Abstract
Objective: To evaluate whether measurements of N-terminal pro-brain natriuretic peptide (NT-proBNP) can be used to differentiate patients with normal and reduced left ventricular ejection fraction (LVEF) in an unselected consecutive group of hospital inpatients.
Setting: City general hospital, Copenhagen, Denmark.
Patients and design: During a 10 month period 2230 admissions to a city general hospital (80% of targeted patients) had an echocardiographic evaluation of left ventricular function, a comprehensive clinical evaluation, and blood analysis of N-terminal-pro-brain natriuretic peptide (NT-proBNP) within 24 hours of admission. Exclusions resulted from lack of informed consent or failure to obtain the required evaluations before death or discharge from hospital. Echocardiography was unsatisfactory in 37 patients, so the final number studied was 2193.
Results: A raised NT-proBNP (≥ 357 pmol/l) identified patients with an LVEF of ≤ 40% (n = 157) with a sensitivity of 73% and a specificity of 82%. The negative predictive value of having an NT-proBNP concentration below 357 pmol/l was 98%. Concentrations of NT-proBNP increased with increasing age and with decreasing LVEF (p < 0.05). A predicted concentration of NT-proBNP (corrected for age, sex, and serum creatinine) was determined for each patient. In patients with an NT-proBNP value less than predicted, the probability of having an LVEF of > 40% was more than 97%. This probability rapidly decreased to 70% as the measured NT-proBNP increased to 150% of the predicted value.
Conclusions: A single measurement of NT-proBNP at the time of hospital admission provides important information about LVEF in unselected patients.
Keywords: natriuretic peptides, N-terminal proBNP, systolic dysfunction
Chronic heart failure is a clinical syndrome that primarily affects elderly people. The syndrome is associated with high morbidity and mortality and is often attributable to left ventricular systolic dysfunction.1,2 On the basis of previous reports, as many as 50% of patients with a reduced left ventricular ejection fraction (LVEF) do not have clinical symptoms related to chronic heart failure.3 These patients may remain asymptomatic for years and when symptoms or clinical signs appear, they are often non-specific and the syndrome may be misdiagnosed.
Clinical trials have shown that angiotensin converting enzyme (ACE) inhibitors, spironolactone, and some β blockers significantly reduce mortality and morbidity in patients with systolic chronic heart failure.4–7 Thus an early and reliable diagnosis of left ventricular systolic dysfunction is important for these patients. Because of their costs and limited availability, echocardiography and radionucleotide ventriculography are not suitable as primary diagnostic screening tools, and new cost–effective diagnostic tools are needed. In this respect, neurohormonal markers could be useful in the diagnosis of left ventricular dysfunction.3,8,9
Natriuretic peptides are produced primarily within the heart and released into the circulation in response to increased wall tension.10 Brain natriuretic peptide (BNP), in contrast to atrial natriuretic peptide (ANP), is not only secreted from the atria but also from the ventricles, especially in patients with heart failure.11 Circulating concentrations of several cardiac natriuretic peptides—including ANP, BNP, and their N-terminal pro-hormones (N-terminal pro-atrial natriuretic peptide (NT-proANP) and N-terminal pro-brain natriuretic peptide (NT-proBNP))—are raised in both symptomatic and asymptomatic patients with left ventricular dysfunction.8,9,12 Recent smaller studies suggest that BNP and NT-proBNP may be superior to ANP and NT-proANP in the detection of left ventricular dysfunction.12,13 Recently a reliable and less time consuming enzyme linked immunosorbent assay (ELISA) method for the analysis of NT-proBNP has been developed and NT-proBNP may therefore be a suitable peptide for a diagnostic assay.14
In the present study we investigated the role of NT-proBNP as a screening tool for the identification of patients with normal and reduced left ventricular systolic dysfunction in an unselected group of consecutive patients at the time of admission to a community hospital.
METHODS
Patients and study design
Between 1 April 1998 and 31 March 1999 all patients above the age of 40 years admitted to a general city hospital in the Copenhagen area (Amager Hospital) were invited to participate in the study. Among 3644 patients admitted, 3236 (89%) gave their written informed consent, while 408 (11%) were excluded for the following reasons: discharge before echocardiography could be done (n = 155); death before inclusion (n = 56); mental or physical status not allowing written informed consent (n=68); and lack of informed consent (n = 129). Physicians in the ward were blinded to the results of the study procedures and laboratory test results. However, for ethical reasons echocardiographic findings from 13 patients were reported to the physician in the ward (seven major pericardial effusions and six severe valvar conditions).
