Abstract
Objective: To determine whether the plasma concentration of the putative new cardiac hormone relaxin is predictive of clinical outcome in patients with chronic heart failure (CHF).
Design: Plasma relaxin and N-terminal pro B type natriuretic peptide (NT pro BNP) concentrations were measured in 87 patients admitted in an emergency with CHF caused by left ventricular systolic dysfunction. These were related to death and death or readmission with CHF over the following year.
Setting: Western Infirmary, Glasgow, UK.
Main outcome measures: Plasma concentrations of relaxin and NT pro BNP; time to death or hospitalisation caused by heart failure.
Results: Plasma concentrations of both relaxin and NT pro BNP were greatly increased. Of the 43 patients with NT pro BNP above the group median concentration, 23 (53%) died and 30 (70%) died or were hospitalised with CHF. Among the 44 with concentrations below the median, these numbers were 5 (11%) and 12 (27%), respectively (p < 0.0001 and p < 0.0001, respectively). Plasma NT pro BNP concentration remained an independent predictor of an adverse clinical outcome in a multivariate analysis. Of the 42 patients with a relaxin concentration above the median, 13 (31%) died and 20 (48%) died or were hospitalised. Below the median, these numbers were 15 of 45 (33%) and 22 of 45 (49%) (p = 0.76 and p = 0.84, respectively).
Conclusions: NT pro BNP is a powerful and independent predictor of outcome in CHF, whereas relaxin, also secreted by the heart in increased amounts in CHF, is not.
Keywords: natriuretic peptides, relaxin, heart failure, prognosis, survival, hospital admission
Relaxin is a polypeptide hormone belonging to the insulin family.1–3 Though known for many years as a hormone of parturition, relaxin has lately been shown to be a powerful systemic arterial vasodilator released from the heart.1,4,5 One recent study reported increased cardiac relaxin release and increased plasma relaxin concentrations in heart failure.4 Consequently, it has been postulated that relaxin, like the natriuretic peptides, may be secreted as a compensatory neuroendocrine response in heart failure.4,5 With other pathophysiologically important neurohumoral mediators there is a clear relation to outcome in heart failure, whereby higher plasma concentrations, indicating greater neurohumoral activation, are associated with a worse prognosis.6–8 Consequently, we have examined the relation between plasma relaxin concentration and clinical events in patients with chronic heart failure (CHF). As a “positive control”, we also examined the prognostic importance of N-terminal pro B type natriuretic peptide (NT pro BNP) in the same patients.9
METHODS
Patients
Patients taking part in a randomised controlled trial of specialist nurse intervention were studied. This trial has been described in detail elsewhere.10 Briefly, patients admitted to hospital, on an emergency basis, with heart failure caused by left ventricular systolic dysfunction were enrolled in a trial comparing conventional care with conventional care supplemented by specialist heart failure nurse intervention. Patients were followed up for a mean of 12 months after randomisation. Deaths and hospital readmissions were recorded. Readmissions were adjudicated by a blinded end point committee. The primary end point was death or readmission with heart failure. Patients consented to have venous blood collected for measurement of neurohumoral factors.
Assays
NT pro BNP was measured in blood samples taken just before discharge by using a validated and commercially available immunoassay (Roche Diagnostics, Mannheim, Germany).11 Plasma relaxin was determined with the use of an enzyme linked immunosorbent assay (ELISA) kit (Immundiagnostik, Bensheim, Germany), as reported previously.4
Statistical analysis
Event rates were compared for patients with plasma concentrations of NT pro BNP and relaxin above and below the group median. As NT pro BNP concentrations above the median were associated with a significantly worse clinical outcome, multivariate analyses were carried out to determine whether NT pro BNP was an independent predictor of outcome (death and death or hospital admission for CHF). Firstly, a univariate analysis was performed using all relevant baseline data (for example, age, sex, New York Heart Association functional class, left ventricular function, heart rhythm, comorbidity, history of prior CHF hospitalisation, creatinine). Variables significantly (p < 0.05) associated with outcome were then examined in a stepwise multivariate analysis.
