Transient loss of consciousness is a dramatic symptom, which has many possible mechanisms and hence different therapeutic, psychosocial, and prognostic implications. It is a common cause both for emergency room visits and for hospitalisation, and has recently been the topic of a task force within the European Society of Cardiology (ESC).1 Syncope is a symptom, defined as a transient, self limited loss of consciousness with a relatively rapid onset and usually leading to falling; the subsequent recovery is spontaneous, complete, and usually prompt. The underlying mechanism is a transient global cerebral hypoperfusion. Seizure is, according to the same document, synonymous with an epileptic fit, which is the manifestation of a paroxysmal discharge of abnormal rhythms in some part of the brain, and “Epilepsy is then defined as a condition in which seizures recur, usually spontaneously”.2 The diagnosis thus requires that the episodes are spontaneous or unprovoked and recurrent.3 In order to differentiate between syncope and seizure, videotelemetry with simultaneous electroencephalographic (EEG) and electrocardiographic (ECG) recording with multiple scalp and chest electrodes is required—a situation that is rarely fulfilled.
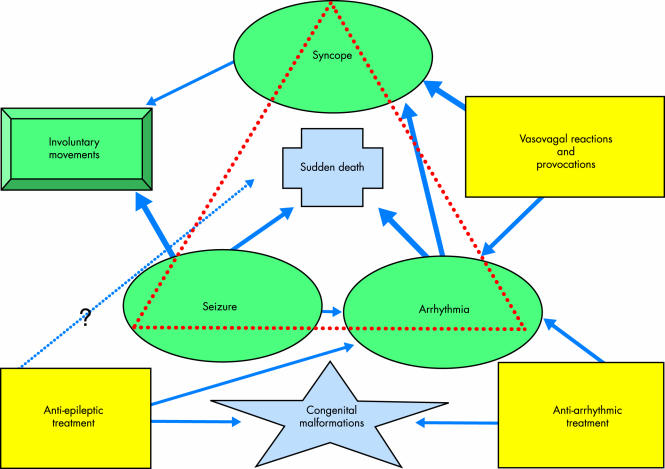
There are clinically important relations between cardiovascular causes of syncope and seizure disorders (fig 1). Involuntary movements, often referred to as myoclonic jerks, may accompany syncope due to cardiovascular causes and create a differential diagnostic problem against seizure with important therapeutic and prognostic implications. These implications are basically: the underlying disease may not receive proper treatment, and some cardiac causes of syncope carry a considerable mortality risk; bradycardias might be aggravated by some (ion channel active) antiepileptic drugs (AEDs); and a diagnosis of epilepsy may also lead to significant psychosocial consequences.4 Put slightly differently: “Hardly anyone with epilepsy will come to any harm from a delay in diagnosis whereas a false positive diagnosis is gravely damaging”.2 Therefore seizure-like or convulsive syncope from the cardiovascular perspective has been chosen as the topic for this article. “Convulsive syncope” is not a recommended term by the ESC task force, “ …because it carries the risk of increasing confusion between syncope and epilepsy”.1 Unfortunately, there is no simple term to denote syncope accompanied by “myoclonic jerks” or “jerking movements”, which are preferred; therefore, for linguistic reasons and because it is used in some of the references, “convulsive syncope” is used in this article, which focuses on cardiovascular or cardiogenic syncope.
Figure 1.
Relations between syncope, seizure, and arrhythmia. There are clinically important relations between syncope and seizure disorders. Diagnostic mistakes are frequent when loss of consciousness is followed by involuntary movements, usually referred to as myoclonic jerks. The main cardiovascular mechanisms causing cerebral hypoperfusion and convulsive syncope are vasovagal reactions and brady- and tachyarrhythmias. Also other connections exist between syncope and seizure disorders as outlined in this figure. The thickness of the arrows reflects the strength of the scientific documentation and/or the relation. See text and references for further information.
MISDIAGNOSIS IS NOT UNCOMMON
According to the literature the problem is rather one of misdiagnosing epileptic fits and missing a cardiovascular syncope, rather than the other way around, which does not exclude the occurrence of, for example, improper pacemaker implantation in patients with fits and falls of neurological origin. Syncope accompanied by myoclonic jerks might occur in up to a fifth or more of patients in cohorts with presumed seizure disorders, depending upon how far the initial diagnostic procedure and re-evaluation, respectively, has been pursued; initially undetected cardiovascular causes are most common (table 1).3,5,6 Fortunately, the co-existence of syncope and seizure disorders in the same patient seems to be rare, at least according to one study by Gastaut, who found syncope in only three out of 797 patients with epileptic seizures (“ictal bradycardia syndrome”).
