the final diagnostic categories. A, angina of unspecified type; CTnI, cardiac troponin I; CV, coefficient of variation; MI, myocardial infarction; NC, non-cardiac cause; OC, other cardiac cause; UA, unstable angina.
Table 4.
Number of cases of myocardial infarction detected using different diagnostic methods
| Diagnostic method | Number of cases of MI | Per cent of cases |
| Stratus CS (10% CV) | 32 | 40 |
| Stratus CS (functional sensitivity, 20% CV) | 35 | 43.8 |
| Stratus CS (99th centile) | 30 | 37.5 |
| Immuno 1 (10% CV) | 19 | 23.8 |
| Immuno 1 (functional sensitivity, 20% CV) | 28 | 35 |
| Vitros CK-MB | 23 | 28.8 |
| Creatine kinase | 10 | 12.5 |
| Final clinical diagnosis on discharge | 13 | 16.3 |
99th Centile cut off
Thirty patients (37.5%) had a cTnI that fell above the 99th centile on Dade-Behring Stratus CS. Each of the 13 patients (16.3%) with a final diagnosis of myocardial infarction had a troponin above the 99th centile, but an additional 15 patients (18.8%) with unstable angina and two patients (2.5%) with angina would be assigned a diagnosis of myocardial infarction using the 99th centile figure. It was not possible to define a 99th centile cut off for the Bayer Immuno 1 assay owing to the insensitivity of this assay.
Cut off at 10% CV
Only 19 patients (23.8%) had cTnI concentrations above the 10% CV cut off using the Bayer Immuno 1 system, and one patient with a diagnosis of myocardial infarction on discharge failed to achieve a cTnI that was above this cut off point. For the Dade-Behring Stratus CS system, the 10% CV cut off was a concentration that was below the 99th centile of the reference population.
Functional sensitivity (20% CV)
The use of functional sensitivity as a cut off point for the Bayer Immuno 1 system identified 29 patients (36.3%) in whom cTnI was detectable (and therefore above the 99th centile of the reference population). This compared with only 19 patients (23.8%) who had a cTnI above the 10% CV cut off figure for this assay system. With the Dade-Behring Stratus system, 35 patients (43.8%) were found to have a cTnI that was detectable using “functional sensitivity” as a cut off.
Creatine kinase and CK-MB
Only 10 patients (12.5%) had creatine kinase activities that were above the reference range and were thus consistent with myocardial damage; nine of these patients had a final clinical diagnosis of myocardial infarction. Twenty three patients (28.8%) had CK-MB levels indicative of myocardial damage, all of whom had a positive cTnI result using the Dade-Behring Stratus CS assay.
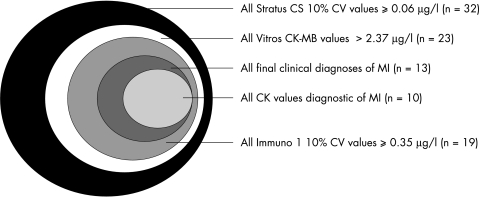
The number and distribution of cases of myocardial infarction detected using the different diagnostic methods are summarised in table 4 and fig 2.
Figure 2.
Diagram illustrating the number of cases of myocardial infarction detected using different diagnostic methods. The area of circle is proportional to the number of patients fulfilling the respective diagnostic thresholds.
Statistical analyses
A significant relation was found between the Dade-Behring Stratus CS assay and the final clinical diagnoses (p< 0.001, χ2). The relation between the Dade-Behring Stratus CS and the Bayer Immuno 1 cTnI assays was also found to be significant (p = 0.01, χ2). No other significant relation was found between the different diagnostic methods.
DISCUSSION
Measurement of biochemical markers of myocardial injury has made an important contribution to the definition of myocardial infarction for many years. With the advent of highly specific and sensitive cardiac troponin assays has come the possibility of redefining myocardial infarction. One such definition is that proposed by the ACC/ESC.10 This prospective study has determined the impact of the new diagnostic criteria for myocardial infarction as stated by this new definition in a non-selected and representative series of patients admitted with acute chest pain.
In our study, 23 patients (29%) had a myocardial infarct using the conventional WHO criteria,1,2 while 30 patients (37.5%) had an infarct diagnosed using the ACC/ESC guidelines.10 Based on this unselected population, the use of the new definition of myocardial infarction, when applied to patients with abnormal but non-diagnostic ECG changes, would identify approximately 135 additional patients with myocardial infarction a year in our hospital (pro rata) who would not otherwise be classified as having a myocardial infarct. Published data suggest that the conventional markers of myocardial infarction are relatively poor at detecting patients with myocardial injury5,6 and our data support this view. We found that measurement of total creatine kinase activity was insensitive at identifying patients with myocardial injury, being raised in only 10 (12.5%) of the 80 patients we studied. Measurement of CK-MB was superior to creatine kinase in that CK-MB was raised in 23 of the 80 patients (28.8%). Nevertheless CK-MB was raised in only 76% of the patients (23/30) who had an abnormal cTnI result as defined by the ACC/ESC and, importantly, in no patient was a raised CK-MB level detected when cTnI was undetectable by the Dade-Behring Stratus CS system.