During the last 10 months of the study, blood samples were drawn for the analysis of NT-proBNP from 2230 patients (80% of the patients included in this period). Among these patients, echocardiographic measurements of left ventricular ejection fraction were unsatisfactory in 37, leaving 2193 patients to be included in the study.
The study was formally approved by the regional ethics committee of the city of Copenhagen.
Medical history
Within 24 hours of admission all patients underwent a structured comprehensive clinical examination including heart and lung auscultation. A structured medical history was taken with specific focus on heart related symptoms (orthopnoea, dyspnoea when walking or climbing stairs, oedema of the legs, fatigue or weight loss in response to diuretic treatment), including known ischaemic heart disease, hypertension, chronic lung disease, liver disease, and diabetes. In addition, information about smoking habits, alcohol consumption, and drug treatment was recorded. The medical history was obtained (by MB and VK) without knowledge of the results of LVEF and NT-proBNP. After discharge, the hospital records were evaluated and the final clinical diagnosis, routine laboratory results, and drug treatment at time of discharge were recorded.
Symptoms or clinical signs of heart failure
Symptoms or signs of chronic heart failure were considered to be present if a patient had at least one of the following features: orthopnoea; dyspnoea when walking at a regular pace; peripheral fluid retention; weight loss because of treatment with diuretics; auscultatory rales; or neck vein distension.
Echocardiography
Echocardiography was done within 24 hours of admission by one of the two investigators (MB or VK) using a Hewlett Packard Imagepoint, model M2410A (Andover, Massachusetts, USA). LVEF was estimated according to Teichholz and colleagues in all subjects with a homogeneous contraction pattern.15 Where there was a heterogeneous contraction pattern, LVEF was estimated from the wall motion index.16 A reduced LVEF was defined as a value of 40% or less. Interobserver variation in the evaluation of LVEF was 4% (r = 0.95; n = 12).
Analysis of NT-proBNP
Blood samples were drawn between 8.00 am and 10.00 am within 24 hours of admission. Samples were collected in prechilled tubes containing EDTA, immediately placed on ice, and promptly centrifuged at 4°C. After separation, plasma was stored at −80°C. NT-proBNP measurements were done using an ELISA—a two step sandwich assay with streptavidin coated microtitre plates.14 This assay does not require sample extraction and there is no detectable cross reactivity with ANP, NT-proANP, BNP, or urodilatin. The interassay and intra-assay variances were 10% and 3%, and recovery was between 104% and 112%. In patients with an LVEF of > 50%, 85% of subjects had an NT-proBNP value below 357 pmol/l (1n(357) = 5.9). This value was used as the upper normal limit in the analyses of sensitivity and specificity. It should be stressed that 357 pmol/l is not a true normal value but a cut off value derived from the present hospital inpatient population.
Statistics
For normally distributed variables, values are expressed as mean (SD). All statistical analyses were done using statistical analysis software (SAS version 6.12 ; S−+ version 3.3). Other continuous variables are given as median and range. Differences in means between groups were compared using a t test or an F test as appropriate, and differences in medians by the Mann–Whitney U test. Differences in proportions were compared with a χ2 test.
Assessing the effect of predictors of LVEF was feasible using a multivariate logistic regression model. LVEF was chosen as the dependent variable, while the set of predictors were age, sex, 1n(NT-proBNP), and serum creatinine. The log linearity of age, 1n(NT-proBNP), and serum creatinine on the odds ratio, and their interaction, was investigated using generalised additive models.17 In addition, all lower order interactions were investigated. For other types of clinical information the diagnostic value of NT-proBNP was assessed by modelling the probability of reduced LVEF using a logistic regression model.
The measure “per cent of predicted NT-proBNP” was constructed by regressing 1n(NT-proBNP) on the predictors age, sex, and serum creatinine using general linear models. The ability of this measure to predict an LVEF of ≤ 40% was assessed using a logistic regression model. Probability values of p < 0.05 were considered significant.
RESULTS
Patients
The 2193 patients included represent 2193 admissions; 2061 (94%) were acute admissions and 132 (6%) were planned. The patients were allocated to different hospital wards: coronary care unit (17%), internal medicine (54%), orthopaedics (14%), and general surgery (15%). At the time of admission, 35% of all patients were being treated with diuretics and 10% were receiving either ACE inhibitors or angiotensin II antagonists. Baseline characteristics of the patients are shown in table 1.
