Abstract
Objective: To assess the structural and functional characteristics of pulmonary arteries by intravascular ultrasound (IVUS) in the setting of primary pulmonary hypertension, and to correlate the ultrasound findings with haemodynamic variables and mortality at follow up.
Design: Prospective observational study.
Setting: University hospital (tertiary referral centre).
Patients: 20 consecutive patients with primary pulmonary hypertension (16 female; mean (SD) age, 39 (14) years).
Methods: Cardiac catheterisation and simultaneous IVUS of pulmonary artery branches at baseline and after infusion of epoprostenol.
Results: 33 pulmonary arteries with a mean diameter of 3.91 (0.80) mm were imaged, and wall thickening was observed in all cases, 64% being eccentric. Mean wall thickness was 0.37 (0.13) mm, percentage wall area 31.0 (9.3)%, pulsatility 14.6 (4.8)%, and pulmonary/elastic strain index 449 (174) mm Hg. No correlation was observed between IVUS findings and haemodynamic variables. Epoprostenol infusion increased pulsatility by 53% and decreased the pulmonary/elastic strain index by 41% (p = 0.0001), irrespective of haemodynamic changes. At 18 (12) months follow up, nine patients had died. A reduced pulsatility and an increased pulmonary/elastic strain index were associated with increased mortality at follow up (12.0 (4.4)% v 16.4 (4.4)%, p = 0.03; 369 (67) v 546 (216) mm Hg, p = 0.02).
Conclusions: IVUS demonstrated pulmonary artery wall abnormalities in all patients with primary pulmonary hypertension, mostly eccentric. The severity of the changes did not correlate with haemodynamic variables, and epoprostenol improved pulmonary vessel stiffness. There was an association between impaired pulmonary artery functional state as determined by IVUS and mortality at follow up.
Keywords: intravascular ultrasound, pulmonary hypertension, epoprostenol, pulmonary artery pulsatility
Primary pulmonary hypertension is a life threatening disease characterised by a progressive increase in pulmonary blood pressure that often leads to right ventricular failure and death.1 Median survival is 2.8 years from the time of diagnosis, and mortality reaches 65% at three years of follow up.2 Calcium channel blockers, warfarin, and prostacyclin have improved the prognosis, but the three year mortality has remained as high as 50%.3 The diagnosis of primary pulmonary hypertension is based on clinical and haemodynamic data, and prognosis is determined by the alterations in haemodynamic variables (mean pulmonary artery pressure, cardiac output, mean right atrial pressure).
The assessment of pulmonary artery morphology in primary pulmonary hypertension has been limited to pulmonary angiography and to the histological study of lung samples obtained at biopsy. Pulmonary angiography, which is not free of complications in these cases, only shows the vessel lumen and provides no information about vessel wall abnormalities. Histological evaluation of lung biopsies provides a valuable quantitative and qualitative description of the pulmonary wall changes, but remains a static in vitro examination without functional assessment and requires a thoracotomy. Intravascular ultrasound (IVUS) has been validated as a reliable method for describing pulmonary vessel wall morphology and pulmonary artery pulsatility.4,5 It is a unique form of exploration that can provide a simultaneous morphological and functional evaluation of the pulmonary vasculature. However, pulmonary artery ultrasound imaging has mostly been restricted to the study of patients with secondary pulmonary hypertension6–10 and pulmonary embolism,11,12 and its potential role in evaluating patients with primary pulmonary hypertension is unknown.
The aim of our study was to examine the pulmonary arteries of patients with primary pulmonary hypertension by IVUS in order to establish their morphological and functional characteristics at baseline and after an acute infusion of epoprostenol. We also aimed to correlate clinical and haemodynamic data with ultrasound measurements and to determine the relation between pulmonary IVUS findings and mortality at follow up.
METHODS
Patients
Twenty two consecutive patients with primary pulmonary hypertension who underwent cardiac catheterisation at our institution were included in the study. The diagnosis was made on the basis of the criteria in the National Institutes of Health registry.13
Duration of symptoms, New York Heart Association (NYHA) functional class, and the presence of signs of right ventricular failure were recorded. Clinical follow up was available in all cases. All patients received anticoagulant treatment, and all underwent a clinical test with calcium antagonists. Either intravenous epoprostenol or aerosolised iloprost (both prostacyclin analogues) was prescribed if clinical worsening was observed in patients with baseline NYHA functional class < III, or if no improvement occurred in case of baseline functional class ≥ III. Patients were added to the lung transplant waiting list if clinical worsening persisted despite epoprostenol or iloprost treatment.