The high sensitivity of the Dade-Behring Stratus CS cTnI assay meets the new diagnostic and performance criteria as defined by the ACC/ESC.10 Unfortunately most other assay systems for cTnI are not sufficiently sensitive to detect cTnI in the healthy population and are unable to meet the analytical performance characteristics of 10% CV at the 99th centile of the healthy population. For these insensitive cTnI assays it has been suggested that the cut off point should be the concentration that has an imprecision of 10% CV. When applied to the Bayer Immuno 1 system, only 19 patients were identified with myocardial infarction (as compared to 30 identified using the ACC/ESC guidelines).
A more practical and widely accepted cut off for those assays that fail to detect cTnI in the healthy population is to use the so called “functional sensitivity” of the assay. The concept of functional sensitivity has been universally adopted since 1990 for characterising the detection limit of thyrotropin assays.12 It is derived by determining the concentration of analyte that has a between-assay CV of 20% in routine use and represents the lowest concentration of analyte that can reliably be detected.12 With an insensitive assay, any detectable cTnI must be greater than the 99th centile of the reference population, so it follows that “functional sensitivity” serves as an appropriate cut off point. Our data from Bayer Immuno 1 analyser illustrate this, in that 28 patients with myocardial infarction were detected on the basis of functional sensitivity, a significant improvement on the use of the 10% CV cut off, which identified only 19 patients.
Our data show that the use of the high sensitivity cTnI immunoassay in conjunction with the ACC/ESC guidelines would identify a substantial and additional proportion of patients with myocardial infarction compared with current regimens. Based on registry data (GRACE, global registry of acute coronary events)13 and trial populations, such patients are nevertheless at increased risk of coronary events and death compared with those who are troponin negative.14,15 Identification of such patients facilitates early treatment, interventional therapy, and secondary prevention in those who might otherwise not receive it.16
Recent clinical trials have shown that patients with detectable cTnI specifically benefit from treatment with glycoprotein IIb/IIIa antagonists or low molecular weight heparin, while no such benefit was observed in patients without troponin elevation.17–19 Furthermore, the use of high sensitivity cTnI measurement would result in improved specificity for excluding the diagnosis of myocardial infarction, potentially leading to reduced hospital stays.10 In addition it may also be used to predict outcome in patients presenting with acute coronary syndromes. Published data consistently show that patients with raised levels of troponins but without apparent elevation of other cardiac biomarkers have an unfavourable short term and long term clinical outcome when compared with those without troponin elevation.3,14–16
Although cardiac troponins are undoubtedly useful, problems still remain. Standardisation of cTnI assays is unresolved, with different assays giving numerically different results (particularly at the lower end of their range).6 Thus if sensitive assays for cTnI did become available from several manufacturers it is likely that the 99th centile cut off point would vary considerably between centres. A further limitation to the use of cardiac troponins in emergency departments is that they take several hours to rise after symptom onset,3–6 often producing negative values upon admission. Thus unless samples are taken at appropriate times, cTnI measurements may be misleading. Furthermore, 30% of patients with low risk clinical features and negative cTnI values throughout the first 12 hours of admission have severe underlying coronary artery disease.20,21 Whether this observation holds using the new sensitive assays requires to be determined.
A further important limitation of cardiac troponins concerns the long plasma half life of the protein, which means that concentrations stay raised for up to 14 days after myocardial infarction. This restricts their usefulness in detecting reinfarction.3,6 Furthermore they cannot be used to guide reperfusion treatment in patients who present within 2–3 hours of symptom onset. Laboratory assays can result in additional delays (and rapid assays for near-patient testing may be less accurate). Thus the acute management of a myocardial infarction must usually be started before the cTnI result is available.22
Despite their specificity for cardiac myocyte injury, sensitive assays of troponin elevation can detect myocyte injury unrelated to atheromatous plaque rupture and thrombosis. Cardiac troponins are detectable in serum from patients with pulmonary embolism, cardiac failure, myocarditis, and renal failure, possibly reflecting subclinical myocyte damage.9
Conclusions
In a non-selected series of patients admitted with acute ischaemic chest pain but non-diagnostic ECG changes, the use of high sensitivity cTnI measurements and the implementation of the new ACC/ESC guidelines will identify approximately twice as many patients with myocardial infarction than with current clinical practice. In addition, this study shows that cardiac troponin measurements are diagnostically superior to measurements of creatine kinase or its isoenzyme MB. The implications of the redefinition of myocardial infarction are substantial, not only for individual patients but also for society and for the use of health care resources.