Table 1.
Baseline characteristics of the patients
| All patients (n=2193) | LVEF ≤40% (n=157) | LVEF >40%, ≤50% (n=244) | LVEF >50% (n=1792) | |
| Age (years) (median (range)) | 73 (40–104) | 77 (41–97) | 77 (41–95) | 72* (40–104) |
| Sex (male) | 41 | 57 | 52 | 38* |
| History of hypertension | 26 | 32 | 31 | 24 |
| History of IHD | 23 | 56 | 39* | 18* |
| History of lung disease | 19 | 24 | 18 | 19 |
| Smoker | 42 | 35 | 37 | 44* |
| Diabetes | 12 | 17 | 15 | 11 |
| Any symptoms or signs of CHF | 43 | 74 | 53* | 39* |
| NT-proBNP (median) (pmol/l) (range) | 110 (0–12464) | 860 (21–12464) | 280* (5–7637) | 81* (0–5903) |
Values are % unless indicated.
*p < 0.05 v the group of patients with an LVEF of ≤ 40%.
CHF, chronic heart failure; IHD, ischaemic heart disease; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal pro-brain natriuretic peptide.
Echocardiography
Measurements of LVEF were normal distributed, with a mean (SD) value of 59 (11)%. One hundred and fifty seven patients (7%) had an LVEF of ≤ 40% and 26% of these patients had no symptoms or signs of congestive heart failure. Patients with an LVEF of ≤ 40% were more often male, on average six years older, and had a higher prevalence of ischaemic heart disease compared with patients with an LVEF of > 50%. In addition, the median value of NT-proBNP was significantly higher in patients with an LVEF of ≤ 40% than in patients with a normal LVEF (> 50%) and patients with an LVEF of between 40–50%.
Single measurement of NT-proBNP as a predictor of reduced LVEF
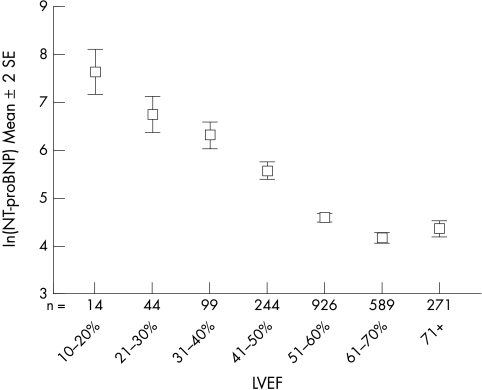
Logarithmic (1n) transformation of NT-proBNP values resulted in a dataset with a normal distribution. The median value of NT-proBNP was 110 pmol/l (1n 110 = 4.7). The relation between LVEF and 1n(NT-proBNP) is shown in fig 1. We found that 1n(NT-proBNP) was inversely related to LVEF. Table 2 shows the diagnostic value of a single measurement of NT-proBNP for the detection of an LVEF of ≤ 40%, when applied to the whole study population and to patients with any symptoms or signs of congestive heart failure. When applied to the whole study population, NT-proBNP alone (cut off value 357 pmol/l) showed a sensitivity of 73%, a specificity of 82%, a positive predictive value of 24%, and a negative predictive value of 98%. Similar findings were obtained in the subgroup with symptoms or signs of congestive heart failure.
Figure 1.
Error bars illustrating the correlation between left ventricular ejection fraction (LVEF) and the mean value of 1n(NT-proBNP). 1n(55 pmol/l) = 4; 1n(2981 pmol/l) = 8. NT-proBNP, N-terminal pro-brain natriuretic peptide.
Table 2.
Diagnostic value of NT-proBNP for the detection of a left ventricular ejection fraction of ≤ 40%
| All patients (n=2193) | Any symptoms or signs of CHF (n=928) | |
| Sensitivity | 73% | 78% |
| Specificity | 82% | 76% |
| Positive predictive value | 24% | 30% |
| Negative predictive value | 98% | 96% |
| AUC* | 0.85 | 0.84 |
| Prevalence of LVEF ≤40% | 7% | 12% |
The cut off value for NT-proBNP was defined as the 85th centile of subjects with an LVEF of > 50% (357 pmol/l).
*Area under the curve in a receiver operating characteristic curve.
CHF, chronic heart failure; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal pro-brain natriuretic peptide.