RESULTS
Of the 165 patients randomly assigned in the study, plasma NT pro BNP and relaxin concentrations were available for 87. Table 1 gives details of these patients.
Table 1.
Characteristics of patients studied
| Number of patients | 87 |
| Age (years) (range) | 75 (51–93) |
| Sex (male/female) | 51/36 |
| Current angina | 38 |
| Previous myocardial infarction | 40 |
| Diabetes | 13 |
| Chronic obstructive pulmonary disease | 24 |
| Atrial fibrillation | 25 |
| β Blocker | 9 |
| Angiotensin converting enzyme inhibitor | 37 |
| Diuretic | 60 |
| HMG CoA reductase inhibitor | 2 |
| Calcium channel blocker | 20 |
| Digoxin | 17 |
| Nitrate | 12 |
| Aspirin | 43 |
| Warfarin | 9 |
| Admission New York Heart Association class | |
| II | 21 |
| III | 28 |
| IV | 38 |
| Creatinine (μmol/l) | *132 (7.2) |
HMG CoA, 3-hydroxy-3-methylglutaryl coenzyme A.
*Mean (SD)
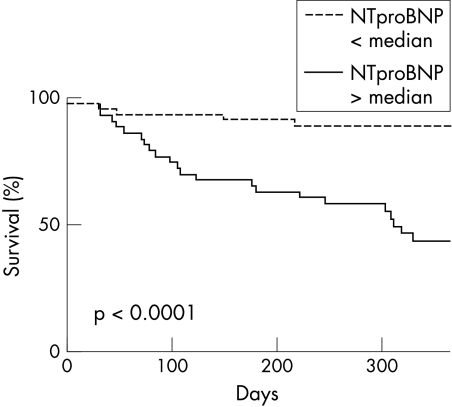
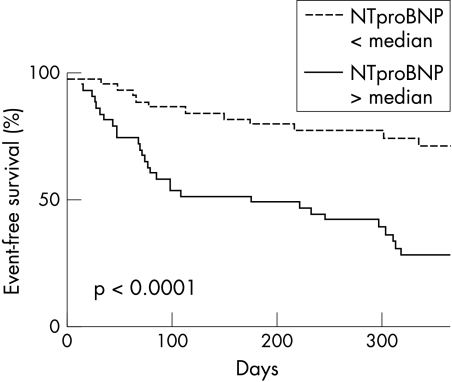
The median (range) plasma NT pro BNP concentration was much increased at 2994 (134–35 000) pg/ml compared with normal (< 334 pg/ml for female and < 227 pg/ml for male patients). Plasma NT pro BNP was a predictor both of death and of heart failure hospitalisation or death (figs 1 and 2). Of patients with NT pro BNP above the median concentration (n = 43), 23(53%) died and 30 (70%) died or were hospitalised with CHF. For those with NT pro BNP concentrations below the median (n = 44), these proportions were 5 (11%) and 12 (27%) (p < 0.0001 for death and p < 0.0001 for death or CHF hospitalisation).
Figure 1.
Time to death in patients with plasma N-terminal pro B type natriuretic peptide (NT pro BNP) concentrations above and below the median.
Figure 2.
Time to death or hospital admission for heart failure in patients with plasma NT pro BNP concentrations above and below the median.
In the multivariate analysis, plasma NT pro BNP concentration was a significant, independent predictor of death or CHF hospitalisation (odds ratio 4.15, p = 0.003) and of death alone (odds ratio 2.22, p = 0.03).