The procedures were performed in accordance with the institutional ethics committee, and all patients gave informed consent.
Cardiac catheterisation: acute epoprostenol test
Right and left heart catheterisation was undertaken with femoral access. Cardiac output and cardiac index were calculated by the Fick method, and pulmonary resistance was calculated as mean arterial pulmonary pressure/cardiac output. Right ventricular stroke work index was calculated as: [mean pulmonary artery pressure − mean right atrial pressure] × stroke volume index × 0.0136 (g.m/m2). After baseline measurements, an infusion of epoprostenol was started at a dose of 2 ng/kg/min, and increased progressively until there was a decrease of more than 30% in pulmonary resistance, or until side effects occurred. All haemodynamic variables were measured at the maximum dose of epoprostenol.
Intravascular ultrasound imaging
IVUS examination was done with a 20 MHz, 3.5 French, 64 element circumferential phased array ultrasound catheter (Endosonics Inc, Rancho Cordova, California, USA), with an axial resolution of 200 μm. The ultrasound catheter was advanced into a distal pulmonary artery and images were recorded on videotape (S-VHS). The intention was to image two pulmonary lobes per patient. Ultrasound measurements were recorded at baseline (in all pulmonary arteries studied) and at the maximum dose of epoprostenol (at the same point at which the last pulmonary artery was imaged).
Images of the most distal segment studied were analysed off-line by two observers unaware of clinical and haemodynamic findings. The following measurements were made:
vessel diameter
lumen diameter
wall (intima + media) thickness (mean, maximum, and minimum)
relative wall thickness: mean wall thickness/lumen diameter
lumen area in systole (LAs) and in diastole (LAd)
wall area
area circumscribed by the external elastic membrane (EEM)
percentage wall area: wall area/EEM × 100
eccentricity index: minimum wall thickness/maximum wall thickness
pulsatility: LAs − LAd/LAd × 100
pressure/elastic strain index: (PASP − PADP) × LAd/LAs − LAd, where PASP = pulmonary artery systolic pressure and PADP = pulmonary artery diastolic pressure.
The pulmonary artery wall was considered thickened when maximum wall thickness was > 0.2 mm.7,8 Mean wall thickness was the mean of the four measurements made in each quadrant of the artery. The wall thickening was considered eccentric if eccentricity index was < 0.5. The EEM was represented by the interface between the intima + media and the more echogenic adventitia. Pulsatility was calculated as the average value of three consecutive cardiac cycles. The average value of the measurements made in the two arteries imaged was used for analysis. For the evaluation of the effects of epoprostenol on pulmonary vessel pulsatility, only the last pulmonary artery imaged at baseline was used for comparison (baseline v maximum dose of epoprostenol).
Pathology
The lungs of five patients were available for pathological study. Necropsy was done in two cases and double lung transplantation was carried out in three, at a mean (SD) of 7 (6) months (range 2 days to 17 months) after IVUS examination. Explanted lungs were prepared by the Thurlbeck’s method.14 Five micron thick sections from the samples with medium size arteries were stained with Verhoef–Van Gieson for elastic tissue. One or two elastic pulmonary arteries were selected from the lobes previously assessed by IVUS, and the microscopic image of the vessels was electronically captured, digitised, and calibrated, performing the same measurements as those obtained with ultrasound imaging.
Statistical analysis
Continuous variables were expressed as mean (SD). Student’s t test was used for comparison of means. The comparison of more than two means was done by analysis of variance. The Pearson correlation coefficient was calculated for comparison of continuous variables. Intraobserver and interobserver variability of ultrasound measurements was assessed using the method of Bland and Altman, whereby measurements are repeatable if 95% of the differences are within 2 SD.15 A probability value of p < 0.05 was considered significant.