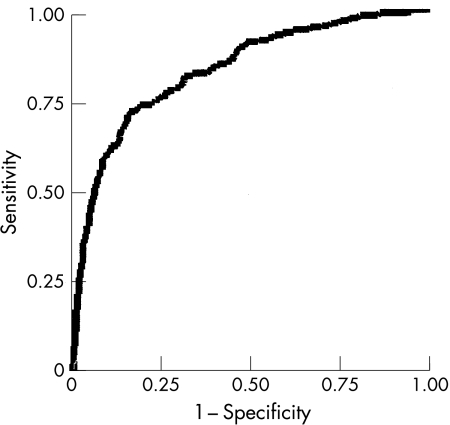
A receiver operating characteristic (ROC) curve was created to assess the sensitivity and specificity of NT-proBNP to detect an LVEF of ≤ 40% (fig 2). The diagnostic value of a single NT-proBNP value without other information about the patient is reflected in an area under the ROC curve of 0.85. A severely reduced ejection fraction (≤ 30%) was present in 58 patients (3%), and the diagnostic value of NT-proBNP in this population was even higher, with an area under the ROC curve of 0.89 (data not shown).
Figure 2.
Receiver operating characteristic (ROC) curve showing the ability of N-terminal pro-brain natriuretic peptide (NT-proBNP) to identify patients with a left ventricular ejection fraction (LVEF) of ≤ 40%.
Relations between clinical variables, NT-proBNP, and LVEF
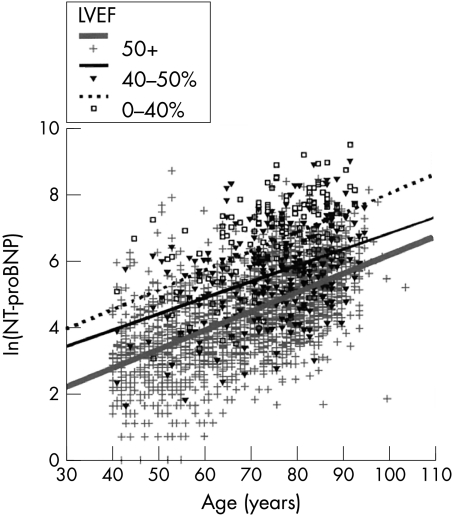
In the total population, the plasma concentrations of NT-proBNP were found to increase with increasing age. Furthermore, when subdividing patients into three groups according to LVEF (0–40%, 40–50%, 50%+) three separate regression lines could be identified (fig 3). When we excluded all patients with abnormal echocardiographic findings (LVEF < 50%, hypertrophy, enlarged chamber dimensions, or valve diseases) and a raised serum creatinine, the concentration of NT-proBNP still correlated with age (data not shown).
Figure 3.
Scatter plot showing the correlation between age and 1n(NT-proBNP). Patients are divided into three categories according to left ventricular ejection fraction (LVEF); LVEF ≤ 40%, LVEF > 40% but < 50%, and LVEF of 50% or above. The three lines identified according to LVEF values were significantly different (p < 0.001), but not their slopes. 1n(7 pmol/l) = 2; 1n(8103 pmol/l) = 9. NT-proBNP, N-terminal pro-brain natriuretic peptide.
The relations between NT-proBNP, age, sex, serum creatinine, and LVEF were examined in a multivariate regression analysis. In the resulting model the combination of age and NT-proBNP was of major importance for predicting an LVEF of ≤ 40%, while sex and serum creatinine had only a minor impact.
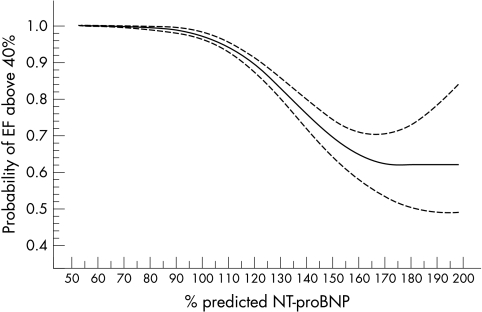
Prediction of LVEF based upon NT-proBNP and clinical variables
Accounting for sex, age, a history of myocardial infarction, angina pectoris, and hypertension, the concentration of NT-proBNP showed a strong and significant (p < 0.001) diagnostic value in predicting a low LVEF. Thus the usefulness of NT-proBNP as a screening tool is clearly greater than the clinical information gained from the patient’s history. Based on information about age, sex, and serum creatinine it was possible to determine a predicted NT-proBNP value for each patient. This value represents the mean NT-proBNP for any given age, taking sex and serum creatinine into account. Thus every patient had a predicted as well as an actually measured value of NT-proBNP. The difference between these two values can be given as a percentage of the predicted value (as with lung function indices). In fig 4, the predicted NT-proBNP is set at 100%. The figure illustrates the probability of having an LVEF of > 40% as a function of percentage of predicted NT-proBNP. For NT-proBNP values less than 100% of the predicted value, the probability of having an LVEF of > 40% is more than 97%. Having an NT-proBNP value of 150% of the predicted value is associated with only a 70% chance of having an LVEF of > 40%.
