Abstract
The discrete form of subaortic stenosis is thought to be an acquired lesion, the aetiology of which may be a combination of factors which include an underlying genetic predisposition, turbulence in the left ventricular outflow tract, and various geometric and anatomical variations of the left ventricular outflow tract. A review of hypotheses relating to its aetiology is provided
Keywords: subaortic stenosis, aortoseptal angle, double outlet right ventricle, ventricular septal defect
Rheology, as the science of flow and deformation of matter, would seem to apply to the discrete form of fixed subaortic stenosis, the development of which is poorly understood. It has become apparent in recent years that this is an acquired lesion that is rarely seen in the newborn or neonatal period.1–4 Recent theories about the pathophysiological mechanism of its formation suggest an abnormal underlying endothelial substrate that is stimulated to undergo proliferation by sheer stresses caused by abnormal flow patterns and chronic turbulence. The lesion increases in severity, and progression of obstruction occurs if the initially discrete obstruction is not adequately relieved at an early age. Ultimately, increasing left ventricular outflow obstruction will lead to concentric left ventricular hypertrophy with the potential for diffuse ischaemic myocardial damage and rhythm disturbances in the long term, to aortic valve insufficiency, and to bacterial endocarditis.5
ANATOMICAL SITES AND COMMON ASSOCIATIONS
Subvalvar subaortic stenosis is a relatively uncommon type of left ventricular outflow obstruction and accounts for approximately 8–30% of subaortic obstruction.6,7 Most commonly, a discrete fibrous membrane or fibromuscular collar encircles the left ventricular outflow tract just below the aortic valve. Rarely, a long diffuse fibromuscular narrowing obstructs the left ventricular outflow tract for several centimetres.8 Associated cardiac malformations—especially coarctation of the aorta and ventricular septal defect (VSD)—occur in approximately 65% of patients.1,7 As many as 51% of patients with a VSD and discrete subaortic stenosis have been found to have deviation of the outlet septum. It is thought that deviation of the interventricular septum (anterior or posterior) results in the development of a fibrous shelf which contributes to the development of subaortic stenosis because the deviated septum causes a disturbance of the flow pattern in the left ventricular outflow tract.9
RECENT AETIOLOGICAL THEORIES
The following series of hypotheses on the aetiology of this lesion were preceded by earlier observations by Rosenquist and colleagues10 and Somerville and associates,11 who concluded that fixed subaortic stenosis is a lesion that is acquired because of a flow disturbance in the left ventricular outflow tract.
Turbulence theory
The fact that discrete subaortic stenosis can recur after surgical removal led to the supposition that the lesion occurs as a result of a pathological process that was left unaltered by the surgery. An echocardiographic study by Gewillig and colleagues in 199212 showed that abnormal flow patterns are present in patients with discrete subaortic stenosis and that chronic flow disturbances are the cause of the development of the stenosis and its recurrence. Causes of chronic flow disturbances that may stimulate the endothelium to undergo transformation are mainly anatomical. They are as follows:
apically situated muscular ventricular bands that reach the outflow tract, causing disturbance of flow in the subaortic area
a septal ridge, which is an offshoot of a muscular band situated more apically in the outflow tract, causing turbulence that reaches the subaortic region
malalignment of the interventricular septum, resulting in protrusion of the septum into the left ventricular outflow tract, so causing flow disturbances
a long left ventricular outflow tract associated with increased mitral–aortic separation, resulting in an enhanced flow disturbance in the left ventricular outflow tract.
Geometric theory
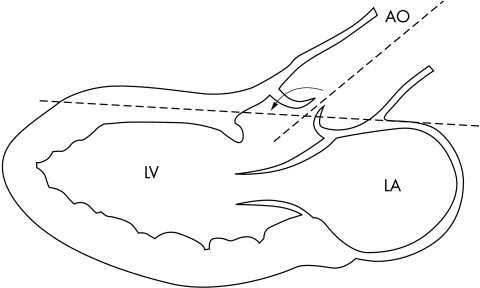
In 1987, Zielinsky and colleagues found that most patients who developed subaortic stenosis had a malaligned VSD with anterior deviation of the infundibular septum,13 while Rosenquist and associates showed a twofold increase in mitral–aortic separation compared with normal hearts.10 In 1993, Kleinert and Geva confirmed the above findings but also showed that there was exaggerated aortic override in patients with subaortic stenosis and an intact interventricular septum.14 An aortoseptal angle (defined as the angle formed by the long axis of the ascending aorta and the plane of the ventricular septum) of < 130° was a prominent feature in their group of patients with subaortic stenosis (fig 1). The steeper angle results in a flow disturbance in the left ventricular outflow tract. The turbulent flow produced by the angle may induce an abnormal proliferative response at the site of high shear stress. The presence of a VSD will add to the increased shear stresses produced by an acute aortoseptal angle. Subsequent investigators have also demonstrated a steepened aortoseptal angle in association with discrete subaortic stenosis, with and without a VSD.15
Figure 1.