RESULTS
Clinical and haemodynamic characteristics
Clinical and baseline haemodynamic variables are given in table 1. The mean age of the study population was 39 years (range 16–56 years) and most of the patients were female. Epoprostenol infusion, at a maximum dose of 10.7 (2.4) ng/kg/min, significantly increased the cardiac index (from 1.9 (0.66) to 2.7 (0.79) l/min/m2, p < 0.0001), cardiac output (from 3.3 (1.1) to 4.6 (1.5) l/min, p < 0.0001), stroke volume (from 39.4 (14.4) to 49.2 (19.6) ml, p < 0.0001), and right ventricular stroke work index (from 16.1 (5.9) to 19.9 (8.6) g.m/m2, p = 0.006). The epoprostenol infusion decreased total pulmonary resistance (from 1829 (215) to 1418 (212) dyn.s.cm−5, p < 0.0001), but caused no variation in mean pulmonary artery pressure (from 63 (20) to 64 (28) mm Hg, p = 0.67).
Table 1.
Clinical and haemodynamic characteristics of 20 patients with primary pulmonary hypertension
| Age (years) | 39 (14) |
| Women (n) | 16 |
| Duration of symptoms (months) | 44 (26) |
| NYHA class I–II (n) | 7 |
| NYHA class III–IV | 13 |
| Right ventricular failure (n) | 6 |
| Mean pulmonary artery pressure (mm Hg) | 63 (20) |
| Cardiac output (l/min) | 3.3 (1.1) |
| Stroke volume (ml) | 39.4 (14.4) |
| Right ventricular stroke work index (g.m/m2) | 16.1 (5.9) |
| Total pulmonary resistance (dyn.s.cm−5) | 1829 (962) |
| Mean right atrial pressure (mm Hg) | 9 (5) |
| Systemic oxygen saturation (%) | 92.5 (3.3) |
NYHA, New York Heart Association functional class.
IVUS findings
IVUS examination was undertaken on all patients with no complications. Thirty six pulmonary lobes were studied, but the quality of ultrasound images was considered inadequate for analysis in two patients, who were therefore excluded from the study. In all, 33 pulmonary lobes (all but three inferior lobes) were analysed from 20 patients (two pulmonary lobes were studied in 13, and only one lobe in seven because of low patient tolerance or difficulty in catheterising a second pulmonary artery). We were able to analyse the structural characteristics of the pulmonary wall in 25 pulmonary arteries, but morphological measurements were not made in eight because the EEM could not be delineated. Pulsatility was calculated in 31 of the 33 arteries studied. All measurements were reproducible on the basis of the Bland and Altman analysis.
The results of IVUS measurements are summarised in table 2. All patients had thickened pulmonary artery walls, leading to a mean reduction in lumen area of 31.0 (9.3)%. Wall thickening was eccentric in most of the arteries (64%), with a mean eccentricity index of 0.44 (0.20) (fig 1).
Table 2.
Intravascular ultrasound data
| Vessel diameter (mm) | 3.91 (0.80) |
| Maximum wall thickness (mm) | 0.51 (0.20) |
| Mean wall thickness (mm) | 0.37 (0.13) |
| Relative wall thickness | 0.12 (0.04) |
| Eccentricity index | 0.44 (0.20) |
| Wall area (mm2) | 3.80 (1.53) |
| Percentage wall area (%) | 31.0 (9.3) |
| Pulsatility (%) | 14.6 (4.8) |
| Pressure/elastic strain index (mm Hg) | 449 (174) |
Figure 1.