Figure 4.
Probability of having an ejection fraction (EF) above 40% as a function of percentage of predicted N-terminal pro-brain natriuretic peptide (NT-proBNP). Predicted NT-proBNP is based on sex, age, and serum creatinine measurements (95% confidence intervals are shown).
DISCUSSION
The main findings of this study are that the concentrations of NT-proBNP increase with increasing age and that NT-proBNP increases with decreasing LVEF. In addition, the negative predictive value of having a “normal” value of NT-proBNP is very high (98%) and NT-proBNP therefore seems to be a valuable tool for excluding a decreased LVEF at the time of admission to hospital.
Previous studies have shown that concentrations of several natriuretic peptides are increased when left ventricular systolic function is impaired. There is now increasing evidence that these peptides may be useful in diagnosing systolic dysfunction and as prognostic markers. In general, BNP is considered superior to ANP and its prohormone as a marker of systolic dysfunction and decreased LVEF.9,13,18–20 Within the BNP group, NT-proBNP more accurately separates patients with normal and impaired LVEF than BNP.12,21 However, because NT-proBNP most probably reflects myocardial wall tension it should be borne in mind that it probably also identifies other cardiac pathologies characterised by increased wall stress in addition to a reduced LVEF.
Identification of left ventricular systolic function
This is the first study to investigate the diagnostic value of NT-proBNP at the time of admission in a broad group of consecutive hospital inpatients. Ninety four per cent of the admissions were acute and the prevalence of a low LVEF (≤ 40%) was 7%, with symptoms or findings compatible with heart failure occurring in 75% of these patients. For the identification of an LVEF of ≤ 40% in the total population, NT-proBNP had a negative predictive value of 98% and an area under the ROC curve of 0.85. NT-proBNP had similar values for the identification of an LVEF of ≤ 40% in the subgroup of patients with signs or symptoms of heart failure. This finding is compatible with recent data from Dao and colleagues,22 who reported that measurements of BNP were able to identify heart failure with a sensitivity and negative predictive value of 98% in a smaller group of patients with shortness of breath treated in an urgent care setting. In less acute settings, both BNP and ANP have also been found to be of diagnostic value among patients referred to heart failure clinics.8,23 There are no previous studies of NT-proBNP in unselected groups of patients, but in a random sample from family physicians’ lists in Glasgow, McDonagh and colleagues showed that the overall diagnostic accuracy of BNP in detecting an LVEF of ≤ 30% corresponded to an area under the curve (AUC) of 0.88 (sensitivity 77%, specificity 87%).9 The prevalence of LVEF values of ≤ 30% in the present population was 3.0%, and NT-proBNP identified this group of patients with a similar diagnostic accuracy (AUC = 0.89; sensitivity 90%, specificity 73%). In patients referred to echocardiography, NT-proBNP has also been found to be of value in detecting patients with a decreased LVEF.24
BNP concentrations seem to fall after treatment with loop diuretics and ACE inhibitors, probably reflecting a reduction in left ventricular filling pressure.25,26 On the other hand, many of our patients with systolic dysfunction (LVEF ≤ 40%) were already receiving diuretics (62%) and ACE inhibitors/angiotensin II antagonists (27%) at the time of admission. Despite this, the relation between LVEF and concentrations of NT-proBNP was preserved and the diagnostic value of a single NT-proBNP measurement was comparable with the results of a previous community based study.9
NT-proBNP and age
The correlation that we found between increasing age and increasing concentrations of NT-proBNP has not been properly established in previous studies, although Campbell and colleagues described an age correlation in 33 healthy women.27 Hunt and associates found a significant correlation between age and concentrations of both BNP and NT-proBNP among patients with an LVEF of ≤ 45%, but when including creatinine in a multivariate model the age factor was excluded.12 In the present study, serum creatinine did add significant information in the prediction of a reduced LVEF. Most previous studies investigating natriuretic peptides have excluded patients over the age of 75 years or have only investigated old patients in a narrow age span, thereby potentially missing a correlation with age.28,29 Although the reason for the age related increase in NT-proBNP is unknown, the finding is important to consider when defining cut off values for NT-proBNP. Thus an NT-proBNP concentration that equals the mean value of patients aged 70 years should be considered raised when found in a blood sample from a 40 year old patient.