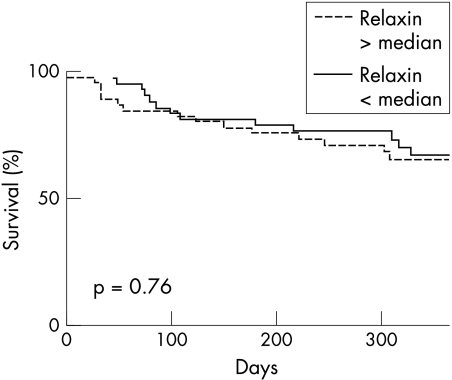
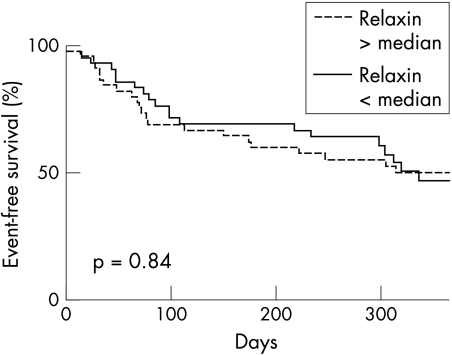
The median (range) plasma relaxin concentration was also greatly increased at 89 (11–644) pg/ml compared with normal (< 2 pg/ml). However, in contrast to NT pro BNP, there was no relation between relaxin and outcome (figs 3 and 4). Of those patients with a relaxin concentration above the median (n = 42), 13 (31%) died and 20 (48%) died or were hospitalised. These proportions for patients with a plasma relaxin concentration below the median (n = 45) were 15 (33%) and 22 (49%) (p = 0.76 for death and p = 0.84 for death or CHF hospitalisation). Plasma relaxin concentration was not a significant predictor of outcome in the univariate analysis.
Figure 3.
Time to death in patients with plasma relaxin concentrations above and below the median.
Figure 4.
Time to death or hospital admission for heart failure in patients with plasma relaxin concentrations above and below the median.
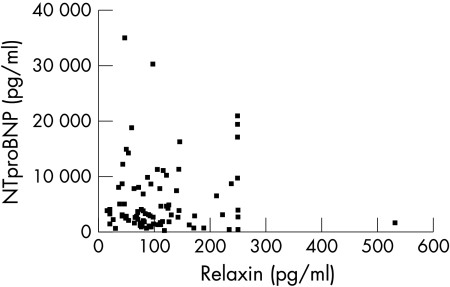
There was no correlation between plasma concentrations of relaxin and those of NT pro BNP (fig 5).
Figure 5.
Correlation plot for NT pro BNP and relaxin concentrations.
DISCUSSION
Our study confirms that heart failure caused by left ventricular systolic dysfunction is associated with a large increase in the plasma concentration of the two new neurohumoral markers NT pro BNP and relaxin. As yet, there are very few reports of plasma NT pro BNP concentrations in heart failure11–16 and only one other describing relaxin concentrations.4
In the present study NT pro BNP was also predictive of both death and death or readmission with worsening CHF. Though the predictive value of other natriuretic peptides in CHF has been extensively reported, we know of only one other study describing the prognostic importance of NT pro BNP in CHF.15,17–22 In a substudy of the Australia-New Zealand carvedilol trial, Richards and colleagues15 found that NT pro BNP was a strong predictor of all cause mortality, as well as admission to hospital with CHF. In that study, NT pro BNP had more predictive power for these outcomes than left ventricular ejection fraction. We also found NT pro BNP to be an independent predictor of adverse clinical outcome. Consequently, there are now two studies confirming that this very stable peptide,23,24 which is easy to assay,13,23,24 has prognostic as well as diagnostic value in CHF. NT pro BNP also gives prognostic information after myocardial infarction and in acute coronary syndromes.25,26
Dschietzig and colleagues4 have recently shown that cardiac relaxin production and plasma relaxin concentrations are increased in CHF; the latter finding was confirmed in the present study. As relaxin is a powerful vasodilator secreted by the heart,5 our hypothesis was that, like the natriuretic peptides, plasma concentrations may be related to prognosis. We were not able to confirm this.