An illustration of the long axis of the heart showing the aortoseptal angle between the long axis of the aortic root and the proximal ascending aorta and the midline of the interventricular septum. An angle of < 130° is thought to contribute to increased turbulence in the subaortic area, resulting in the development of a subaortic ridge. Drawing reproduced from Kleinart and Geva14 with permission.
Mechanical stress and genetics theory
More recent data from Cape and colleagues16 highlight the effects of mechanical stress on endothelial cells and the later development of fixed subaortic stenosis. Mechanical stresses alter the structural and functional properties of cells by mechanotransduction. The stresses are converted to electrophysiological and biochemical responses in the sensing cells, and this is followed by adaptation of the cells to external forces by altered gene expression.17
A four stage aetiology for the development and progression of discrete subaortic stenosis has been proposed, based on Cape's hypothesis.16 The procession of events begins with an underlying morphological abnormality, such as a steep aortoseptal angle, which is associated with a genetic predisposition and results in cellular proliferation when exposed to altered septal shear stresses. A genetic predisposition to the development of subaortic stenosis has been documented in Newfoundland dogs,18 while a familial occurrence of subaortic stenosis has been reported in humans.19,20 Other evidence for cellular proliferation related to abnormal shear stresses has been obtained in studies of atherogenesis,21 where obstruction to flow has been shown to develop after exposure to abnormal stresses in subjects with a predisposition to circulatory vascular disease.
UNUSUAL ASSOCIATIONS WITH DISCRETE SUBAORTIC STENOSIS
Bilateral fibrous ridges have been noted in patients with a doubly committed VSD. Turbulence is maximal in the area of the subpulmonary and subaortic ridges, and the histopathological similarities suggest a common mechanism for the development of fibrous ridges in patients with this type of VSD.22 The increased flow across the left ventricular outflow tract in patients with a patent arterial duct23 may be the stimulant for membrane development, while the haemodynamic changes accompanying pulmonary artery banding24 have been implicated in the development of subaortic stenosis related to a secondary leftward shift of the conal septum. A further intriguing association is the trilogy of double chambered right ventricle with subaortic narrowing. The severity or progression of the subpulmonary obstruction and any relation to the severity of subaortic narrowing is unclear.25
CONCLUSIONS
The pathophysiology of discrete, fixed subaortic stenosis is now closer to being understood. The definitive answer may evolve with further cellular biological research. Studies on endothelial and other growth factors may eventually provide the means of preventing and treating this intriguing heart lesion.
REFERENCES
- 1.Vogt J, Dische R, Rupprath G, et al. Fixed subaortic stenosis: an acquired secondary obstruction? A twenty-seven year experience with 168 patients. Thorac Cardiovasc Surg 1989;37:199–206. [DOI] [PubMed] [Google Scholar]
- 2.Choi JY, Sullivan JD. Fixed subaortic stenosis: anatomical spectrum and nature of progression. Br Heart J 1991;65:280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leichter DA, Sullivan I, Gersony WM. “Acquired” discrete subvalvular aortic stenosis: natural history and hemodynamics. J Am Coll Cardiol 1989;14:1539–44. [DOI] [PubMed] [Google Scholar]
- 4.Somerville J. Fixed subaortic stenosis – a frequently misunderstood lesion. Int J Cardiol 1985;8:145–8. [Google Scholar]
- 5.Son JAM, Hoffman D, Puga FJ, et al. Surgery for membranous subaortic stenosis. Eur J Cardiothorac Surg 1994;8:110–12. [DOI] [PubMed] [Google Scholar]
- 6.Katz NM, Buckley MJ, Liberthson RR. Discrete membranous subaortic stenosis: report of 31 patients, review of the literature, and delineation of management. Circulation 1977;56:1034–8. [DOI] [PubMed] [Google Scholar]
- 7.Latson LA. Fibromuscular subvalvular aortic stenosis. In: Garson A, Bricker JT, McNamara GD, eds. The science and practice of pediatric cardiology. Philadelphia: Lea and Febiger,1990:1346–52.
