Abstract
Objective: To determine whether patients with congestive heart failure on different β adrenoreceptor blocking drugs have similar haemodynamic responses to dobutamine.
Design: Single centre, single blind, randomised, two period crossover study comparing carvedilol with metoprolol CR/XL.
Patients: Ten patients with stable chronic congestive heart failure (ejection fraction < 40%) on chronic treatment with metoprolol CR/XL.
Methods: Patients were treated with carvedilol or metoprolol CR/XL (target dose 50 mg twice daily and 200 mg once daily, respectively) for eight weeks. Stress echocardiography was undertaken at the end of each maintenance period, using dobutamine 5 and 15 μg/kg/min.
Results: No significant haemodynamic differences were seen at rest on the two treatments. There was a more pronounced increase in heart rate and cardiac output during dobutamine infusion when the patients were on metoprolol than when they were on carvedilol. Mean arterial pressure increased significantly when the patients were on carvedilol, and cardiac output increased during low dose dobutamine, without further change during high dose dobutamine. During the dobutamine infusion, there was no significant difference in ejection fraction between carvedilol and metoprolol treatment.
Conclusions: Patients with congestive heart failure on a non-selective β adrenoreceptor blocker or β1 selective blocker responded differently to the inotropic drug dobutamine: the β1 blockade caused by metoprolol could be counteracted by dobutamine, whereas with carvedilol a low dose of dobutamine increased cardiac output, and a higher dose of dobutamine caused a pressor effect. These findings may be clinically relevant when choosing an inotropic drug.
Keywords: heart failure, inotropic agents, β adrenoreceptor blocker
Large clinical trials have shown the beneficial effect of β adrenoreceptor blocking agents in patients with congestive heart failure, and these drugs are now considered to be first line treatment, together with angiotensin converting enzyme (ACE) inhibitors.1–3 Thus the number of patients with congestive heart failure receiving a β adrenoreceptor blocking agent along with other drugs is increasing. Improvements in survival are comparable with β1 selective adrenoreceptor blockers (metoprolol and bisoprolol) and non-selective blockers (carvedilol).4
Congestive heart failure is a progressive disease in which deterioration could occur as part of the natural history or as consequence of infection, other concomitant diseases, or emergency conditions requiring operation and intensive care. In these conditions temporary inotropic support may be required to counteract the effect of β blockade in order to improve cardiac performance. The most widely used inotropic drug for this purpose is dobutamine. Dobutamine is a β1 agonist acting primarily on adrenergic β1 receptors in the myocardium, and also promoting vasodilatation through both direct (β2) and secondary effects on the systemic circulation. Furthermore, dobutamine possesses α1 adrenergic activity which to some extent is offset by the β2 adrenergic vasodilatation. The net effect is an unchanged or slightly reduced systemic vascular resistance and an improvement in cardiac output.5,6
Our aim in this study was to determine whether dobutamine has similar haemodynamic effects when given to patients on chronic treatment with either a non-selective β adrenoreceptor blocker with α1 blocking properties (carvedilol) or a β1 selective adrenoreceptor blocker (metoprolol CR/XL).
METHODS
Study population
The study involved 10 patients with stable congestive heart failure who had been on chronic treatment with metoprolol for at least six months. Their mean (SEM) ejection fraction was 30 (2.4)%, their age 57 (3.4) years, and their body weight 76.3 (4.3) kg. Six patients had ischaemic heart disease (ischaemic cardiomyopathy, ICM) and four had idiopathic dilated cardiomyopathy (DCM). The patients were concomitantly taking one or more of the following prescribed drugs: ACE inhibitors (8), digoxin (3), diuretics (7). Inclusion criteria were symptomatic heart failure and a left ventricular ejection fraction of 45% or less. It was a requirement that the patients had been treated optimally for heart failure on stable doses of antifailure drugs for at least two weeks before the study.
Exclusion criteria included uncorrected primary valvar disease, restrictive or hypertrophic cardiomyopathies, symptomatic uncontrolled ventricular arrhythmias, unstable angina pectoris, active myocarditis, a heart rate less than 50 beats/min, sitting systolic blood pressure less than 85 mm Hg, and uncontrolled hypertension.
