A55 year old man with type A aortic dissection underwent an emergency Bentall operation in 1995. Intraoperatively, he developed myocardial infarction. This resulted in progressive heart failure, eventually requiring heart transplantation in January 2002. The transplantation was successful and uncomplicated.
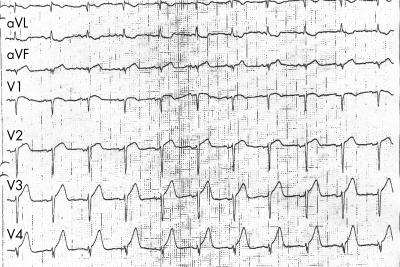
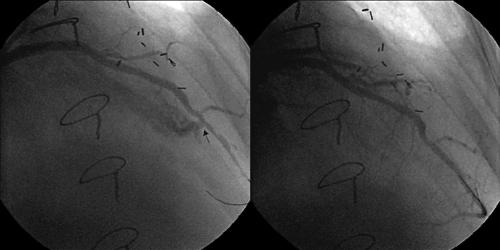
He was admitted for routine endomyocardial biopsy on 11 March 2002. A total of six biopsy fragments were removed and the patient was stable during the procedure. He experienced chest pain two hours later. A 12 lead ECG showed new onset ST segment elevation of 2 mm over the precordial leads (V2–V4) (upper panel), compatible with a diagnosis of anterior myocardial infarction. A coronary angiogram revealed the presence of a large fistula draining from the distal part of the left anterior descending coronary artery to the right ventricle (lower left panel). No significant stenosis or other abnormalities were observed elsewhere in the coronary system. A PTFE covered stent 3.0 × 12 mm (Jostent Coronary Stent Graft, Jomed, Germany) was percutaneously deployed and completely sealed off the fistula (lower right panel).
Cardiac enzymes were raised and peaked at 1549 IU/l (creatine kinase (CK) normal < 103 IU/l), 211 IU/l (CK-MB normal < 24 IU/L), and 4.24 ng/ml (troponin T). Two dimensional echocardiogram showed a newly developed apical and distal septal hypokinesia. There was no pericardial effusion. In-hospital outcome was uneventful and the patient was discharged two days later.
This case shows that an acute myocardial infarction caused by coronary steal phenomenon resulting from a coronary fistula can be a potentially serious complication during endomyocardial biopsy. Percutaneous implantation of a PTFE covered stent seems an effective treatment.