Table 1.
Misdiagnosis of epilepsy in three population based and three cohort studies of patients with presumed seizure disorder. The third column states the number of re-evaluated cases, and the fourth in how many cases the initial diagnosis was considered wrong. Various clinical explanations emerged on re-evaluation; the number of cases with syncope and the confirmed cardiovascular mechanisms are presented in the right hand column.
| Author | Referral population | Presumed epilepsy | Misdiagnosis | Syncope/cardiovascular mechanism |
| Scheepers3 | 40.000 | 261 (249*) | 49 (+ 26 ?) | 15 syncope/vasovagal, carotid sinus syndrome, postural hypotension, bradycardia, congenital heart disease |
| King5 | 500000 | 496* | 178 | 60 convulsive syncope; 13 syncope |
| Smith6 | NA | 184 | 46 | 13 syncope |
| Grubb13 | NA | 15 | 10 | 10 syncope/vasovagal (10) |
| Linzer14 | NA | 12 | 12 | 12 syncope/vasovagal (5), TdP (4), bradycardia (2), SVT (1) |
| Zaidi15 | NA | 74 | 31 | 29 syncope/vasovagal (20), carotid sinus syndrome (7), bradycardia (2) |
*≥5 years of age.
NA, not available, SVT, supraventricular tachycardia; TdP, torsade de pointe polymorphic ventricular tachycardia.
MECHANISTIC ASPECTS OF SEIZURE-LIKE SYNCOPE
Myoclonus or myoclonic jerks (sometimes tonic spasms) is probably the most misleading symptom in the differential diagnosis between syncope and seizure disorders. It is frequently part of spontaneous or provoked syncope related to vasovagal reactions, and has been reported in 12% of blood donors,7 in approximately 20% of individuals during ocular compression,8 in 40 (66%) out of 61 with syncope induced by the Weber manoeuvre among 200 young men exposed,9 in 38 (90%) of 42 syncopal episodes among 56 patients provoked by a combination of hyperventilation during squatting, followed by fast rising and 10 seconds of Valsalva,10 and in 21 (75%) of 28 with vasovagal syncope induced by tilt table testing out of 279 consecutive patients with transient loss of consciousness suggestive of syncope.11 There is some (11/16, 69%), but not complete intra-individual concordance in the reactions to ocular compression and head-up tilt testing in young patients with recurrent unexplained syncope.w1 While there was a correlation between the duration of asystole (cardioinhibition) and the clinical manifestations during ocular compression, this was not the case during the Weber manoeuvre and head-up tilt. The conclusion is that what matters is the degree of cerebral anoxia, not whether it is induced by cardioinhibition or vasodilation, or a combination.
Multifocal jerks sometimes superimposed on generalised myoclonus seem most common,9,10 but other features have also been reported such as eye movements and vocalisations, as well as tonic spasms7–9 or righting movements (head rising, sitting or standing up).10 These signs might be very difficult to distinguish from seizure disorders not only for the layman. In addition, amnesia was a common feature in the studies above, not surprisingly, since impaired blood supply to the brain is one cause of “transient global amnesia”. In consequence, the patient might not be able to describe symptoms immediately preceding the episode, and even believe or deny there was any. The history from a witness might therefore be crucial.
EEG recordings have shown generalised high amplitude brain wave slowing and flattening, without cortical discharges, as observed during generalised cerebral anoxia12 and distinctly different from epileptic activity.8–10 The convulsive activity has tentatively been ascribed to activation (or loss of suppression) of the medullar reticular formation.8,10
A comparison of the clinical features of cardiogenic syncope and seizure disorders is presented in table 2.
Table 2.
Comparison of clinical features in cardiogenic syncope versus seizure disorders
| Clinical features | Cardiogenic syncope | Seizure disorders |
| Loss of consciousness | Typical | Common |
| Episode duration | Seconds | Minutes |
| Involuntary movements | Common | Typical |
| Amnesia | Yes | Yes |
| Arrhythmia | Common | Rare* |
| Electroencephalogram | Slow waves Flattening | Focal or general spike activity |
| Responsive to AEDs | No | Often |
| Short term mortality† | High | Low |
*Except sinus tachycardia.
†Within a year.
AEDs, antiepileptic drugs.