Written informed consent was obtained from each patient and the study was approved by the ethics committee of the University of Göteborg.
Study design
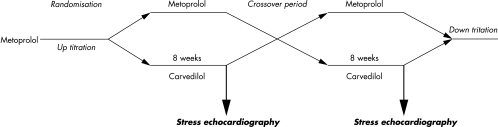
The scheme of the study design is shown in fig 1. Patients were studied using a single blind, randomised, crossover design for eight weeks on carvedilol (maximum dose 50 mg twice daily) and eight weeks on metoprolol CR/XL (maximum dose 200 mg once daily). Patients were randomly switched from their original treatment to either carvedilol or metoprolol by gradual withdrawal and uptitration. The aim of titration was to reach the highest dose at which heart rate would not differ by more than 5 beats/min from the condition at baseline. At the end of the study, the patients were gradually withdrawn from the study drug and uptitrated back to metoprolol CR/XL.
Figure 1.
Schematic presentation of the study design.
Dobutamine echocardiography
A complete Doppler and cross sectional echocardiographic examination was done with the patient in the left lateral position after each study period at rest, using an Acuson XP 128 instrument with a 4V2C transducer (Acuson, Mountain View, California, USA). Parasternal long and short axis views, together with apical two, four, and long axis chamber views, were obtained. Dobutamine was infused intravenously, starting at 5 μg/kg/min and increasing by 5 μg/kg/min increments at 10 minute intervals up to 15 μg/kg/min or less if the heart rate increased by more than 20 beats/min from the resting state. ECG and blood pressure were monitored continuously. Echocardiographic recordings were evaluated off-line by an investigator who was blinded to clinical data. Left ventricular volumes and ejection fraction were calculated using the biplane Simpson formula.7 Left ventricular volumes were used to calculate stroke volume and cardiac output. Total peripheral resistance was calculated as mean arterial pressure divided by cardiac output and expressed as resistance units.
Statistical analysis
Haemodynamic and echocardiographic variables were analysed by a two sample t test for crossover analysis. If the analysis of residuals rejected the assumption of normality for any variable, this variable was analysed using the Wilcoxon rank-sum test. Carryover effects were analysed.
Changes in variables from rest to dobutamine infusion were compared using a paired t test. A probability value pf p < 0.05 was considered significant. All data are expressed as mean (SEM).
RESULTS
The mean doses during the maintenance phases were 85 (7) mg/day for carvedilol and 160 (16) mg/day for metoprolol CR/XL. Eight weeks of treatment with carvedilol or metoprolol did not change any of the investigated variables compared with baseline (table 1). There was no carryover effect.
Table 1.
Haemodynamic variables at rest and during dobutamine infusion
| Carvedilol, 85 (7.6) mg/day | Metoprolol CR/XL, 160 (16) mg/day | |||||
| Variable | At rest | Dobutamine (5 μg/kg/min) | Dobutamine (15 μg/kg/min) | At rest | Dobutamine (5 μg/kg/min) | Dobutamine (15 μg/kg/min) |
| HR (beats/min) | 57 (2.4) | 57 (3.2) | 56 (2.8) | 57 (2.6) | 60 (3.9) | 76 (5.7)*† |
| SBP (mm Hg) | 122 (6.4) | 132 (8.1)* | 168 (10.3)*† | 123 (6.9) | 128 (7.2) | 130 (6.9) |
| DBP (mm Hg) | 77 (2.1) | 82 (2.2) | 89 (2.6)*† | 78 (3.1) | 78 (2.1) | 77 (2.6) |
| MAP (mm Hg) | 92 (2.5) | 100 (3.1)* | 115 (4.0)*† | 93 (3.7) | 95 (3.4) | 95 (3.8) |
| EF (%) | 31 (3.4) | 35 (3.6) | 36 (3.6) | 31 (2.2) | 35 (2.6) | 35 (2.7) |
| SV (ml) | 58 (4.6) | 72 (6.1)* | 69 (6.2)* | 61 (4.6) | 66 (5.4) | 68 (5.1)* |
| CO (l/min) | 3.4 (0.3) | 4.2 (0.4)* | 3.9 (0.4)* | 3.4 (0.4) | 3.9 (0.5)(p=0.059) | 5.1 (0.4)*† |
| TPR (RU) | 29 (2.2) | 26 (3.4) | 31 (2.5) | 29 (3.7) | 27 (3.1) | 19 (1.7)*† |
Values are mean (SEM).
