Shear induced platelet activation is responsible for arterial thrombosis. The role of fibrinogen is established at low shear stress, but at high shear stress von Willebrand factor (vWF), not fibrinogen, is essential for platelet adhesion and aggregation.1 Patients with vWF deficiency exhibit resistance to thrombosis,2 and raised vWF is a risk factor for acute coronary syndromes. Interpretation of vWF concentrations is, however, complicated since vWF may be an acute phase reactant. The effect of vWF on thrombosis in the normal (non-vWF deficient) population remains unknown. The aim of this study was to determine the effect of coronary occlusion on plasma vWF level in vivo and the effect of raised vWF on thrombosis/haemostasis in vitro.
METHODS
Effect of coronary angioplasty
Eleven patients with single vessel coronary disease and stable angina, undergoing elective angioplasty to the left anterior descending or circumflex artery, were enrolled and 10 000 U of heparin were administered. Balloon inflations (2.5 (0.5) per patient) were followed by stent implantation in eight patients. Blood was drawn from a coronary sinus (CS) catheter immediately before the first balloon inflation and at 1, 5, 10, 15, 20, and 30 minutes, and from the femoral vein before and 30 minutes after the first inflation. Samples were collected into 3.2% citrate for measurement of vWF antigen (vWF:Ag), factor VIII coagulant activity (FVIII:c), and platelet reactivity using the PFA-100 (Dade Behring, Milton Keynes, UK) before, 15–20, and 30 minutes after the first inflation. Plasma vWF:Ag was measured by enzyme linked immunosorbent assay (ELISA) and FVIII:c with the CA-6000 coagulation analyser (Sysmex, Milton Keynes, UK).
The PFA-100 employs citrated whole blood, which is added to two cartridges which contain a collagen coated membrane, one containing adrenaline (epinephrine) (C/Epi) and the other, ADP (C/ADP) as agonist to induce platelet aggregation.3 Platelets are pre-activated by a shear stress of 190 dynes/cm2. The time for blood to occlude the aperture in the membrane (closure time) is recorded.
Effect of vWF on platelet reactivity in vitro
Native haemostasis was assessed using the PFA-100 in 10 healthy volunteers (26–40 years; six men). After one hour, subjects were retested, adding 10.7 μg vWF (Calbiochem, Nottingham, UK) to the blood in each cartridge. vWF:Ag was measured before and after in vitro addition of vWF, on three pairs of blood samples using ELISA.
Results were analysed using paired t tests with Bonferroni‘s correction and simple linear regression.
RESULTS
Effect of angioplasty
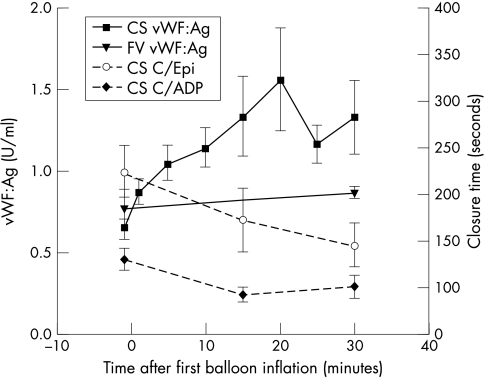
Plasma vWF in the CS rose in response to angioplasty (fig 1). There was no further increase in vWF with subsequent inflations, although a significant rise occurred immediately after stent deployment (0.9 (0.08) U/ml to 1.26 (0.07) U/ml, p = 0.003). There was no rise in vWF in systemic blood. There was a progressive increase in platelet reactivity in the CS as evidenced by a reduction in closure time in C/Epi at 15–20 (p = 0.194) and at 30 min (p = 0.035) compared to baseline, but no significant change in platelet reactivity to C/ADP. CS vWF:Ag was inversely related to closure time in response to C/Epi (r = −0.5, p = 0.02). Platelet reactivity in systemic blood was unaltered. There was no change in FVIII:c in either the CS or the femoral vein.
Figure 1.