NT-proBNP in the clinical setting
Our results show that a single measurement of NT-proBNP provides important information about LVEF. An association between values of NT-proBNP and age was found, whereas sex and serum creatinine concentrations did not affect the NT-proBNP values. In analogy to the measurements used in lung physiology (that is, per cent of predicted lung function), the percentage of predicted NT-proBNP can be used to identify patients with an increased risk of having a reduced LVEF. When using percentage of predicted NT-proBNP, there was a steep and significant fall in the probability of a patient having an LVEF of > 40% when the actual NT-proBNP measurement exceeded the predicted value.
Conclusions
This appears to be the first study to show a clear age related increase in NT-proBNP concentrations. Concentrations of NT-proBNP increased with increasing age across three different intervals of LVEF. Furthermore, the results suggest that a patient with a measured value of NT-proBNP below that predicted (after correction for age, sex, and serum creatinine corrected) has a 97% certainty of having an LVEF of > 40%. We conclude that a single measurement of NT-proBNP at the time of admission to hospital can provide important information about LVEF in unselected patients.
Acknowledgments
This study was supported by unrestricted research grants from Astra-Zeneca (Copenhagen, Denmark), Roche (Basel, Switzerland), and The Danish Heart Foundation (Copenhagen, Denmark).
Abbreviations
ACE, angiotensin converting enzyme
ANP, atrial natriuretic peptide
AUC, area under the curve
BNP, brain natriuretic peptide
ELISA, enzyme linked immunosorbent assay
LVEF, left ventricular ejection fraction
NT-proANP, N-terminal pro-atrial natriuretic peptide
NT-proBNP, N-terminal pro-brain natriuretic peptide
REFERENCES
- 1.McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: the Framingham study. N Engl J Med 1971;285:1441–6. [DOI] [PubMed] [Google Scholar]
- 2.The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293–302. [DOI] [PubMed] [Google Scholar]
- 3.McDonagh TA, Morrison CE, Lawrence A, et al. Symptomatic and asymptomatic left-ventricular systolic dysfunction in an urban population. Lancet 1997;350:829–33. [DOI] [PubMed] [Google Scholar]
- 4.The CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the cooperative North Scandinavian enalapril survival study (CONSENSUS). N Engl J Med 1987;316:1429–35. [DOI] [PubMed] [Google Scholar]
- 5.MERIT-HF Trial Study Group. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 1999;353:2001–7. [PubMed] [Google Scholar]
- 6.Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. US carvedilol heart failure study group. N Engl J Med 1996;334:1349–55. [DOI] [PubMed] [Google Scholar]
- 7.Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med 1999;341:709–17. [DOI] [PubMed] [Google Scholar]
- 8.Cowie MR, Struthers AD, Wood DA, et al. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet 1997;350:1349–53. [DOI] [PubMed] [Google Scholar]
- 9.McDonagh TA, Robb SD, Murdoch DR, et al. Biochemical detection of left-ventricular systolic dysfunction. Lancet 1998;351:9–13. [DOI] [PubMed] [Google Scholar]
- 10.Kinnunen P, Vuolteenaho O, Ruskoaho H. Mechanisms of atrial and brain natriuretic peptide release from rat ventricular myocardium: effect of stretching. Endocrinology 1993;132:1961–70. [DOI] [PubMed] [Google Scholar]
- 11.Yasue H, Yoshimura M, Sumida H, et al. Localization and mechanism of secretion of B-type natriuretic peptide in comparison with those of A-type natriuretic peptide in normal subjects and patients with heart failure. Circulation 1994;90:195–203. [DOI] [PubMed] [Google Scholar]
- 12.Hunt PJ, Richards AM, Nicholls MG, et al. Immunoreactive amino-terminal pro-brain natriuretic peptide (NT-PROBNP): a new marker of cardiac impairment. Clin Endocrinol (Oxf) 1997;47:287–96. [DOI] [PubMed] [Google Scholar]
- 13.Yamamoto K, Burnett JC, Jougasaki M, et al. Superiority of brain natriuretic peptide as a hormonal marker of ventricular systolic and diastolic dysfunction and ventricular hypertrophy. Hypertension 1996;28:988–94. [DOI] [PubMed] [Google Scholar]
- 14.Karl J, Borgya A, Gallusser A, et al. Development of a novel, N-terminal-proBNP (NT-proBNP) assay with a low detection limit. Scand J Clin Lab Invest Suppl 1999;230:177–81. [PubMed] [Google Scholar]
- 15.Teichholz LE, Kreulen T, Herman MV, et al. Problems in echocardiographic volume determinations: echocardiographic-angiographic correlations in the presence of absence of asynergy. Am J Cardiol 1976;37:7–11. [DOI] [PubMed] [Google Scholar]
- 16.Berning J, Rokkedal NJ, Launbjerg J, et al. Rapid estimation of left ventricular ejection fraction in acute myocardial infarction by echocardiographic wall motion analysis. Cardiology 1992;80:257–66. [DOI] [PubMed] [Google Scholar]
- 17.Hastie T, Tibshirani RJ. Generalized additive models. London: Chapman and Hall, 1990.
