Temporary transvenous cardiac pacing is occasionally required for prolonged periods, particularly in patients with severe infection and bradyarrhythmias who may need several weeks of antibiotic treatment before a permanent pacemaker can be safely implanted. Prolonged temporary transvenous pacing is frequently associated with complications such as local or systemic infection, lead displacement, and right ventricular perforation,1,2 that necessitate sequential lead replacement or repositioning, subjecting patients to the risk, inconvenience, and additional cost of multiple invasive procedures. Furthermore, traditional external pulse generators significantly limit patients’ mobility and nursing care. We sought to overcome these problems by evaluating an alternative method for prolonged temporary pacing which (1) involves a single procedure, (2) provides reliable pacing for several weeks with a low risk of complications, and (3) allows patients to ambulate freely during this period.
METHOD
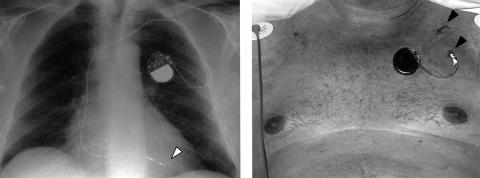
A bipolar active-fixation permanent pacing lead (Medtronic 5068, 58 cm) was introduced via the internal jugular or subclavian vein using a peel-away introducer sheath, and positioned in the right ventricle under fluoroscopic guidance. Pacing parameters were checked with the active-fixation screw deployed. The lead was tunnelled subcutaneously to an exit point approximately 10 cm from the point of vascular access and secured to the skin using the suture sleeve (fig 1). Ventricular pacing was achieved using an external permanent pacing pulse generator, which was attached to the skin of the upper chest using an adhesive dressing. Patients were monitored via telemetry with regular checks of the pacing parameters. After the required period of temporary pacing, the lead was removed at the bedside, without additional fluoroscopy, having retracted the active-fixation mechanism.
Figure 1.
(Left) Chest radiograph showing the position of the bipolar ventricular pacing lead positioned in the right ventricular apex using an active fixation screw (arrow). (Right) The lead was tunnelled subcut- aneously from the point of vascular access (top arrow) to an exit point approximately 10 cm away. The lead was secured to skin using the suture sleeve (bottom arrow) and was connected to an external permanent pacemaker pulse generator. Both lead and generator were covered with an adhesive dressing.
RESULTS
This technique was used for prolonged temporary pacing in 20 patients, median (range) age 65.5 (40–85) years (17 men). All had symptomatic bradyarrhythmias or were pacemaker dependent, but immediate permanent pacing was precluded either because of systemic infection or the likelihood that the bradycardia would resolve. Nine patients had infected permanent pacemakers requiring total system explantation. Non-pacemaker related severe infection in seven patients included endocarditis (2), post cardiac surgery sepsis (3), and septicaemia from other causes (2). Cases without infection included three post-infarction patients (two with complete heart block, one with refractory ventricular tachycardia plus sinus bradycardia) and one with tetanus plus severe autonomic dysfunction. The median procedure time including venous access, measurement of electrical parameters, subcutaneous tunnelling, and securing of the lead was 16 (range 9–28) minutes with a median fluoroscopy time of 3.1 (range 1.8–7.0) minutes. Tunnelled pacing leads remained in situ for a median of 28 (range 9–81) days. During a total pacing duration of 550 patient days, there were no episodes of lead displacement or of pacing failure, nor did any system require revision. In three cases, Hickman vascular access lines were placed at the same time as the pacing lead, through the same venous puncture, but tunnelled to a separate exit site; none of these procedures were associated with any complications. Only two patients developed localised infection at the exit site; neither required additional treatment, nor was there evidence of systemic infection. One patient died from overwhelming infection unrelated to the pacing system. All leads were easily removed without complications.
DISCUSSION
These findings show that insertion of an active-fixation permanent pacing lead through a subcutaneous tunnelled approach allows safe, reliable temporary cardiac pacing over prolonged periods with minimal risk of infection, avoiding the need for multiple replacement/repositioning procedures and the associated hazards. Patient tolerability was excellent, particularly in comparison to traditional semi-rigid temporary pacing leads. The use of anchoring sleeves to secure the lead and a small permanent pulse generator allowed unrestricted patient ambulation, nursing care and physiotherapy, and facilitated transfer of patients for other procedures or investigations without the risk of lead dislodgement. Finally, the need for only a single insertion procedure conserved central venous access sites, and enabled subsequent permanent pacemaker implantation into a site that had not undergone previous instrumentation. The technique itself is straightforward for cardiologists trained in permanent pacemaker implantation. Indeed, we found the active-fixation leads easier to insert and position than traditional semi-rigid temporary pacing catheters, as evidenced by comparatively short fluoroscopy and procedure times. The moderate extra cost of the permanent pacing lead is offset by the reduced requirement for temporary pacing catheters and by avoiding multiple procedures. The pulse generator itself is entirely external and therefore re-usable after routine antisepsis.
Martin and colleagues have described the use of an active-fixation permanent lead for temporary pacing,3 but there are no prior reports on the utility of this approach to achieve temporary pacing over extended periods. Subcutaneous tunnelling is widely used for haemodialysis or other long term vascular access devices, to reduce the risk of bacterial colonisation and infection,4 but has not been previously described with temporary cardiac pacing. Our series demonstrates that a temporary pacing technique using the combination of an active fixation permanent pacing lead and subcutaneous tunnelling is invaluable as a “bridge” to permanent pacing in patients with systemic sepsis who require prolonged antibiotic treatment to eradicate infection before a permanent system can be implanted. This approach may also be beneficial in patients with prolonged, symptomatic bradyarrhythmias that are expected to resolve—for example, after inferior myocardial infarction—thereby avoiding the need for permanent pacing in a significant proportion. In principle, extended dual chamber temporary pacing via tunnelled atrial and ventricular pacing leads should also be feasible, and benefit particularly those patients with bradyarrhythmias and haemodynamic compromise. Given its simplicity and reliability, we believe that development of specific pacemaker leads for prolonged temporary cardiac pacing is justified.
In conclusion, prolonged temporary cardiac pacing using tunnelled active-fixation permanent pacing is a safe, effective, and convenient approach to transvenous cardiac pacing in patients with severe sepsis or other indications to defer permanent pacemaker implantation.
REFERENCES
- 1.Hynes JK, Holmes DR, Harrison CE. Five year experience with temporary pacemaker therapy in the coronary care unit. Mayo Clin Proc 1983;58:122–6. [PubMed] [Google Scholar]
- 2.Winner S, Boon N. Clinical problems with temporary pacemakers prior to permanent pacing. J R Coll Physicians Lond 1989;23:161–3. [PMC free article] [PubMed] [Google Scholar]
- 3.Martin DO, Vergara I, Greenfield RA, et al. Prolonged temporary transvenous pacing using permanent active-fixation leads. Circulation 1999;100(suppl 1):1–786. [Google Scholar]
- 4.Moran KT, McEntee G, Jones B, et al. To tunnel or not to tunnel catheters for parenteral nutrition. Ann R Coll Surg Engl 1987;69:235–6. [PMC free article] [PubMed] [Google Scholar]