RE-EVALUATION OF AN EPILEPSY DIAGNOSIS
Three studies, involving altogether 101 patients, have focused on patient cohorts with presumed and re-evaluated seizure disorders.13–15 One hundred of them were treated with, but were unresponsive to, AED therapy. In these studies it was confirmed that vasovagal syncope may be accompanied by myoclonus, as well as carotid sinus hypersensitivity and primary arrhythmias such as bradycardia, caused by sinus node dysfunction and intermittent atrioventricular (AV) block, as well as ventricular (torsade de pointe) and, more rarely, supraventricular tachycardia.
Certain features might prompt the re-evaluation of a diagnosis of presumed epilepsy and engage the cardiologist. The diagnostic strategy can be chosen based on the age of the individual patient: in the very young patient the efforts should be directed towards vasovagal syncope or variants of the long QT syndrome, while in older patients sinus node disease or intermittent high degree AV block should be looked for; in the highest age group carotid sinus syndrome should be investigated. Hence, the primary diagnostic tools are standard ECG, head-up tilt testing (including pharmacological provocation with glyceryl trinitrate or isoprenaline), invasive electrophysiological study (including pharmacological provocation), carotid sinus massage, and possibly implantable loop recorders (ILRs). Most aspects of these techniques have been covered in the recent task force report1; a few points will, however, be stressed here. In suspected sinus node disease and intermittent high degree AV block the diagnostic yield is low both for exercise testing and Holter monitoring. The diagnostic yield of the invasive electrophysiological evaluation is also often limited at baseline, and hence often dependent on drug provocation: class IA substances are useful in suspected His-Purkinje disease,w2 autonomic tone inhibition with atropine and propranolol in suspected sinus node dysfunction,w3 and isoprenaline for the induction of supraventricular tachycardia, especially AV node re-entrant tachycardia.w4 Documentation on the usefulness of the implantable loop recorder in patients with “presumed epilepsy” is so far limited to a dozen patients,14,15 while data on its value in the evaluation of patients with “unexplained syncope” (negative tilt and electrophysiological testing without pharmacological provocation) is starting to come forth.16 w5 With the development of a new generation of ILRs with ECG recording activated both by the patient and by preset arrhythmia criteria, its application in patients with the present type of problem will probably increase. There are, however, major limitations with this device since no other physiologic variable (such as blood pressure or oxygen saturation) is recorded, and it is non-therapeutic, which might be hazardous—for example, in patients with intermittent high degree AV block or ventricular arrhythmias.
CARDIAC EFFECTS OF ANTIEPILEPTIC DRUGS
Some antiepileptic drugs like carbamazepine and phenytoin exert their therapeutic action through ion channel effects, and the structure of some of the ion channels is similar in different organ systems. Sodium channel blocking drugs used for neurologic or cardiac purposes have minor effects on the healthy heart, but negative chronotropic and dromotropic effects in the sick heart. This may cause adverse effects, but might also be taken advantage of in pharmacologically provocative tests, as mentioned above. In the present context and in the patient with presumed epilepsy, increase in the frequency of episodes of unconsciousness with or without convulsions following the initiation or dose increment of an ion channel active substance should raise the suspicion of intermittent bradycardia either as the cause of syncope or as provoking a coexisting condition, especially in the elderly. Dysfunction of the entire conduction system, including the sinus node, might be induced by carbamazepine in some patients,17 a susceptibility which might be disclosed on the surface ECG by, for example, bundle branch block or exaggerated sinus cycle variations.w6
The embryonic heart might also be affected by ion channel active AEDs, which might cause developmental defects similar to what have been described for some class III antiarrhythmic drugs.w7 This is alluded to in fig 1, but will not be discussed further.
DO SEIZURES PROVOKE ARRHYTHMIAS?
Although sinus tachycardia is frequently observed in relation to seizures, systematic studies suggest that clinically significant arrhythmias are rarely provoked by epileptic fits. In one study 338 patients with seizure disorders, of whom 241 were less than 40 years of age, were followed with ambulatory ECG for 20–24 hours.18 There were 56 episodes of electrographic seizures (both focal and generalised) lasting at least 10 seconds, but there was no significant arrhythmia. However, adding to the complexity of the brain–heart interaction, a rarely occurring “ictal bradycardia syndrome” has been described, mostly related to temporal lobe epilepsy, preferentially in male patients, who in a significant proportion were older than 50 years.19 The diagnosis is based on simultaneous EEG and ECG recording with electrographic seizure activity preceding bradycardia and subsequent syncope accompanied by electrographic activity typical for cerebral hypoperfusion. A combination of AED treatment and pacemaker therapy might be required in such patients, if a cure cannot be offered by surgery for the epilepsy.w8
Sudden unexpected death in epilepsy (SUDEP) is also an issue of great concern and a growing area of research.w9 w10 The mechanistic role of cardiac arrhythmias in this setting is an obvious matter of interest. The risk factors observed in patients with SUDEP are a high frequency of episodes (> 50 v 1–2/year), increasing number of antiepileptic drugs taken concomitantly (3 v 1 drug), early versus late onset epilepsy, frequent changes of drug treatment, and low postmortem concentrations of such drugs.20 w10 Against this background it seems unlikely—albeit not proven—that patients with an arrhythmic cause of convulsive syncope constitute a significant fraction of those ascribed to as succumbing to SUDEP.