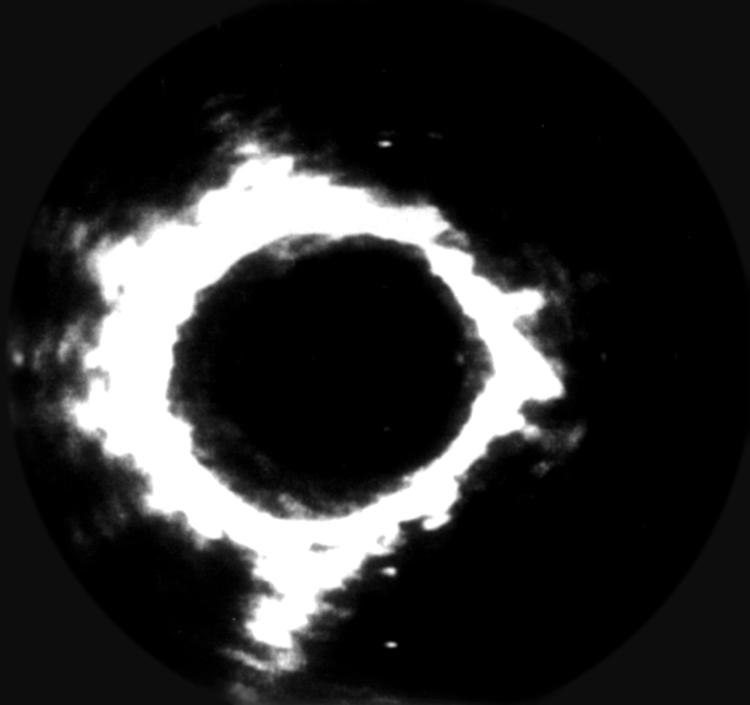
Cross sectional IVUS image from a patient with primary pulmonary hypertension. Note the intima + media thickening (soft echoes) between the arterial lumen and the outer echobright layer (adventitia). Wall thickening is eccentric, with more prominent changes between 5 and 12 o’clock. Distance between two white points is 1 mm. The circular artefact within the lumen is generated by the ultrasound catheter.
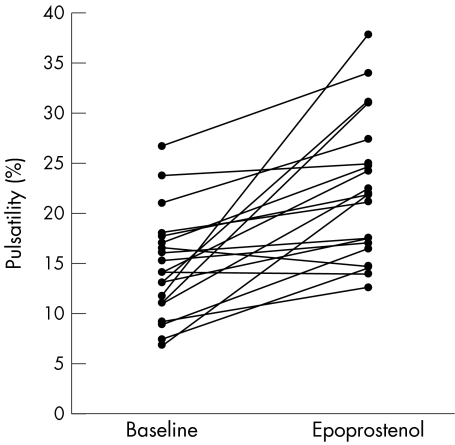
Epoprostenol increased the pulsatility and decreased the pressure/elastic strain index of pulmonary arteries to some degree in all but two of the patients (fig 2). Pulsatility increased by 53% compared with baseline (from 14.6 (5.2)% to 22.4 (7.0)%, p = 0.0001), and the pressure/elastic strain index decreased by 41% (from 440 (177) to 258 (121) mm Hg, p = 0.0001).
Figure 2.
Effect of acute administration of intravenous epoprostenol on pulmonary artery pulsatility measured by intravascular ultrasound. Epoprostenol increased vessel pulsatility from 14.6 (5.2)% to 22.4 (7.0)% (p = 0.0001), and some improvement was detected in 18 of the 20 patients studied (90%).
Relation between clinical status, baseline haemodynamics, and IVUS findings
There was no correlation between clinical variables (duration of symptoms, NYHA class, presence of right cardiac failure), baseline haemodynamics, and IVUS measurements. The degree of pulsatility and pressure/elastic strain index changes induced by epoprostenol also did not correlate with the haemodynamic changes, baseline haemodynamics, or morphological ultrasound measurements (r < 0.5 with p > 0.05 for all correlations).
Follow up
Clinical follow up was available in all cases. At a mean follow up of 18 (12) months, nine patients had died, three had undergone lung transplantation, and eight had remained clinically stable with no significant change or a mild to moderate improvement in baseline functional class. Five patients received intravenous epoprostenol and two were treated with aerosolised iloprost. Death was of cardiac origin in all cases, and occurred at a mean of 7 (8) months (range 2 days to 19 months) after cardiac catheterisation. Three patients died suddenly, and the rest had a rapid clinical deterioration, dying within the two weeks after the worsening of symptoms.
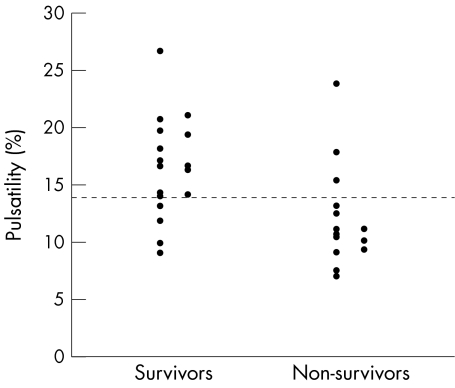
None of the structural variables measured by IVUS had a significant relation to clinical follow up. However, baseline pulmonary artery pulsatility was decreased in patients who died during follow up compared with those who survived (12.0 (4.4)% v 16.4 (4.4)%, p = 0.03). The pressure/elastic strain index was also higher in patients who died at follow up (369 (67) v 546 (216) mm Hg, p = 0.02). The baseline pulsatility values of all pulmonary arteries imaged, grouped according to clinical outcome, are presented in fig 3.