Though plasma concentrations of most neurohumoral factors are predictive of outcome, not all are (for example, arginine vasopressin).27 We found no correlation between plasma NT pro BNP and relaxin concentrations, suggesting different release mechanisms. The atria may be a more important source of relaxin than the ventricles, whereas the opposite is true for NT pro BNP.4,28 As a biochemical marker of left ventricular dilatation and wall stress, NT pro BNP, perhaps not surprisingly, is therefore a powerful prognostic factor.15 Furthermore, net cardiac relaxin release is not pronounced except in moderate to severe CHF and even then is not always observed.4 These reasons may explain why relaxin was not predictive of outcome. However, it remains possible that relaxin does have some weak predictive effect that was not observed because of the modest size of our study.
In summary, even though relaxin has been shown to be a potent vasodilator released by the failing heart, it is not a powerful prognostic indicator in CHF.
Acknowledgments
This study was supported by the British Heart Foundation.
Abbreviations
CHF, chronic heart failure
ELISA, enzyme linked immunosorbent assay
NT pro BNP, N-terminal pro B type natriuretic peptide
REFERENCES
- 1.Bani D. Relaxin: a pleiotropic hormone. Gen Pharmacol 1997;28:13–22. [DOI] [PubMed] [Google Scholar]
- 2.Hsu SY, Nakabayashi K, Nishi S, et al. Activation of orphan receptors by the hormone relaxin. Science 2002;295:671–4. [DOI] [PubMed] [Google Scholar]
- 3.Ivell R, Einspanier A. Relaxin peptides are new global players. Trends Endocrinol Metab 2002;13:343. [DOI] [PubMed] [Google Scholar]
- 4.Dschietzig T, Richter C, Bartsch C, et al. The pregnancy hormone relaxin is a player in human heart failure. FASEB J 2001;15:2187–95. [DOI] [PubMed] [Google Scholar]
- 5.Fisher C, MacLean M, Morecroft I, et al. Is the pregnancy hormone relaxin also a vasodilator peptide secreted by the heart? Circulation 2002;106:292–5. [DOI] [PubMed] [Google Scholar]
- 6.Francis GS, Goldsmith SR, Levine TD, et al. The neurohumoral axis in congestive heart failure. Ann Intern Med 1984;101:370–7. [DOI] [PubMed] [Google Scholar]
- 7.Cohn JN, Levine TB, Olivari MT, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 1984;311:819–23. [DOI] [PubMed] [Google Scholar]
- 8.Swedberg K, Eneroth P, Kjekshus J, et al. Hormones regulating cardiovascular function in patients with severe congestive heart failure and their relation to mortality. CONSENSUS Trial Study Group. Circulation 1990;82:1730–6. [DOI] [PubMed] [Google Scholar]
- 9.Hunt PJ, Yandle TG, Nicholls MG, et al. The amino-terminal portion of pro-brain natriuretic peptide (Pro-BNP) circulates in human plasma. Biochem Biophys Res Commun 1995;214:1175–83. [DOI] [PubMed] [Google Scholar]
- 10.Blue L, Lang E, McMurray JJ, et al. Randomised controlled trial of specialist nurse intervention in heart failure. BMJ 2001;323:715–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hobbs FD, Davis RC, Roalfe AK, et al. Reliability of N-terminal pro-brain natriuretic peptide assay in diagnosis of heart failure: cohort study in representative and high risk community populations. BMJ 2002;324:1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Masson S, Vago T, Baldi G, et al. Comparative measurement of N-terminal pro-brain natriuretic peptide and brain natriuretic peptide in ambulatory patients with heart failure. Clin Chem Lab Med 2002;40:761–3. [DOI] [PubMed] [Google Scholar]
- 13.Hunt PJ, Richards AM, Nicholls MG, et al. Immunoreactive amino-terminal pro-brain natriuretic peptide (NT-PRO BNP): a new marker of cardiac impairment. Clin Endocrinol 1997;47:287–96. [DOI] [PubMed] [Google Scholar]