Withdrawal of carbamazepine was in a small group of patients, however, found to be accompanied by changes in heart rate variability and electrocardiographic signs of an increased arrhythmogenic state.w11 Along the same line decreased heart rate variability (the majority with AED polytherapy),w12 and changes in the QTc interval (AED treatment not stated),w13 have been proposed as possible signs of increased propensity for arrhythmia. Looking specifically at patients with refractory epilepsy—a high risk group for SUDEP—a relation was observed between the duration and type of seizures (generalised tonic–clonic) and the accompanying ECG abnormalities, of which some were potentially serious.w14 The cardiovascular consequences of a seizure is thus dependent on seizure characteristics (including duration), respiratory impairment, drug treatment, and the pre-ictal physical state, especially any coexisting cardiovascular and/or pulmonary disorders.
FINDING THE MECHANISM OF CONVULSIVE SYNCOPE: A TENTATIVE STRATEGY
The cardiovascular part of the re-evaluation of a diagnosis of presumed epilepsy basically follows the initial evaluation of syncope in general: a careful history, a physical examination including orthostatic blood pressure measurement, and an ECG.1 A family history should always be included, both from a diagnostic and prognostic point of view, bearing in mind the possibility of familial sudden death as part of the long QT syndrome and hypertrophic cardiomyopathy. Again, the importance of obtaining a history from a witness should be emphasised, not the least because of the possibility of post-ictal amnesia.
Then, from what we know about likely cardiovascular causes of convulsive syncope, and because of the important prognostic impact of the presence of heart disease, echocardiography and exercise testing should be part of the initial evaluation—with the possible exception of the very young, and the previously healthy person with loss of consciousness not provoked by physical exercise, when left ventricular hypertrophy or other structural anomalies of the heart should always be ruled out.
Vasovagal syncope—or neurally mediated reflex syncope—is obviously one of the most common causes of convulsive syncope, and when the history alone does not allow a diagnosis head-up tilt testing is the preferred diagnostic tool.
While invasive electrophysiological evaluation in pursuit of sinus node dysfunction or intermittent AV block comes relatively early in the higher age groups, it is rarely indicated in the otherwise healthy young individual. However, in patients with palpitations preceding loss of consciousness, non-invasive or invasive (with a possibility to add on an ablation) electrophysiological evaluation apparently comes very early. In patients with structural heart disease and tachycardias, symptoms other than palpitations—apart from loss of consciousness—might dominate, such as dyspnoea, fatigue, or chest pain. The diagnostic yield of the invasive electrophysiological evaluation is, however, limited in the absence of ECG abnormalities or evidence of structural heart disease, although pharmacological provocation might improve the yield. Unfortunately, the same is true for 24–48 hour Holter monitoring,w15 and only a positive diagnosis is reliable. Therefore, the absence of a significant arrhythmia during the two latter procedures does not rule out its causative role. It therefore sometimes becomes a clinical dilemma whether to pursue a positive diagnosis of an arrhythmia with an ILR, without therapeutic modalities, or implant a pacemaker or a cardioverter-defibrillator, with combined diagnostic and therapeutic options.
Carotid sinus massage should be part of the evaluation, at least in patients older than 40 years.
Table 3 summarises the tentative strategy outlined above.
Table 3.