Figure 3.
Baseline pulsatility in all pulmonary arteries studied, grouped according to clinical outcome. The median value of pulmonary pulsatility was 14.0%, range 7.7–26.7% (discontinuous line). Note that among the patients who survived, 13 of the 17 pulmonary arteries studied had a pulsatility above the median value. On the other hand, among the nine who died at follow up, only three of the 14 pulmonary arteries studied had a pulsatility of ≥ 14%.
Pathological findings
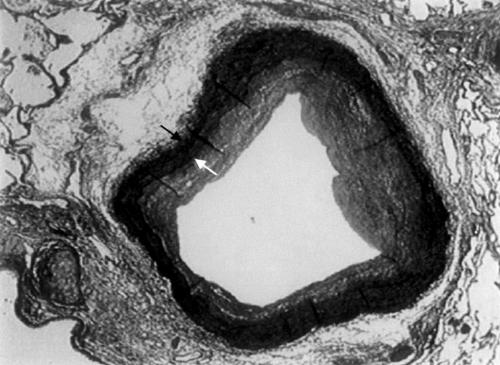
Histological measurements were made in nine elastic pulmonary arteries, with a mean diameter of 2.77 (1.26) mm. Intimal proliferation and medial hypertrophy was demonstrated in all arteries (fig 4). Mean wall thickness was 0.41 (0.21) mm, maximum wall thickness was 0.58 (0.28) mm, relative wall thickness was 0.13 (0.04), wall area was 3.79 (3.27)mm2, percentage wall area was 55 (12)%, and the proportion of the wall area occupied by the intima was 33 (16)%. Wall thickening was eccentric in 56% of cases, with an eccentricity index of 0.44 (0.15). Intimal proliferation and medial hypertrophy were eccentric in six and seven of the nine arteries studied, respectively. Eccentricity values for intima and media were 0.36 (0.16) and 0.47 (0.22), respectively.
Figure 4.
Histological section of an elastic pulmonary artery obtained from the necropsy specimen of a patient with primary pulmonary hypertension, showing significant structural changes caused by proliferation of the intima and medial hypertrophy. Black and white arrows show the external and internal elastic lamina, respectively. Note the irregularity of intimal proliferation and medial hypertrophy, leading to eccentric wall thickening (×7.8, Verhoef Van Giesson stain).
DISCUSSION
IVUS adequately depicted the arterial wall changes observed in the elastic pulmonary vessels of patients diagnosed with primary pulmonary hypertension. The pulmonary arterial wall was thickened in all cases to varying degrees, mostly in eccentric form. Also, ultrasound imaging allowed functional evaluation of the pulmonary vasculature by measuring arterial pulsatility. No relation could be demonstrated between ultrasound morphology, pulsatility, and haemodynamic indices. An acute vasodilator test with intravenous epoprostenol improved pulsatility and the pressure/elastic strain index to a variable extent in 90% of cases, irrespective of the absence of changes in pulmonary artery pressure. Pulsatility and the pressure/elastic strain index were the only ultrasound imaging variables that were shown to have prognostic value. Thus pulsatility and the pressure/elastic strain index were significantly lower and higher, respectively, in patients who died at the mid term follow up compared with those who survived.
IVUS evaluation of pulmonary artery morphology
The pulmonary arteries in primary pulmonary hypertension are characterised by intimal proliferation and fibrosis, medial hypertrophy, adventitial proliferation, thrombotic lesions, and obliteration of small arteries.16,17 IVUS was able to explore elastic pulmonary arteries ranging from 2.4–5.3 mm in vessel diameter, showing wall thickening in all cases. Pulmonary vessel changes were caused by different degrees of intimal proliferation and medial hypertrophy, as demonstrated by the pathology. These changes were eccentric in most cases, owing to non-uniform medial hypertrophy and intimal proliferation (fig 4). However, none of the structural wall changes detected by IVUS correlated with haemodynamic variables.