- 14.Talwar S, Squire IB, Davies JE, et al. Plasma N-terminal pro-brain natriuretic peptide and the ECG in the assessment of left-ventricular systolic dysfunction in a high risk population. Eur Heart J 1999;20:1736–44. [DOI] [PubMed] [Google Scholar]
- 15.Richards AM, Doughty R, Nicholls MG, et al. Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin: prognostic utility and prediction of benefit from carvedilol in chronic ischaemic left ventricular dysfunction. Australia-New Zealand Heart Failure Group. J Am Coll Cardiol 2001;37:1781–7. [DOI] [PubMed] [Google Scholar]
- 16.Groenning BA, Nilsson JC, Sondergaard L, et al. Detectionof left ventricular enlargement and impaired systolic function with plasma N-terminal pro brain natriuretic peptide concentrations. Am Heart J 2002;143:923–9. [DOI] [PubMed] [Google Scholar]
- 17.Hall C, Kjekshus J, Eneroth P, et al. The plasma concentration of N-terminal proatrial natriuretic factor ANF(1–98) is related to prognosis in severe heart failure. Clin Cardiol 1994;17:191–5. [DOI] [PubMed] [Google Scholar]
- 18.Eriksson SV, Caidahl K, Hall C, et al. Atrial natriuretic peptide ANP (1–98) and ANP (99–126) in patients with severe chronic congestive heart failure: relation to echocardiographic measurement. A subgroup analysis from the cooperative north Scandinavian enalapril survival study (CONSENSUS). J Card Fail1995;1:109–16. [DOI] [PubMed] [Google Scholar]
- 19.Dickstein K, Aarsland T, Hall C. Plasma N-terminal atrial natriuretic factor: a predictor of survival in patients with congestive heart failure. J Card Fail 1997;3:83–9. [DOI] [PubMed] [Google Scholar]
- 20.Selvais PL, Robert A, Ahn S, et al. Direct comparison between endothelin-1, N-terminal proatrial natriuretic factor, and brain natriuretic peptide as prognostic markers of survival in congestive heart failure. J Card Fail 2000;6:201–7. [DOI] [PubMed] [Google Scholar]
- 21.McDonagh TA, Cunningham AD, Morrison CE, et al. Left ventricular dysfunction, natriuretic peptides, and mortality in an urban population. Heart 2001;86:21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bettencourt P, Ferreira S, Azevedo A, et al. Preliminary data on the potential usefulness of B-type natriuretic peptide levels in predicting outcome after hospital discharge in patients with heart failure. Am J Med 2002;113;215–9. [DOI] [PubMed] [Google Scholar]
- 23.Hughes D, Talwar S, Squire IB, et al. An immunoluminometric assay for N-terminal pro-brain natriuretic peptide: development of a test for left ventricular dysfunction. Clin Sci 1999;96:373–80. [PubMed] [Google Scholar]
- 24.Downie PF, Talwar S, Squire IB, et al. Assessment of the stability of N-terminal pro-brain natriuretic peptide in vitro: implications for assessment of left ventricular dysfunction. Clin Sci 1999;97:255–8. [PubMed] [Google Scholar]
- 25.Richards AM, Nicholls MG, Yandle TG, et al. Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin: new neurohormonal predictors of left ventricular function and prognosis after myocardial infarction. Circulation 1998;97:1921–9. [DOI] [PubMed] [Google Scholar]
- 26.Omland T, de Lemos JA, Morrow DA, et al. Prognostic value of N-terminal pro-atrial and pro-brain natriuretic peptide in patients with acute coronary syndromes. Am J Cardiol 2002;89:463–5. [DOI] [PubMed] [Google Scholar]
- 27.Richards AM, Doughty R, Nicholls MG, et al. Neurohumoral prediction of benefit from carvedilol in ischaemic left ventricular dysfunction. Australia-New Zealand Heart Failure Group. Circulation 1999;99:786–92. [DOI] [PubMed] [Google Scholar]
- 28.Taylor MJ, Clark CL. Evidence for a novel source of relaxin: atrial cardiocytes. J Endocrinol 1994;143:R5–8. [DOI] [PubMed] [Google Scholar]