Tentative strategy for evaluation of the cardiovascular mechanism of syncope in a patient without palpitations or history of familial (genetic) disease predisposing to loss of consciousness, and episodes less frequent than weekly. A surface ECG is considered a mandatory part of the initial evaluation, as well as hospitalisation and ECG monitoring, if the patient arrives at the emergency department because of a recent episode. Echocardiography for evaluation of cardiac structure and function is a useful early investigation.
| Surface ECG abnormal, but not immediately diagnostic |
| A Cardiovascular disorders: |
| Q waves suggesting myocardial infarction, or other signs of ischaemic heart disease |
| Negative T waves in V1–3 with/without epsilon waves, suggestive of arrhythmogenic right ventricular dysplasia (cardiomyopathy) |
| High amplitudes with/without ST segment depression and negative T waves in left sided precordial leads, suggestive of left ventricular hypertrophy |
| B Primary electrophysiologic abnormalities: |
| Prolonged QT interval |
| Right bundle branch block pattern with ST elevation in V1–3, suggestive of the Brugada syndrome |
| Bifascicular block* or undetermined intraventricular conduction abnormalities (QRS ≥ 0.12 s) |
| Mobitz type I second degree atrioventricular block |
| Sinus bradycardia (< 50 beats/min) or sinus pauses |
| Invasive electrophysiological testing or therapeutic actions without further delay |
| Surface ECG normal |
| A In a young person with normal physical examination, first episode: |
| Head-up tilt testing |
| If there are recurrent episodes, also: |
| Evaluation of the presence of SHD with echocardiography and stress testing |
| Holter monitoring 48 hours |
| Implantable loop recorder |
| B In a middle aged person: |
| Evaluation of the presence of SHD: |
| SHD yes: Invasive electrophysiologic study |
| Head-up tilt testing |
| Implantable loop recorder |
| SHD no: Head-up tilt testing |
| Implantable loop recorder |
| (Invasive electrophysiologic study) |
| C. In an older person: |
| Carotid sinus massage |
| Evaluation of the presence of SHD |
| Head-up tilt testing |
| Invasive electrophysiologic study |
| Implantable loop recorder |
Refer to text for discussion.
*Defined as either left bundle branch block or right bundle branch block combined with left anterior or left posterior fascicular block.
SHD, structural heart disease.
SUMMARY
Syncope accompanied by involuntary movements is not uncommon and creates a differential diagnostic problem against seizure disorders with important therapeutic and prognostic implications: the underlying cardiac condition may not receive proper treatment at a considerable mortality risk, bradycardias might be aggravated by some ion channel active antiepileptic drugs, and a diagnosis of epilepsy may lead to significant psychosocial consequences. Possible cardiovascular causes of convulsive syncope include various neurally mediated, vasovagal reactions (including carotid sinus hypersensitivity), bradycardia, and ventricular as well as supraventricular tachycardias. Besides awareness of this possibility, a careful clinical history from the patient and available witnesses, physical examination, ECG, and head-up tilt testing are the most important diagnostic tools in younger patients, while invasive electrophysiological studies with pharmacological stress testing and carotid sinus massage become more important with increasing age; echocardiography and exercise testing are additional important tools in the search for structural heart disease, which when present has the highest prognostic impact.
When should convulsive syncope or a misdiagnosis of epilepsy be suspected and a cardiovascular cause of syncope pursued?
Consider the possibility of a “vasovagal” mechanism, bradycardia, or torsade de pointe ventricular tachycardia, when sudden loss of consciousness is followed by myoclonic jerks
Consider the possibility of convulsive syncope when EEG is non-diagnostic
Consider the possibility of convulsive syncope, when antiepileptic drug treatment is inefficient in presumed epilepsy
Consider the possibility of convulsive syncope of cardiovascular cause when there are atypical premonitory symptoms (nausea, lightheadedness, palpitations)
Consider the possibility of drug induced bradycardia, when ion channel active antiepileptic treatment* is followed by an increase in attack frequency or a change in attack characteristics
*Always check a standard ECG before starting patients on such drugs
Acknowledgments
Dr Bergfeldt is a Swedish Heart-Lung Foundation Clinical Investigator.