Previous pulmonary ultrasound studies in patients with pulmonary hypertension have reported divergent results with respect to the relation between ultrasound morphological changes and haemodynamic variables.6,7,9,10 The lack of correlation between pulmonary morphology and haemodynamics could be explained by the fact that the degree of pulmonary vascular disease is not uniform over the whole lung, and only one to two pulmonary arteries could be selected for analysis among all the pulmonary vasculature. Furthermore, the earliest alterations observed in primary pulmonary hypertension occur in the small muscular arteries and arterioles,17 and the structural changes observed in elastic pulmonary arteries are secondary, only partially reflecting the severity of distal disease. Finally, pulmonary wall changes are at the same time the consequence of existing pulmonary hypertension and the cause of its further evolution, so that these two variables could have a significant overlap.
The severity of the ultrasound morphological changes of the pulmonary vessels was of no value in predicting mortality at follow up in our study. Palevsky and colleagues studied the lung samples obtained at biopsy in patients with primary pulmonary hypertension and showed that the only pulmonary wall change predictive of poor outcome at mid term follow up was the area occupied by the intima.18 We were not able to differentiate the intima from the medial hypertrophy owing to the homogeneous echogenicity across the different layers of the artery wall, which precluded measurement of the area occupied by the intima.
Functional evaluation of elastic pulmonary arteries
Previous studies have shown a reduced pulsatility in cases of secondary pulmonary hypertension compared with controls, in whom pulmonary pulsatility was about 20%.6,9 We have shown here that pulmonary pulsatility is below 18% in most cases of primary pulmonary hypertension, and a greater reduction in baseline pulsatility was associated with a high mortality at follow up. The pulsatility of an artery depends on the mechanical forces working on the vessel wall, and the intrinsic and vasomotor properties of the arterial wall. Vascular remodelling is a prominent feature of primary pulmonary hypertension, and several changes of the vessel wall could explain the reduced pulsatility observed in these cases. Alterations in the intima (proliferation and fibrosis) and media (increased fibrosis) are described. Also, important changes occur in the adventitia, where the production of extracellular matrix (collagen, elastin, fibronectin, and tenascin) is increased. The absence of a relation between pulsatility and haemodynamic variables suggests that the changes in pulmonary vessel structure are responsible for the functional alteration shown by ultrasound. The reduced pulsatility in patients who died at follow up probably reflects more advanced disease with more severe changes in the vascular structure of the elastic pulmonary arteries. Furthermore, arterial stiffening has been shown to increase left ventricular systolic stress, favouring cardiac dysfunction,19,20 and a deleterious effect of a reduction in pulmonary artery compliance on right ventricular function has also been suggested.21 This may have contributed to the higher mortality observed in the patients with decreased pulmonary artery pulsatility.
Prostacyclin is a short acting vasodilator and platelet inhibitor that is produced by the vascular endothelium. However, it does not usually have a potent vasodilator effect when given intravenously as an acute test in patients with primary pulmonary hypertension, and there is often minimal or even absent lowering of mean pulmonary artery pressure.22 However, long term treatment with epoprostenol (a prostacyclin analogue) produces sustained haemodynamic benefit and improved survival, even in patients with no response to an acute infusion.3,18,22–24 It has been suggested that an effect of epoprostenol on pulmonary vascular remodelling is responsible for these beneficial long term effects.25–27 Our study has shown that intravenous epoprostenol could significantly improve pulmonary artery pulsatility irrespective of haemodynamic changes. In the light of the established relation between cardiac flow indices and global pulmonary vascular compliance, the absence of a correlation between increases in cardiac output/stroke volume and changes in pulmonary artery pulsatility induced by epoprostenol was unexpected. Although cardiac function and pulmonary artery pulsatility improved in most patients, there was no correlation between the changes in these variables. One explanation for this could be that pulmonary pulsatility was measured as lumen area change in a single elastic pulmonary artery and not as overall distensibility of the pulmonary vascular bed, a problem compounded by the heterogeneity of pulmonary blood flow.28 Also, the absence of a relation between pulmonary flow and pulsatility changes induced by epoprostenol might suggest a direct positive effect of this type of drug on the vasomotor properties of the artery wall, which have been shown to contribute substantially to vessel elasticity.29 However, only by measuring the pulmonary flow changes at the level of the artery imaged could we have determined whether the improvement in pulmonary pulsatility was the result of vasomotor changes in the artery wall or an increase in blood flow, or both.