*p < 0.05 v rest; †p < 0.05 v values during infusion of 5 μg/kg/min dobutamine.
CO, cardiac output; DBP, diastolic blood pressure; EF, ejection fraction; HR, heart rate; MAP, mean arterial pressure; RU, resistance units; SBP, systolic blood pressure; SV, stroke volume; TPR, total peripheral resistance.
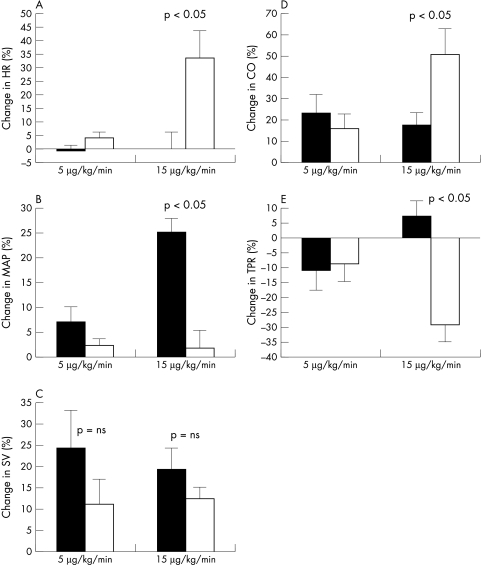
There was a significant difference in the response to dobutamine infusion on the two treatments (fig 2, table 1). After eight weeks of carvedilol treatment, infusion of dobutamine was associated with no change in heart rate or total peripheral resistance, but there was an increase in arterial pressure. After metoprolol treatment, heart rate increased significantly and total peripheral resistance declined, with no change in arterial pressure (fig 2). On carvedilol, stroke volume and cardiac output increased during low dose dobutamine infusion (5 μg/kg/min) from 3.4 (0.3) to 4.2 (0.4) l/min; during high dose dobutamine there was a tendency for cardiac output to decrease. On metoprolol treatment, on the other hand, stroke volume and cardiac output increased significantly during high dose dobutamine infusion. A slight but non-significant increase in ejection fraction was observed during dobutamine infusion on both treatments.
Figure 2.
Effect of dobutamine infusion on (A) heart rate (HR), (B) mean arterial pressure (MAP), (C) stroke volume (SV), (D) cardiac output (CO), and (E) total peripheral resistance (TPR). Data are percentage change from rest (mean and SEM). Filled bars, carvedilol; empty bars, metoprolol; p values between columns refer to the significance of differences between treatments.
Though the number of patients was too low for reliable statistics, the response to dobutamine was assessed in relation to the aetiology of the heart failure. At rest the ICM patients tended to be in a less satisfactory haemodynamic state than the DCM patients, with a lower stroke volume and cardiac output. The response to low dose dobutamine was similar to that for the whole group. However, during high dose dobutamine, the difference between carvedilol and metoprolol appeared to be accentuated. During the 15 μg/kg/min dobutamine infusion in the ICM patients, cardiac output increased from 2.9 (0.2) to 3.3 (0.2) l/min on carvedilol, and from 3.1 (0.4) to 4.5 (0.2) l/min on metoprolol. In the DCM group, the equivalent values were 3.8 (0.6) to 5.0 (0.6) l/min (carvedilol), and 3.9 (0.8) to 6.2 (1.1) l/min (metoprolol).