- 8.Reis RL, Peterson LM, Mason DT, et al. Congenital fixed subvalvular aortic stenosis. An anatomical classification and correlations with operative results. Circulation 1971;33/34(suppl 1):11–18. [DOI] [PubMed] [Google Scholar]
- 9.Kitchiner D, Jackson M, Malaiya N, et al. Morphology of left ventricular outflow tract structures in patients with subaortic stenosis and a ventricular septal defect. Br Heart J 1994;72:251–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenquist GC, Clark EB, McAllister HA, et al. Increased mitral aortic separation in discrete subaortic stenosis. Circulation 1979;60:70–4. [DOI] [PubMed] [Google Scholar]
- 11.Somerville J, Stone S, Ross D. Fate of patients with fixed subaortic stenosis after surgical removal. Br Heart J 1980;43:629–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gewillig M, Daenen W, Dumoulin M, et al. Rheologic genesis of discrete subvalvular aortic stenosis: a Doppler echocardiographic study. J Am Coll Cardiol 1992;19:818–24. [DOI] [PubMed] [Google Scholar]
- 13.Zielinsky P, Rossi M, Haertel JC, et al. Subaortic fibrous ridge and ventricular septal defect: the role of septal malalignment. Circulation 1987;75:1124–9. [DOI] [PubMed] [Google Scholar]
- 14.Kleinert S, Geva T. Echocardiographic morphometry and geometry of the left ventricular outflow tract in fixed subaortic stenosis. J Am Coll Cardiol 1993;22:1501–8. [DOI] [PubMed] [Google Scholar]
- 15.Sigfusson G, Tacy T, Vanauker MD, et al. Abnormalities of the left ventricular outflow tract associated with discrete subaortic stenosis in children: an echocardiographic study. J Am Coll Cardiol 1997;30:255–9. [DOI] [PubMed] [Google Scholar]
- 16.Cape EG, Vanauker MD, Gunnlaugur S, et al. Potential role of mechanical stress in the etiology of pediatric heart disease. J Am Coll Cardiol 1997;30:247–54. [DOI] [PubMed] [Google Scholar]
- 17.Davies PF, Tripathi SC. Mechanical stress mechanisms and the cell: an endothelial paradigm. Circ Res 1993;72:239–45. [DOI] [PubMed] [Google Scholar]
- 18.Pyle RL, Patterson DF, Chacko S. The genetics and pathology of discrete subaortic stenosis in the Newfoundland dog. Am Heart J 1976;92:324–34. [DOI] [PubMed] [Google Scholar]
- 19.Gale AW, Cartmill TB, Bernstein L. Familial subaortic stenosis. N Z Med J 1974;4:576–81. [DOI] [PubMed] [Google Scholar]
- 20.Abdallah H, O'Riordan AC, Davidson A, et al. Familial occurrence of discrete subaortic membrane. Pediatr Cardiol 1994;15:198–200. [DOI] [PubMed] [Google Scholar]
- 21.Friedman MH, Bargeron CB, Hutchins GM, et al. Haemodynamic measurements in human arterial casts, and their correlation with histology and luminal area. J Biomech Eng 1980;102:247–51. [DOI] [PubMed] [Google Scholar]
- 22.Ozkutlu S, Saraçlar M, Alehan D, et al. Subpulmonary and subaortic ridges in doubly committed subarterial ventricular septal defect: an echocardiographic study. Eur Heart J 1996;17:935–9. [DOI] [PubMed] [Google Scholar]
- 23.Steinherz L, Ehlers KH, Levin AR, et al. Membranous subaortic stenosis and patent ductus arteriosus. Chest 1977;72:333–8. [DOI] [PubMed] [Google Scholar]
- 24.Freed MD, Rosenthal A, Plauth WH, et al. Development of subaortic stenosis after pulmonary artery banding. Circulation 1973;48(suppl 3):P3–10. [DOI] [PubMed] [Google Scholar]
- 25.Ward CJB, Culham JAG, Patterson MWH, et al. The trilogy of double-chambered right ventricle, perimembranous ventricular septal defect and subaortic narrowing – a more common association than previously recognized. Cardiol Young 1995;5:140–6. [Google Scholar]