Effect of angioplasty. Values represent mean (SEM); *p < 0.05, comparison with pre-angioplasty concentrations. CS, coronary sinus; FV, femoral vein; vWF:Ag, von Willebrand factor antigen, C/Epi, closure time in response to collagen/epinephrine; C/ADP, closure time in response to collagen/ADP.
Effect of vWF on platelet reactivity in vitro
Following the addition of 13.4 mg/ml vWF, plasma vWF:Ag increased from 0.65 (0.01) U/ml to 1.39 (0.01) U/ml and greatly enhanced haemostasis in vitro (C/Epi: 140 (7) s fell to 85 (3) s, p = 0.0001; C/ADP: 84 (2) s fell to 71(4) s, p = 0.005).
DISCUSSION
This is the first study in humans to assess the effect of acute coronary occlusion on both vWF and platelet reactivity in the CS. Furthermore, it is the first to directly assess the effect of increasing the plasma vWF load on platelet reactivity in non-vWF deficient subjects. A significant rise in vWF was observed downstream from the site of coronary occlusion and endothelial injury, which was not detectable in peripheral blood, presumably because of a dilutional effect. Of particular importance is the association, in vivo, of increased vWF:Ag with enhanced platelet reactivity to high shear stress. The greatly enhanced platelet reactivity at high shear, observed in vitro by increasing the vWF concentration twofold, suggests a causal association between vWF concentration and the increased platelet reactivity. It has been postulated that vWF is the orchestrator of arterial thrombogenesis, since its interactions with platelet membrane glycoproteins Ib and IIb/IIIa, apparent only at high shear rates, are the key events resulting in thrombosis.
The enhanced dynamic haemostasis seen after angioplasty appears to be caused by the effect of vWF on platelets rather than activation of the coagulation cascade, since FVIII:c was unaltered. The increase in vWF following stent deployment is supported by recent work demonstrating greater platelet activation after stenting than angioplasty,4 associated with late loss in the stent group.
The quantitative vWF:Ag assay was chosen over assays of vWF activity, with changes in platelet reactivity providing functional information. The PFA-100, which sensitively detects von Willebrand disease, was chosen because it employs conditions of high shear, similar to those in a stenosed coronary artery.
Coronary angioplasty can be used as a model to study the effects of acute coronary occlusion caused by spontaneous coronary thrombosis, which occurs with myocardial infarction. The release of vWF into the coronary circulation, with direct effects on platelet reactivity as demonstrated here, may play an important role in thrombosis, both in unstable angina, where platelet rich microemboli have been identified, and in occlusive coronary thrombosis in patients with myocardial infarction. Our hypothesis is supported by the high shear stress conditions that are prevalent in these conditions. Furthermore, since an increase in vWF enhances platelet reactivity, the increased vWF concentrations previously identified in healthy individuals and patients may have pathological significance, representing a predisposition to arterial thrombosis.
Abbreviations
C/ADP, closure time in response to collagen/ADP
C/Epi, closure time in response to collagen/epinephrine
CS, coronary sinus
ELISA, enzyme linked immunosorbent assay
vWF, von Willebrand factor
vWF:Ag, von Willebrand factor antigen
REFERENCES
- 1.Ruggeri ZM. Mechanisms initiating platelet thrombus formation. Thromb Haemost 1997;78:611–6. [PubMed] [Google Scholar]
- 2.Fuster V, Badimon JJ, Badimon L. Clinical-pathological correlations of coronary disease progression and regression. Circulation 1992;86(suppl III):III-1–11. [PubMed] [Google Scholar]
- 3.Mammen EF, Comp PC, Gosselin R, et al. PFA-100TM system: a new method for assessment of platelet dysfunction. Semin Thromb Hemost 1998;24:195–202. [DOI] [PubMed] [Google Scholar]
- 4.Inoue T, Sohma R, Miyazaki T, et al. Comparison of activation process of platelets and neutrophils after coronary stent implantation versus balloon angioplasty for stable angina pectoris. Am J Cardiol 2000;86:1057–63. [DOI] [PubMed] [Google Scholar]