DISCUSSION
We found significant differences in the response to dobutamine depending on the type of β adrenoreceptor blocker maintenance treatment. During carvedilol treatment, dobutamine infusion did not alter the heart rate, slightly increasing cardiac output while mean arterial pressure increased significantly. During metoprolol treatment, the patients responded with an increase in heart rate and cardiac output while mean arterial pressure was unchanged.
In the absence of a β adrenergic blocking drug, dobutamine increases the cardiac output, with an equal or greater net effect on β2 adrenergic vasodilatation compared with α adrenergic vasoconstriction.6 The decrease in total peripheral resistance observed during dobutamine infusion reflects both a reflex withdrawal of sympathetic tone secondary to an increase in cardiac output6 and direct β2 adrenoreceptor mediated vasodilatation. Experiments in conscious dogs have shown that propanolol abolishes the inotropic effects of dobutamine and unmasks the α adrenergic receptor effect of this drug.8 A similar response to dobutamine, with an increment in total peripheral resistance, has been reported previously in patients without congestive heart failure being treated with β adrenoreceptor blockers.9
The different responses to dobutamine observed in our study are probably related to the specific properties of carvedilol and metoprolol and their effects on β adrenergic receptors. Metoprolol is approximately 75-fold selective for β1 over β2 receptors. Carvedilol is a non-selective β adrenoreceptor blocker with α1 adrenergic blocking properties.10 The ratio of α1 to β adrenoreceptor blockade for carvedilol is 1:10.11 It is known that carvedilol is a moderate vasodilator when given acutely, but during long term treatment the vasodilator activity is less prominent.12 Metoprolol treatment is thought to be associated with upregulation of the β1 adrenoreceptors that are downregulated in the failing heart,13 whereas carvedilol does not cause such upregulation.12 This difference in receptor sensitivity might be one explanation for the different heart rate response during dobutamine infusion that we observed in our study. It is also possible that the increase in heart rate is partly a β2 effect, which is more profoundly blocked by carvedilol. Finally, the increase in blood pressure could mediate a negative feedback and increased vagal tone, attenuating the increase in heart rate during carvedilol treatment. On the other hand, when carvedilol is given in low dosage, a decrease in blood pressure has been reported during dobutamine infusion, explained by a greater degree of α1 than β2 blockade by carvedilol.14
During carvedilol treatment, the rise in cardiac output with low dose dobutamine was achieved mainly by an increase in stroke volume, while the higher dose of dobutamine did not increase cardiac output or stroke volume further. At the higher dose, dobutamine increased arterial pressure, probably through its peripheral effects. This significant rise in afterload could explain why we did not observe any further increase in cardiac output during carvedilol treatment. With metoprolol treatment, dobutamine caused a gradual increase in cardiac output, mainly by an increase in heart rate. The rise in cardiac output was accompanied by a significant fall in peripheral resistance. In a recently published study, a different response to dobutamine was observed with the two β blockers.15 There were, however, significant differences between that study and ours with regard to study design and the dose of dobutamine. We studied the response to a low to moderate dose of dobutamine, aiming at doses that would be needed for inotropic support in patients with congestive heart failure, and we did not intend to provoke ischaemia. Moreover, it appeared that we used higher doses of both the β blockers. Nevertheless, both these studies underline the variation in response to a widely used inotropic drug in the presence of metoprolol of carvedilol. Our measurements of cardiac output and total peripheral resistance were calculated by non-invasive methods. Preliminary findings from a study using invasive techniques were similar to ours in patients with congestive heart failure receiving carvedilol or metoprolol.16
Our results have clinical implications for the use of inotropic agents in patients with congestive heart failure who are receiving β adrenoreceptor blocking drugs. Our study was done on patients in a stable condition and none was in urgent need of inotropic support. In our study patients with ischaemic cardiomyopathy had a lower stroke volume and cardiac output and responded poorly to dobutamine, though the response was clearly better when they were on treatment with metoprolol than on carvedilol. One might therefore speculate that patients with more severe heart failure would experience even more pronounced differences in their response to dobutamine. An alternative might be to use inotropic drugs with different cellular pathways, such as a phosphodiesterase inhibitor or a calcium sensitiser.