Limitations
As indicated in previous studies, the recognition of the elastic external membrane is the most important limiting factor for ultrasound pulmonary morphology evaluation. In our study, IVUS did not provide adequate images for morphological evaluation in up to 25% of the pulmonary arteries evaluated, and two patients had to be excluded because of the poor quality of the images. However, in most cases ultrasound images were adequate for analysis, and IVUS measurements were reproducible A relation between ultrasound and pathological findings could not be established because the mean delay between the ultrasound exploration and the histopathological studies was too long, and even if the pathologist had studied elastic pulmonary arteries from the same pulmonary lobe as had previously been imaged by IVUS, it would not have been possible to evaluate the same elastic pulmonary artery.
A control group would have provided more consistency in the study results, although previous studies with control subjects have already defined the ultrasound characteristics of pulmonary arteries with no pathological features.6,7 Also, the inclusion of a control group would have incurred ethical objections.
Finally, the small sample size inevitably lessens the potential of the results obtained and precludes the performance of multivariate analysis to establish the prognostic value of the ultrasound findings more accurately.
Conclusions
IVUS provides combined morphological and functional evaluation of the elastic pulmonary vessels of patients with primary pulmonary hypertension and allows direct assessment of the acute changes induced in the pulmonary vessel wall dynamics by epoprostenol. The exploration is safe, and can be undertaken at the same time as cardiac catheterisation. Finally, there is an association between impaired pulmonary artery functional state as determined by IVUS and mortality at follow up. However, larger series are needed to determine the exact prognostic value of this technique in the setting of primary pulmonary hypertension.
Acknowledgments
We thank Aida Ribera for statistical analysis. This study was supported in part by a grant from the Societat Catalana de Cardiologia.
Abbreviations
EEM, external elastic membrane
IVUS, intravascular ultrasound
LAs, lumen area in systole
LAd, lumen area in diastole
NYHA, New York Heart Association
PADP, pulmonary artery diastolic pressure
PASP, pulmonary artery systolic pressure
P/EE, pulmonary/elastic strain index
REFERENCES
- 1.Rubin LJ. Primary pulmonary hypertension. N Engl J Med 1997;336:111–17. [DOI] [PubMed] [Google Scholar]
- 2.D’Alonzo GE, Barst RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension: results from a national prospective registry. Ann Intern Med 1991;115:343–9. [DOI] [PubMed] [Google Scholar]
- 3.Shapiro S, Oudiz R, Cao T, et al. Primary pulmonary hypertension: improved long-term effects and survival with continuous intravenous epoprostenol infusion. J Am Coll Cardiol 1997;30:343–9. [DOI] [PubMed] [Google Scholar]
- 4.Pandian NG, Weintraub A, Kreis A, et al. Intracardiac, intravascular, two-dimensional high frequency ultrasound imaging of pulmonary artery and its branches in humans and animals. Circulation 1990;81:2007–12. [DOI] [PubMed] [Google Scholar]
- 5.Ishii M, Kato H, Kawano T, et al. Evaluation of pulmonary artery histopathologic findings in congenital heart disease: an in vitro study using intravascular ultrasound imaging. J Am Coll Cardiol 1995;26:272–6. [DOI] [PubMed] [Google Scholar]
- 6.Porter TR, Taylor DO, Fields J, et al. Direct in vivo evaluation of pulmonary arterial pathology in chronic congestive heart failure with catheter-based intravascular ultrasound imaging. Am J Cardiol 1993;71:754–7. [DOI] [PubMed] [Google Scholar]
- 7.Borges AC, Wensel R, Opitz C, et al. Relationship between haemodynamics and morphology in pulmonary hypertension. A quantitative intravascular ultrasound study. Eur Heart J 1997;18:1988–94. [DOI] [PubMed] [Google Scholar]