- 18.Choy AM, Darbar D, Lang CC, et al. Detection of left ventricular dysfunction after acute myocardial infarction: comparison of clinical, echocardiographic, and neurohormonal methods. Br Heart J 1994;72:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davidson NC, Naas AA, Hanson JK, et al. Comparison of atrial natriuretic peptide B-type natriuretic peptide, and N-terminal proatrial natriuretic peptide as indicators of left ventricular systolic dysfunction. Am J Cardiol 1996;77:828–31. [DOI] [PubMed] [Google Scholar]
- 20.Omland T, Aakvaag A, Bonarjee VV, et al. Plasma brain natriuretic peptide as an indicator of left ventricular systolic function and long-term survival after acute myocardial infarction. Comparison with plasma atrial natriuretic peptide and N-terminal proatrial natriuretic peptide. Circulation 1996;93:1963–9. [DOI] [PubMed] [Google Scholar]
- 21.Richards AM, Nicholls MG, Yandle TG, et al. Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin: new neurohormonal predictors of left ventricular function and prognosis after myocardial infarction. Circulation 1998;97:1921–9. [DOI] [PubMed] [Google Scholar]
- 22.Dao Q, Krishnaswamy P, Kazanegra R, et al. Utility of B-type natriuretic peptide in the diagnosis of congestive heart failure in an urgent-care setting. J Am Coll Cardiol 2001;37:379–85. [DOI] [PubMed] [Google Scholar]
- 23.Bettencourt P, Ferreira A, Dias P, et al. Evaluation of brain natriuretic peptide in the diagnosis of heart failure. Cardiology 2000;93:19–25. [DOI] [PubMed] [Google Scholar]
- 24.Talwar S, Squire IB, Davies JE, et al. Plasma N-terminal pro-brain natriuretic peptide and the ECG in the assessment of left-ventricular systolic dysfunction in a high risk population. Eur Heart J 1999;20:1736–44. [DOI] [PubMed] [Google Scholar]
- 25.Richards AM, Crozier IG, Yandle TG, et al. Brain natriuretic factor: regional plasma concentrations and correlations with haemodynamic state in cardiac disease. Br Heart J 1993;69:414–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Troughton RW, Frampton CM, Yandle TG, et al. Treatment of heart failure guided by plasma aminoterminal brain natriuretic peptide (N-BNP) concentrations. Lancet 2000;355:1126–30. [DOI] [PubMed] [Google Scholar]
- 27.Campbell DJ, Mitchelhill KI, Schlicht SM, et al. Plasma amino-terminal pro-brain natriuretic peptide: a novel approach to the diagnosis of cardiac dysfunction. J Card Fail 2000;6:130–9. [PubMed] [Google Scholar]
- 28.Arad M, Elazar E, Shotan A, et al. Brain and atrial natriuretic peptides in patients with ischemic heart disease with and without heart failure. Cardiology 1996;87:12–17. [DOI] [PubMed] [Google Scholar]
- 29.Wallen T, Landahl S, Hedner T, et al. Brain natriuretic peptide predicts mortality in the elderly. Heart 1997;77:264–7. [DOI] [PMC free article] [PubMed] [Google Scholar]