Conclusions
Patients with congestive heart failure on a non-selective β adrenoreceptor blocker or a β1 selective blocker responded differently to the inotropic drug dobutamine. These findings could be clinically relevant when choosing an inotropic drug for such patients: the β1 blockade caused by metoprolol may be counteracted by dobutamine, whereas in patients on carvedilol a low dose of dobutamine could be used to increase cardiac output when required, or a high dose of dobutamine when the pressor effect of dobutamine is needed.
Acknowledgments
This work was supported by Roche AB, Cardiovascular Unit, Stockholm, Sweden.
Abbreviations
ACE, angiotension converting enzyme
DCM, dilated cardiomyopathy
ICM, ischaemic cardiomyopathy
REFERENCES
- 1.Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. US carvedilol heart failure study group. N Engl J Med 1996;334:1349–55. [DOI] [PubMed] [Google Scholar]
- 2.Trial Participants. The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomised trial. Lancet 1999;353:9–13. [PubMed] [Google Scholar]
- 3.Trial Participants. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 1999;353:2001–7. [PubMed] [Google Scholar]
- 4.Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651–8. [DOI] [PubMed] [Google Scholar]
- 5.Ruffolo RR. The pharmacology of dobutamine. Am J Med Sci 1987;294:244–8. [DOI] [PubMed] [Google Scholar]
- 6.Sonnenblick EH, Frishman WH, LeJemtel TH. Dobutamine: a new synthetic cardioactive sympathetic amine. N Engl J Med 1979;300:17–22. [DOI] [PubMed] [Google Scholar]
- 7.Schiller NB. Two-dimensional echocardiographic determination of left ventricular volume, systolic function, and mass. Summary and discussion of the 1989 recommendations of the American Society of Echocardiography. Circulation 1991;84(suppl 3):I280–7. [PubMed] [Google Scholar]
- 8.Vatner SF, McRitchie RJ, Braunwald E. Effects of dobutamine on left ventricular performance, coronary dynamics, and distribution of cardiac output in conscious dogs. J Clin Invest 1974;53:1265–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tarnow J, Komar K. Altered hemodynamic response to dobutamine in relation to the degree of preoperative beta-adrenoceptor blockade. Anesthesiology 1988;68:912–19. [DOI] [PubMed] [Google Scholar]
- 10.Bristow MR. Beta-adrenergic receptor blockade in chronic heart failure. Circulation 2000;101:558–69. [DOI] [PubMed] [Google Scholar]
- 11.Frishman WH. Carvedilol. N Engl J Med 1998;339:1759–65. [DOI] [PubMed] [Google Scholar]
- 12.Gilbert EM, Abraham WT, Olsen S, et al. Comparative hemodynamic, left ventricular functional, and antiadrenergic effects of chronic treatment with metoprolol versus carvedilol in the failing heart. Circulation 1996;94:2817–25. [DOI] [PubMed] [Google Scholar]
- 13.Bristow MR, Ginsburg R, Umans V, et al. Beta 1- and beta 2-adrenergic-receptor subpopulations in nonfailing and failing human ventricular myocardium: coupling of both receptor subtypes to muscle contraction and selective beta 1-receptor down-regulation in heart failure. Circ Res 1986;59:297–309. [DOI] [PubMed] [Google Scholar]
- 14.Lindenfeld J, Lowes BD, Bristow MR. Hypotension with dobutamine: beta-adrenergic antagonist selectivity at low doses of carvedilol. Ann Pharmacother 1999;33:1266–9. [DOI] [PubMed] [Google Scholar]
- 15.Maack C, Elter T, Nickenig G, et al. Prospective crossover comparison of carvedilol and metoprolol in patients with chronic heart failure. J Am Coll Cardiol 2001;38:939–46. [DOI] [PubMed] [Google Scholar]
- 16.Metra M, Nodari S, Boldi E, et al. Differential effects of intravenous inotropes in patients on long-term beta-blocker therapy [abstract]. Eur Heart J 2000;21(suppl: August/September):298. [Google Scholar]