- 8.Berger RMF, Cromme-Dijkhuis AH, Van Vliet AM, et al. Evaluation of the pulmonary vasculature and dynamics with intravascular ultrasound imaging in children and infants. Pediatr Res 1995;38:36–41. [DOI] [PubMed] [Google Scholar]
- 9.Ivy D, Neish SR, Knudson O, et al. Intravascular ultrasonic characteristics and vasoreactivity of the pulmonary vasculature in children with pulmonary hypertension. Am J Cardiol 1998;81:740–8. [DOI] [PubMed] [Google Scholar]
- 10.Bressollette E, Dupuis J, Bonan R, et al. Intravascular ultrasound assessment of pulmonary vascular disease in patients with pulmonary hypertension. Chest 2001;120:809–15. [DOI] [PubMed] [Google Scholar]
- 11.Görge G, Erbel R, Schuster S, et al. Intravascular ultrasound in diagnosis of acute pulmonary embolism. Lancet 1991;337:623–4. [DOI] [PubMed] [Google Scholar]
- 12.Ricou F, Nicod PH, Moser KM, et al. Catheter-based intravascular ultrasound imaging of chronic thromboembolic pulmonary disease. Am J Cardiol 1991;67:749–52. [DOI] [PubMed] [Google Scholar]
- 13.Rich S, Dantzker DR, Ayres SM, et al. Primary pulmonary hypertension: a national prospective study. Ann Intern Med 1987;107:216–23. [DOI] [PubMed] [Google Scholar]
- 14.Lanston C, Waszkiewitz E, Thurlbeck WM. A simple method for the representative sampling of lung of diverse size. Thorax 1979;34:527–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;i:307–10. [PubMed] [Google Scholar]
- 16.Wagenvoort CA, Wagenvoort N. Primary pulmonary hypertension. A pathologic study of the lung vessels in 156 clinically diagnosed cases. Circulation 1970;42:1163–84. [Google Scholar]
- 17.Pietra G, Edwards W, Kay M, et al. Histopathology of primary pulmonary hypertension. A qualitative and quantitative study of pulmonary blood vessels from 58 patients in the national heart, lung, and blood institute, primary pulmonary hypertension registry. Circulation 1989;80:1198–206. [DOI] [PubMed] [Google Scholar]
- 18.Palevsky HI, Schloo BL, Pietra GG, et al. Primary pulmonary hypertension. Vascular structure, morphometry, and responsiveness to vasodilator agents. Circulation 1989;80:1207–21. [DOI] [PubMed] [Google Scholar]
- 19.Elzinga G, Westerhof N. Pressure and flow generated by the left ventricle against different impedances. Circ Res 1973;32:178–86. [DOI] [PubMed] [Google Scholar]
- 20.Maruyama Y, Osama N, Nozaki E, et al. Effects of arterial distensibility on left ventricular ejection in the depressed contractile state. Cardiovasc Res 1993;27:182–7. [DOI] [PubMed] [Google Scholar]
- 21.Fourie PR, Coetzee AR, Bolliger CT. Pulmonary artery compliance: its role in right ventricular-arterial coupling. Cardiovasc Res 1992;26:839–44. [DOI] [PubMed] [Google Scholar]
- 22.Barst RJ, Rubin LJ, Long WA, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. N Engl J Med 1996;334:296–301. [DOI] [PubMed] [Google Scholar]
- 23.Mclaughlin V, Genthner D, Panella M, et al. Reduction in pulmonary vascular resistance with long-term epoprostenol (prostacyclin) therapy in primary pulmonary hypertension. N Engl J Med 1998;338:273–7. [DOI] [PubMed] [Google Scholar]
- 24.Higenbottam T, Butt AY, McMahon A, et al. Long term intravenous prostaglandin (epoprostenol or iloprost) for treatment of severe pulmonary hypertension. Heart 1998;80:151–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vane JR, Botting RM. Pharmacodynamic profile of prostacyclin. Am J Cardiol 1995;75:3–10A. [DOI] [PubMed] [Google Scholar]
- 26.Wharton J, Davie N, Upton PD, et al. Prostacyclin analogues differentially inhibit growth of distal and proximal human pulmonary artery smooth muscle cells. Circulation 2000;102:3130–6. [DOI] [PubMed] [Google Scholar]
- 27.Barst RJ. Treatment of primary pulmonary hypertension with continuous intravenous prostacyclin. Heart 1997;77:299–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glenny RW. Blood flow distribution in the lung. Chest 1998;114:8–16S. [DOI] [PubMed] [Google Scholar]
- 29.Lee R, Kamm RD. Vascular mechanics for the cardiologist. J Am Coll Cardiol 1994;23:1289–95. [DOI] [PubMed] [Google Scholar]