Acknowledgments
This study was supported by a grant from the Clinical Audit Committee of the Royal Infirmary of Edinburgh, Lauriston Place, Edinburgh, UK.
Abbreviations
ACC, American College of Cardiology, CK, creatine kinase
CV, coefficient of variation
ESC, European Society of Cardiology
WHO, World Health Organization
REFERENCES
- 1.WHO Working Group. The establishment of ischaemic heart disease registers (report of fifth working group). Copenhagen: World Health Organization. WHO Reg Publ Eur Ser 1972;821(suppl 5).
- 2.Task Force. Task force on standardization of clinical nomenclature. Circulation 1979;59:607–9. [DOI] [PubMed] [Google Scholar]
- 3.Hillis GS, Fox KAA. Cardiac troponins and risk stratification of patients with chest pain. BMJ 1999;319:1451–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katus HA, Agrawal B. Foreword. Eur Heart J 1998;19(suppl N1).
- 5.Collinson PO, Boa FG, Gaze DC. Measurement of cardiac troponins. Ann Clin Biochem 2001;38:423–49. [DOI] [PubMed] [Google Scholar]
- 6.Collinson PO. Troponin T or troponin I or CK-MB (or none?). Eur Heart J 1998;19(suppl N):N16–24. [PubMed] [Google Scholar]
- 7.Bertinchant JP, Larue C, Pernel I, et al. Release kinetics of serum cardiac troponin I in ischaemic myocardial injury. Clin Biochem 1996;29:587–94. [DOI] [PubMed] [Google Scholar]
- 8.Wu AHB, Feng YJ. Biochemical differences between cTnT and cTnI and their significance for diagnosis of acute coronary syndromes. Eur Heart J 1998;19(suppl N):N25–9. [PubMed] [Google Scholar]
- 9.Hamm CW, Goldmann BU, Heeschen C, et al. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med 1997;337:1648–53. [DOI] [PubMed] [Google Scholar]
- 10.JESC/ACC Committee. Myocardial infarction redefined – a consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J 2000;21:1502–13; J Am Coll Cardiol 2000;36:959–69. [DOI] [PubMed] [Google Scholar]
- 11.Hampton JR. The ECG made easy, 5th ed. Edinburgh: Churchill Livingstone, 2000.
- 12.Nicoloff JT, Spencer CA. The use and misuse of the sensitive thyrotropin assays. J Clin Endocrinol Metab 1990;71:553–8. [DOI] [PubMed] [Google Scholar]
- 13.Fox KAA, Goodman SG, Klein W, et al. Management of acute coronary syndromes. Variations in practice and outcome: findings from the Global Registry of Acute Coronary Events (GRACE). Eur Heart J 2002;23:1177–89. [DOI] [PubMed] [Google Scholar]
- 14.Antman EM, Tanasijevic MJ, Thompson B, et al. Cardiac specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med 1996;335:1342–9. [DOI] [PubMed] [Google Scholar]
- 15.Galvani M, Ottani F, Ferrini D, et al. Prognostic influence of elevated values of cardiac troponin I in patients with unstable angina. Circulation 1997;95:2053–9. [DOI] [PubMed] [Google Scholar]
- 16.Lindahl B, Diderholm E, Lagerqvist B, et al. Invasive versus non-invasive strategy in relation to troponin T level and ECG findings: a FRISC 2 sub-study. Eur Heart J 2000;21(abstract suppl):2531. [Google Scholar]
- 17.Bertrand ME, Simoons ML, Fox KAA. et al. Task force report: management of acute coronary syndromes without persistent ST segment elevation. Eur Heart J 2000;21:1406–32. [DOI] [PubMed] [Google Scholar]
- 18.Hamm C, Heeschen C, Goldmann B, et al. Benefit of abciximab in patients with refractory unstable angina in relation to serum troponin level. N Engl J Med 1999;340:1623–9. [DOI] [PubMed] [Google Scholar]
- 19.FRISC II investigators. Long-term low-molecular-weight heparin in unstable coronary-artery disease: FRISC II prospective randomized multi-centre study. Lancet 1999;354:701–7. [PubMed] [Google Scholar]
- 20.Hillis GS, Oliner C, Zhao N, et al. The prevalence and severity of coronary artery disease in “low-risk” patients with chest pain. Heart 1999;81:614–20. [Google Scholar]
- 21.Brscic E, Chiappino I, Bergerone S, et al. Prognostic implications of detection of troponin I in patients with unstable angina pectoris. Am J Cardiol 1998;82:971–3. [DOI] [PubMed] [Google Scholar]
- 22.Richards A, Lainchbury JG, Nicholls MG. Unsatisfactory redefinition of myocardial infarction. Lancet 2001;357:1635–6. [DOI] [PubMed] [Google Scholar]