REFERENCES
- 1.Brignole M, Alboni P, Benditt D, et al. Task force report. Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 2001;22:1256–1306. ▸ Comprehensive document covering most aspects of syncope, with emphasis on cardiovascular diseases. [DOI] [PubMed] [Google Scholar]
- 2.Chadwick D. Epilepsy. J Neurol Neusosurg Psychiatry 1994;57:264–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scheepers B, Clough P, Pickles C. The misdiagnosis of epilepsy: findings of a population study. Seizure 1998;7:403–6. [DOI] [PubMed] [Google Scholar]
- 4.Baker GA, Jacoby A, Buck D, et al. Quality of life of people with epilepsy: a European study. Epilepsia 1997;38:353–362. [DOI] [PubMed] [Google Scholar]
- 5.King MA, Newton MR, Jackson GD, et al. Epileptology of the first-seizure presentation: a clinical, electroencephalographic, and magnetic resonance imaging study of 300 consecutive patients. Lancet 1998;352:1007–11. ▸ The largest population based study of misdiagnosis of epilepsy. [DOI] [PubMed] [Google Scholar]
- 6.Smith D, Defalla BA, Chadwick DW. The misdiagnosis of epilepsy and the management of refractory epilepsy in a specialist clinic. QJM 1999;92:15–23. [DOI] [PubMed] [Google Scholar]
- 7.Lin JT-Y, Ziegler DK, Lai C-W, et al. Convulsive syncope in blood donors. Ann Neurol 1982;11:525–8. [DOI] [PubMed] [Google Scholar]
- 8.Gastaut H, Fischer-Williams M. Electro-encephalographic study of syncope. Its differentiation from epilepsy. Lancet 1957;ii:1018–25. ▸ An early account on the EEG features in syncope versus seizure disorders. [DOI] [PubMed] [Google Scholar]
- 9.Duvoisin RC. Convulsive syncope induced by the Weber maneuver. Arch Neurol 1962;7:219–26. [DOI] [PubMed] [Google Scholar]
- 10.Lempert T, Bauer M, Schmidt D. Syncope: a videometric analysis of 56 episodes of transient cerebral hypoxia. Ann Neurol 1994:36:233–7. [DOI] [PubMed] [Google Scholar]
- 11.Grossi D, Buonomo C, Mirizzi F, et al. Electroencephalographic and electrocardiographic features of vasovagal syncope induced by head-up tilt. Functional Neurology 1990;5:257–60. [PubMed] [Google Scholar]
- 12.Rossen R, Kabat H, Anderson JP. Acute arrest of cerebral circulation in man. Arch Neurol Psychiatry 1943;50:510–28. ▸ A seminal work on cerebral hypoperfusion. [Google Scholar]
- 13.Grubb BP, Gerard G, Roush K, et al. Differentiation of convulsive syncope and epilepsy with head-up tilt testing. Ann Intern Med 1991;115:871–6. [DOI] [PubMed] [Google Scholar]
- 14.Linzer M, Grubb BP, Ho S, et al. Cardiovascular causes of loss of consciousness in patients with presumed epilepsy: a cause of the increased sudden death rate in people with epilepsy ? Am J Med 1994;96:146–54. [DOI] [PubMed] [Google Scholar]
- 15.Zaidi A, Clough P, Cooper P, et al. Misdiagnosis of epilepsy: many seizure-like attacks have a cardiovascular cause. J Am Coll Cardiol 2000;36:181–4. ▸ The largest cohort study with cardiovascular approach to misdiagnosis of epilepsy. [DOI] [PubMed] [Google Scholar]
- 16.Krahn AD, Klein GJ, Yee R, et al. Randomized assessment of syncope trial: conventional diagnostic testing versus a prolonged monitoring strategy. Circulation 2001;104:46–51. ▸ The first randomised study comparing the diagnostic yield of the implantable loop recorder with that of conventional diagnostic procedures. See also accompanying editorial. [DOI] [PubMed] [Google Scholar]
- 17.Kennebäck G, Bergfeldt L, Vallin H, et al. Electrophysiologic effects and clinical hazards of carbamazepine treatment for neurologic disorders in patients with abnormalities of the cardiac conduction system. Am Heart J 1991;121:1421–9. ▸ Non-invasive and invasive electrophysiologic evaluation of the cardiac conduction system on and off carbamazepine. [DOI] [PubMed] [Google Scholar]
- 18.Keilson MJ, Hauser A, Magrill JP, et al. ECG abnormalities in patients with epilepsy. Neurology 1987;37:1624–6. ▸ The largest ambulatory electrocardiographic study during spontaneous seizures. [DOI] [PubMed] [Google Scholar]
- 19.Reeves AL, Nollet KE, Klass DW, et al. The ictal bradycardia syndrome. Epilepsia 1996;37:983–7. ▸ Important account of the “exception from the rule”, when seizures provoke significant arrhythmias. [DOI] [PubMed] [Google Scholar]
- 20.Nilsson L, Farahmand BY, Persson P-G, et al. Risk factors for sudden unexpected death in epilepsy: a case-control study. Lancet 1999;353:888–93. ▸ Recent comprehensive risk factor analysis of patients with SUDEP, sudden unexpected death in epilepsy. [DOI] [PubMed] [Google Scholar]